Abstract
Introduction
The COVID‐19 pandemic caused an unprecedented impact to haemophilia healthcare delivery. In particular, rapid implementation of telehealth solutions was required to ensure continued access to comprehensive care.
Aims
To explore patient and healthcare provider (HCP) experience of telehealth in a European Haemophilia Comprehensive Care Centre.
Method
A systematic evaluation was performed to survey patient and HCP experience and compare clinical activity levels with telehealth to in‐person attendances.
Results
Public health measures implemented in March 2020 to reduce COVID‐19 spread resulted in a 63% decrease in medical/nursing clinic consultation activity compared to the same period in 2019. Implementation of digital care pathways resulted in marked increase in activity (52% greater than 2019). Importantly, enhanced patient engagement was noted, with a 60% reduction in non‐attendance rates. Survey of patients who had participated in medical/nursing teleconsultations demonstrated that teleconsultations improved access (79%), reduced inconvenience (82%), was easy to use (94%) and facilitated good communication with the HCP (97%). A survey exploring the telemedicine experience of HCPs, illustrated that HCPs were satisfied with teleconsultation and the majority (79%) would like to continue to offer teleconsultation as part of routine patient care. In addition to medical/nursing reviews, continued access to physiotherapy with virtual exercise classes for people with haemophilia and teleconsultation for acute dental issues was equally successful.
Conclusion
During an unprecedented public health emergency, telehealth has enabled continued access to specialized haemophilia comprehensive care. Our novel findings show that this alternative is acceptable to both patients and HCPs and offers future novel opportunities.
Keywords: COVID‐19, haemophilia, teledentistry, telehealth, telemedicine
1. INTRODUCTION
The COVID‐19 pandemic has changed the way medicine is practised. In particular, haemophilia comprehensive care centres across the world have been forced to find innovative ways to provide healthcare access and high‐quality specialized care to the bleeding disorder community despite current challenges. 1 Telemedicine (TM) (or telehealth), is defined by the National Institute of Health (NIH) as the use of technology to provide and support healthcare at a distance 2 (Figure 1). Traditional medicine has been slow to embrace telehealth as a routine tool in the delivery of healthcare, partly due to resistance to change and partly due to reported limitations of remote consultation. Barriers to the use of telehealth include concern regarding the patient‐physician relationship, legal issues such as privacy and data concerns, as well as social issues such as variable digital access and familiarity with telecommunications technologies. In some jurisdictions reimbursement and cost are also a concern. 3
Figure 1.
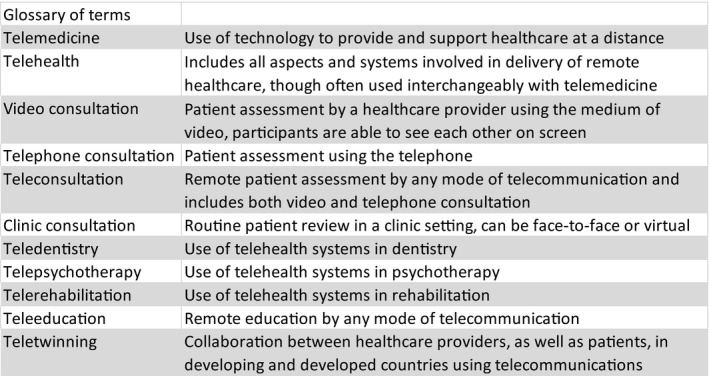
Glossary of terms
Prior to the COVID‐19 pandemic, telehealth had been identified as having a potentially important role in the delivery of comprehensive care for people with haemophilia and inherited bleeding disorders, including virtual TM clinics, telephysical therapy and rehabilitation. 4 Critically, however, limited data have been collected regarding the use of TM in haemophilia comprehensive care. The role of TM in perioperative management and rehabilitation following orthopaedic surgery in a patient with severe haemophilia was recently reported. 5 TM can facilitate early and appropriate treatment in the setting of an acute bleed. Video consultations in children with haemophilia with acute complications 6 allowed care to be delivered more conveniently and did not adversely affect the quality of the patient‐physician relationship. Substantial cost savings for patients with haemophilia and related bleeding disorders who attended clinics locally and received speciality care remotely using TM have been reported. 7
The Irish National Haemophilia Service has been an advocate for telehealth delivery of care to people with haemophilia. A National Electronic Health Record (EHR) for haemophilia and inherited bleeding disorders has been in place since 2006, and upgraded in 2019 to a fully cloud‐based EHR. 8 Haemophilia treatments are also managed electronically using a track and trace solution and a scanning smartphone App, documenting supply and utilization. A bidirectional patient portal to enable direct access to patient healthcare information and to the Haemophilia Treatment Centre is being implemented currently.
The COVID‐19 pandemic resulted in an unprecedented upheaval to healthcare delivery requiring a rapid response to replace the traditional care model with innovative telehealth solutions to maintain access and services to a patient cohort with varied health needs. In this paper, we discuss the Irish patient and healthcare provider (HCP) experience of telehealth which was implemented rapidly to ensure continuity of specialist haemophilia comprehensive care during the COVID‐19 pandemic.
2. METHODS
A multidisciplinary service evaluation was undertaken to survey patient and HCP experience of telehealth as implemented in a European Haemophilia Comprehensive Care Centre (EHCCC) and to compare telehealth clinical activity levels to in‐person attendances during the same time period in 2019.
All HCPs in the EHCCC, including physicians, nurses, physiotherapists, dentist, psychologist and social worker, adopted telehealth (Figure 2), to ensure continued healthcare access for patients. Telephone consultations were carried out using a combination of speaker phones and headsets. Blue Eye (RedZinc Services Limited, Guinness Enterprise Centre, Taylor's Lane, Dublin 8, Ireland), a video communications system which connects patient's smartphone to the HCP on a web‐based platform via a secure SMS or email link, was used for video consultations. Verbal consent was obtained from all patients prior to commencing teleconsultation.
Figure 2.
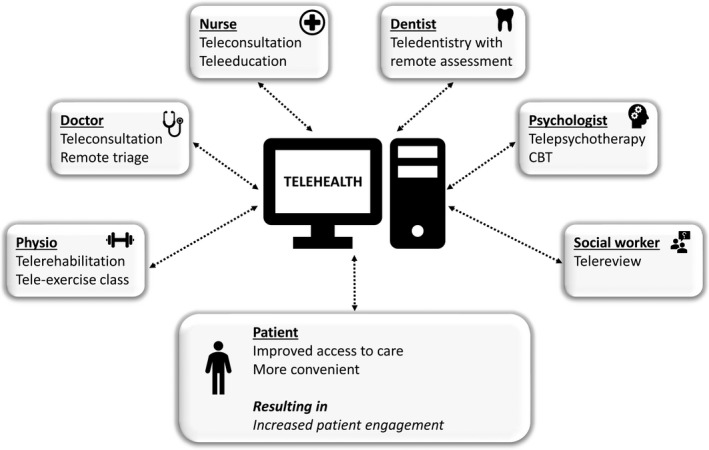
Diagram illustrating the telehealth care model for delivery of patient care
Subsequently, two patient surveys were carried out. Firstly, an anonymized, patient experience survey (5‐point Likert scale) was posted to patients who had a medical telehealth consultation between 11th March and 30th April 2020. All patients who had a video consultation and a random sample (every third patient), who had a telephone consultation received a survey. The patients were new and return patients and included patients with bleeding and thrombosis disorders, reflecting the diversity of patients seen by the EHCCC. Qualitative and quantitative analysis of themes was undertaken. A second, anonymized, patient postal survey was carried out, evaluating the physiotherapy service provided to people with severe haemophilia (PWSH). Part of this survey explored the specific experience of telehealth for PWSH.
HCPs were surveyed using a 10‐question anonymous online survey to assess their early experience of the introduction of telehealth in a large national comprehensive care centre. Personal feedback was also sought from the medical social worker and the clinical psychologist within the EHCCC.
Data on telehealth and in‐person clinic attendances were obtained from the National Haemophilia EHR (indici™, supplied by Valentia Technologies Limited, 9 Exchange Place, IFSC, Dublin 1, Ireland).
Finally, data were collected directly from patients who contacted a dental helpline which was established to provide access to a teledentistry service operated by a consultant dental surgeon and dental nurse working remotely, for a 6‐week period. Data collected included pain scores, validated short form oral health related quality of life tool, 9 bleeding phenotype with a provisional diagnosis and management plan.
3. RESULTS
3.1. Medical and nursing consultation activity
In March 2020, strict public health measures were introduced to reduce the spread of COVID‐19 in Ireland. Consequently, medical and nursing clinic consultation activity in the EHCCC dropped by 63%, from 252 clinic consultations in March 2019 to just 94 in March 2020 (Figure 3A). The service implemented a telehealth care model on 16th March, leading to improved clinical activity in April, with 230 clinic consultations. However, this activity remained less than that in April 2019 (305 clinic consultations). With full integration and optimizing of telehealth we observed clinic consultation activity in May 2020 actually exceeded (52% greater) levels for the same time period the previous year (407 vs 268 clinic consultations). In total, 731 patients were reviewed by medical/nursing telehealth consultation, including 130 new patients and 601 return patients (median age 44 years (range 16‐91 years), 54% female and 46% male patients). The daily number of patients who underwent a teleconsultation varied and depended upon HCP availability but increased as HCPs gained experience and confidence with teleconsultation. Approximately half (51%) of patients reviewed live in the Dublin area and 49% live outside of Dublin, with some living over 300 km (greater than three hours travel time) from the EHCCC.
Figure 3.
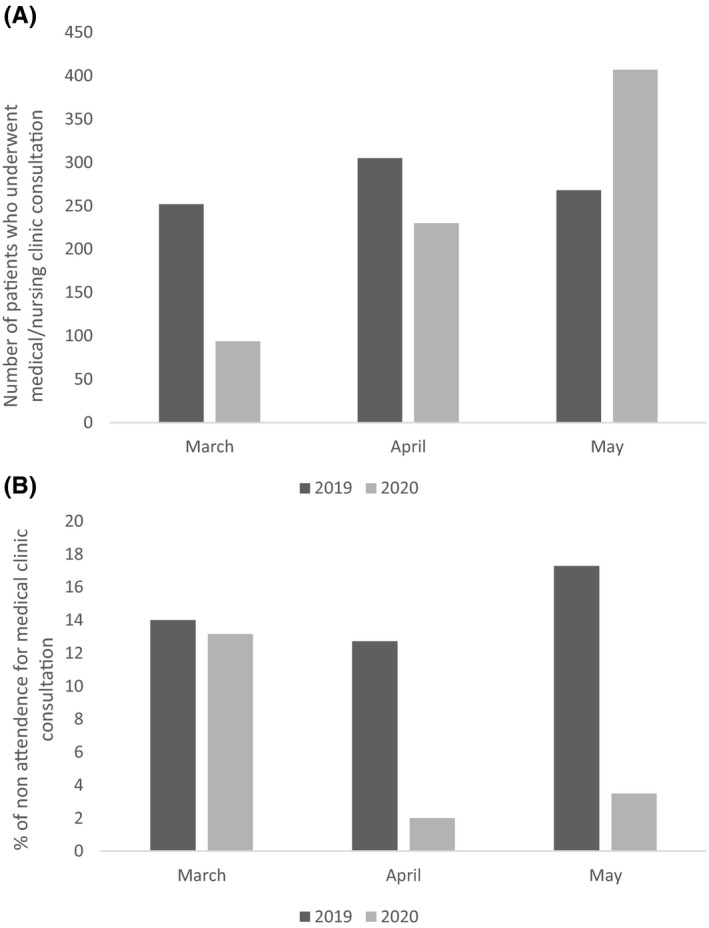
A, Bar chart comparing medical and nursing clinical consultation from March to May in 2019 and 2020. B, Bar chart comparing rates of non‐attendance at clinic appointments from March to May in 2019 and 2020
In keeping with our clinical activity data we also observed a 60% reduction in non‐attendance rates for clinic appointments after the introduction of teleconsultations, decreasing from 15% (March‐May 2019) to 6% for the same time period in 2020 (Figure 3B).
3.2. Patient Experience of telemedicine
Surveys were sent to 100 patients (55% male, 45% female, median age 47, range 17‐89 years) who had participated in medical and nursing telehealth consultations. The overall response rate was 36%; 29/84 telephone consultations, 7/16 video consultation.
A significant majority of respondents agreed or strongly agreed that telehealth consultations improved access (79%), reduced inconvenience (82%), were easy to use (94%) and enabled good communication with the healthcare team (97%) (Figure 4). Particular advantages were seen by people isolating at home on public health advice or those wanting to avoid attending the hospital due to COVID‐19 concerns. Respondents reported it was an advantage not to have travel time or need for hospital parking. Limitations of telehealth included patient factors such as visual impairment or language difficulties and poor internet access for video consultations, as well as patient preference for a face‐to‐face interaction.
Figure 4.
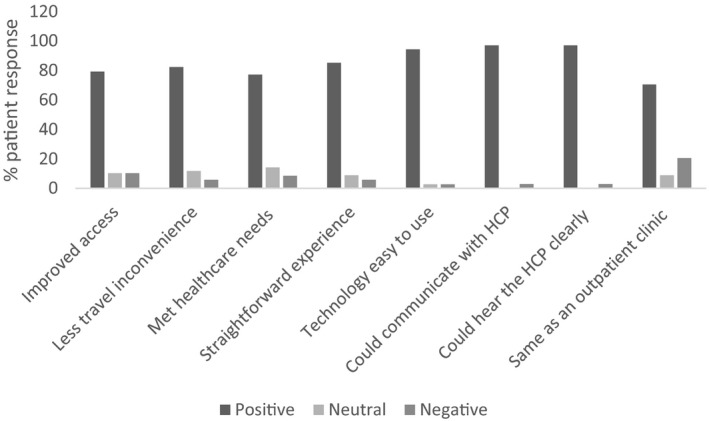
Bar chart illustrating the early patient experience of teleconsultation
3.3. Dental care
In total, 89 telephone or video consultations were conducted during a 6‐week period for acute dental issues. Pain scores of ≥7 were recorded by 18 (20%) patients, with 10% reporting maximum scores. Dental problems impacted significantly on relationship, sleep, nutrition or mood for 26 (29%) people and pain relief prescription was required for 29 (33%) patients who were not managing their dental pain adequately. Teletutoring on self‐placement of temporary fillings was provided for seven patients. Dental extractions with risk assessed management plans were arranged for 22 patients who had facial swelling due to dental abscess or severe toothache. Of the 22 dental extractions, 10 were carried out at the EHCCC dental clinic, following triage, for those patients with more severe bleeding phenotypes requiring factor replacement therapy in addition to dental‐specific local measures. In contrast, 12 extractions were managed locally for people with milder bleeding disorders using a combination of antifibrinolytic and local haemostatic dental measures. Telementoring for patients and their dentist, to assure their confidence and competence, was a key feature to ensure safe outcomes. There was no oral bleeding reported during the 6 weeks of data collection.
3.4. Physiotherapy
With the COVID‐19 restrictions, physiotherapy services also showed an initial reduction in clinical activity of 22% (42 consultations in March 2019 compared to 31 in March 2020, Figure 5). By May 2020, after the introduction of TM consultations on 16th March, clinical activity was 35% higher (49 vs 66 patient consultations) than for the same time the previous year. Consultations were carried out by telephone (46%), video (27%) or face‐to‐face (27%) for the reported time period of March to May 2020. Gait assessment with video consultation was felt to be adequate. Assessment of joint range of motion was possible but would require in‐person assessment for optimal evaluation. The video consultation activity included a new virtual exercise class initiative for people with haemophilia.
Figure 5.
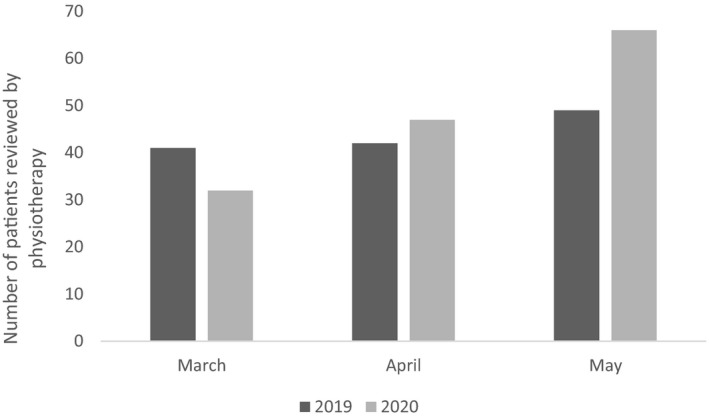
Bar chart comparing physiotherapy clinical activity from March to May in 2019 and 2020
A total of 38 PWSH responded to an anonymous survey from the EHCCC physiotherapy team, response rate of 29% (38/130). Of the respondents, 17 (45%) had participated in a teleconsultation with a HCP from the EHCCC, and the majority report being very satisfied (53%) or satisfied (41%) with the appointment. Regarding future engagement with telehealth, 15 (40%) PWSH report being very interested or interested in a remote annual physiotherapy assessment and 24 (63%) are very interested or interested in remote exercise class and education via video or exercise app.
3.5. Healthcare providers' experience of telemedicine
An anonymous online survey was performed to explore the early TM experience of HCPs within the EHCCC, 84% (21/25) survey response rate. Respondents included 9 (43%) nurses, 8 (38%) physicians, 3 (14%) allied health professionals (AHP), and 1 (5%) dentist. All those who responded had engaged with teleconsultation, 14 (67%) with telephone consultation and 7 (33%) with both video and telephone consultation.
The majority of HCPs were confident using teleconsultation, with 19/21 (90%) reporting confidence with telephone consultation and 6/7 (86%) with video consultations (Figure 6A). The inability to perform phlebotomy was not felt to be a major barrier for patient review for the majority (90%) of HCPs. Overall, HCPs were positive about teleconsultation and 17 (79%) would like to continue to offer teleconsultation as part of routine patient care and 18 (88%) would recommend teleconsultation to colleagues.
Figure 6.
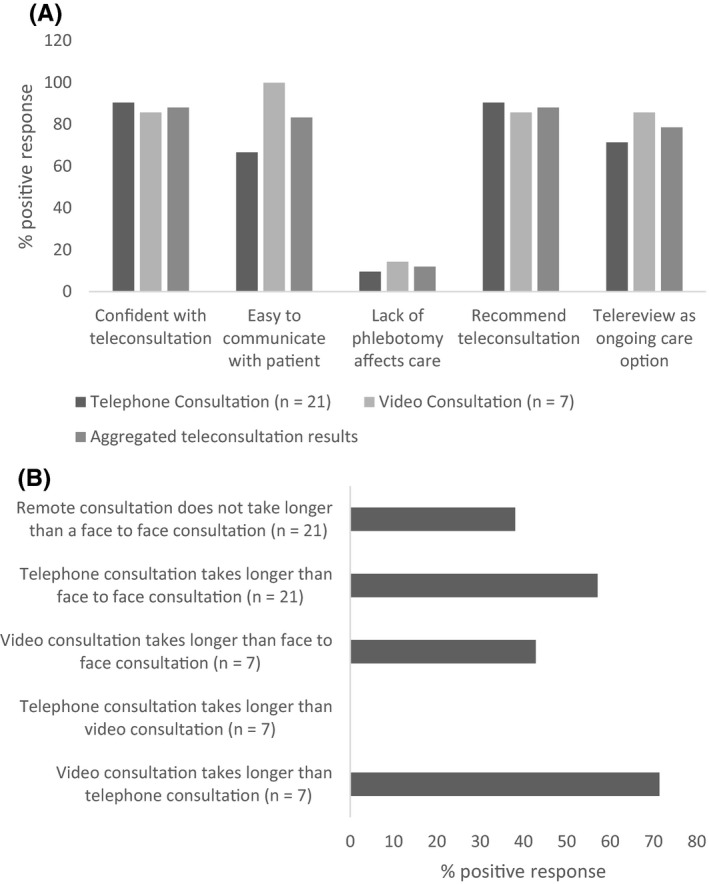
A, Bar chart illustrating the healthcare provider early experience of teleconsultation. B, Bar chart illustrating the duration of teleconsultations
Limitations associated with TM were also explored. Technical difficulties were reported by 8/21 (38%) HCPs in relation to telephone consults and by 5/7 (71%) in relation to video consultation, leading to longer consultations than planned in some cases. A small number, 3 (14%) HCPs, report that technical issues resulted in change of the original consultation modality. Lack of adequate resources to undertake video consultation was reported by 14 (67%) HCPs. All respondents felt adequately resourced to participate in telephone consultations. A need for specific training in telehealth consultation was identified, with 15 (71%) reporting an interest in formal education in this area.
Duration of teleconsultations was also a concern with 12/21 (57%) reporting telephone consultations and 3/7 (43%) reporting video consultations take longer than face‐to‐face consultations (Figure 6B). Interestingly 8 (38%) HCPs did not find that teleconsultations took longer than in‐person consultations.
Further limitations of TM highlighted by HCPs included lack of patient familiarity and acceptability of teleconsultation, patient factors such as communication difficulties (eg hearing impairment), comprehension issues (eg intellectual disability), as well as poor access to or limited experience with digital technology. Suggestions for improvements included patient education and patient choice of consultation type. The HCPs surveyed stressed the value of having the option to see the patient in‐person for physical examination and phlebotomy if required.
3.6. Psychology and social work consultations
Individual psychotherapy sessions were carried out by the Clinical Psychologist during this time period using telehealth consultation, including 18 telephone consultations and 12 video consultations. Video consultation performed better than expected for psychotherapy and manualized cognitive behavioural therapy interventions for pain also worked well through this medium.
Inpatients referred for Social Work consultations were reviewed by phone during the pandemic, and the social worker reported that face‐to‐face contact was more beneficial for establishing rapport and conducting a comprehensive assessment than teleconsultation.
3.7. Other roles of telehealth in the EHCCC
Video‐based teleconferencing has been used successfully for weekly multidisciplinary team meetings since the onset of COVID‐19 public health restrictions, as well as for monthly teleconferences with other haemophilia comprehensive care and treatment centres in Ireland. Multi‐specialty case conferences regarding complex clinical issues have been easier to organize and more frequent since the universal use of video‐based conferencing. Telehealth has also been embraced by the patient society, the Irish Haemophilia Society, which provided HCPs with the opportunity to interact with and regularly update the patient group via their teleconferencing platform. Teletwinning has enabled the ongoing twinning programme between Ireland and Jordan to proceed via a monthly webinar series, building on the existing relationships and work programme.
4. DISCUSSION
This systematic evaluation of TM in a European haemophilia comprehensive care centre shows the major impact on routine delivery of services for people with bleeding disorders in March 2020 associated with COVID‐19. Importantly, however, the rapid implementation of TM enabled rapid resumption of healthcare delivery and remote triage of acute issues. Healthcare access for patients was maintained, despite significant restrictions due to public health recommendations on social distancing and minimizing non‐urgent face‐to‐face patient contact. Indeed, medical, nursing and allied health professional clinical consultation activity was maintained in April 2020 and increased in May 2020, compared to 2019. Furthermore, it is notable that patient engagement with this type of healthcare delivery was increased, as emphasized by a reduction in non‐attendance rates.
The rapidity with which COVID‐19 became widespread globally meant that the switch to TM was necessarily rapid and widespread, with limited time for planning prior to implementation. While the implementation of TM was forced by circumstance, these novel results of the Irish experience show broad acceptance of this mode of service delivery and a recognition of potential benefits for both patients and HCPs. During the COVID‐19 pandemic TM has the potential to increase convenience, improve patient safety and better manage costs, as well as limiting exposures to patients and health care professionals. 10 There is evidence from studies, including randomized controlled trials, in other chronic disease settings that telehealth services can deliver safe and effective outcomes for patients. 11 , 12 , 13 Collectively, our data suggest that telehealth may not replace traditional physician‐patient interactions in all circumstances, but has the potential to augment face‐to‐face model of care. A pathway to arrange face‐to‐face consultation, if required, addresses HCP concerns regarding the inability to conduct a physical exam or take a blood test.
Access to dental care during the pandemic has been severely impacted as patients are unable to wear masks during assessments and aerosol generating procedures are common. Teledentistry, including intra‐oral photographs using a mobile phone, enabled urgent dental problems to be identified and addressed using a patient‐centred approach. Telementoring of dentists unfamiliar with haemophilia dental protocols alongside multidisciplinary online meetings enabled safe care using optimal clotting factor replacement regimes. Teledentistry has the possibility to improve access for this population after the pandemic has ceased.
Telehealth physiotherapy sessions were feasible and well‐received whether for acute assessment or for innovative strategies such as a teleexercise classes for people with haemophilia. This initiative is especially important as high rates of physical inactivity, overweight/obesity, increased waist‐hip ratio and reduced cardiorespiratory fitness have been reported in the Irish population. 14
Inevitably, challenges were encountered in telehealth implementation in the setting of an acute pandemic. Our study highlights the initial lack of adequate resources for video consultations related to the delay in sourcing suitable equipment and need for HCP training in delivering care via telehealth. Reimbursement was not a concern, as haemophilia services in Ireland are government funded with universal access. In other healthcare settings, new organizational workflow process is key to making the shift from complex out‐patient pathways that require physical presence of the patient to a new pathway instead dependent on the virtual presence of the patient. 15 Failing to modify these organizational routines is an important reason for unsuccessful video consultation programmes. Specific methods of communication in telehealth have been demonstrated to increase confidence and promote good clinical practice. 15 Examples include the types of ‘talk’ which are helpful in opening the consultation and establishing rapport as well as summarizing and safety netting. HCP will require support for the technical, professional and organizational changes required to underpin this significant change in practice. 16
Limitations of this study include an expected limited response to the patient postal survey response (36% and 29%) raising the possibility that there are uncaptured views amongst non‐responders. Those who responded may have been influenced by the public health crisis to answer positively and responses might be different in the absence of public health restrictions. The strength of the study is that it represents a national service and a typical EHCCC in Western Europe. There is a need for ongoing assessment of patient experience and other outcomes of TM in haemophilia care.
5. CONCLUSION
In conclusion, current optimal treatment for haemophilia needs to be personalized taking into account patient preferences, bleeding phenotype, joint status and activities. 17 The implementation of telehealth in the COVID‐19 pandemic has also heralded a new service delivery paradigm – the personalization of delivery of haemophilia comprehensive care through a blended model of face‐to‐face and TM. This hybrid model enables individualized care which is flexible and adaptable and recognizes the variability of personal circumstances. The application of a TM care model for people with bleeding disorders was rapidly implemented in response to a particular public health emergency but the benefits demonstrated for patient experience and choice, mean that TM should be maintained into the future.
AUTHOR CONTRIBUTONS
Contribution: CB, SR, M.M and NMO’C designed the surveys. M.O’D, CB, SR, MM, JB, LP, PB, GR, CB, DW, RB, FM HF, ES, SA, JSO’D, KR and AD were responsible for collection of the data. M.O’D, CB, CB and LP were responsible for data analysis and interpretation. M.O’D and NMO’C wrote the manuscript and all authors were involved in reviewing and revising the manuscript, with all authors granting final approval for the manuscript.
CONFLICT OF INTEREST
The authors have no competing interests.
ACKNOWLEDGEMENTS
The authors thank all members of the multidisciplinary team and patients of the National Coagulation Centre, Dublin who contributed data for this study. We would also like to acknowledge the collaboration with the Irish Haemophilia Society who advertized the telehealth service to their members.
O’Donovan M, Buckley C, Benson J, et al. Telehealth for delivery of haemophilia comprehensive care during the COVID‐19 pandemic. Haemophilia. 2020;26:984–990. 10.1111/hae.14156
REFERENCES
- 1. Hermans C, Weill A, Pierce GF. The Covid‐19 pandemic: new global challenges for the haemophilia community. Haemophilia. 2020;26(3):371‐372. [DOI] [PubMed] [Google Scholar]
- 2. Telemedicine FMJ. A Guide to Assessing Telecommunications for Health Care. Washington, DC: National Academies Press; 1996. [PubMed] [Google Scholar]
- 3. Dorsey E, Topol E. State of telehealth. N Eng J Med. 2016;375(2):154‐161. [DOI] [PubMed] [Google Scholar]
- 4. Kulkarni R. Use of telehealth in the delivery of comprehensive care for patients with haemophilia and other inherited bleeding disorders. Haemophilia. 2018;24(1):33‐42. [DOI] [PubMed] [Google Scholar]
- 5. Álvarez‐Román MT, De la Corte‐Rodríguez H, Rodríguez‐Merchán EC, et al. Covid‐19 and Telemedicine in Hemophilia in a Patient with Severe Hemophilia a and Orthopedic Surgery. Haemophilia. 2020. 10.1111/hae.14087. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ludikhuize L, Jansen M, Hooimeijer H, de Bont E, Tamminga R. Feasibility of video consultations in case of acute complications in children with haemophilia. Haemophilia. 2016;22(6):e567‐e570. [DOI] [PubMed] [Google Scholar]
- 7. Kulkarni R, Malouin RA. State of telehealth. N Eng J Med. 2016;375(14):1399‐1400. [DOI] [PubMed] [Google Scholar]
- 8. O'Donovan M, McGroarty F, Rehman KU, et al, editors. Design and Implementation of an Advanced E‐Health Haemophilia Platform in Ireland. Proceedings of the 13th Annual Congress of the European Association for Haemophilia and Allied disorders, 2020, Feb 5‐7, The Hague, Netherlands Haemophilia 2020; Wiley 111 River St, Hoboken 07030‐5774, NJ USA. Abstract published in haemophilia ‐ Haemophilia. 2020;26:98. 10.1111/hae.13911 [DOI] [Google Scholar]
- 9. Locker D, Allen PF. Developing short‐form measures of oral health‐related quality of life. J Public Health Dent. 2002;62(1):13‐20. [DOI] [PubMed] [Google Scholar]
- 10. Valentino LA, Skinner MW, Pipe S. The Role of Telemedicine in the Delivery of Healthcare in the Covid‐19 Pandemic. Haemophilia. 2020. 10.1111/hae.14044. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hansen CR, Perrild H, Koefoed BG, Zander MJ. Video Consultations as Add‐on to Standard Care among Patients with Type 2 Diabetes Not Responding to Standard Regimens: A Randomized Controlled Trial. Eur J Endocrinol. 2017;176(6):727‐736. [DOI] [PubMed] [Google Scholar]
- 12. Katz IJ, Pirabhahar S, Williamson P, et al. Iconnect Ckd‐Virtual Medical Consulting: A Web‐Based Chronic Kidney Disease, Hypertension and Diabetes Integrated Care Program. J Nephrology. 2018;23(7):646‐652. [DOI] [PubMed] [Google Scholar]
- 13. Nield M, Hoo GWS. Real‐Time Telehealth for Copd Self‐Management Using Skype™. J COPD: COPD. 2012;9(6):611‐619. [DOI] [PubMed] [Google Scholar]
- 14. Kennedy M, Roche S, McGowan M, et al, Physical Activity and Cardiometabolic Risk Profiles Amongst Irish Adults with Severe Haemophilia: The Irish Personalised Approach to the Treatment of Haemophilia (Ipath) Study. Proceedings of the 13th Annual Congress of the European Association for Haemophilia and Allied disorders, 2020, Feb 5–7, The Hague, Netherlands Haemophilia 2020; Wiley 111 River St, Hoboken 07030–5774, NJ USA. Abstract published in haemophilia ‐ Haemophilia. 2020;26:170. 10.1111/hae.13911 [DOI] [Google Scholar]
- 15. Wherton J, Shaw S, Papoutsi C, Seuren L, Greenhalgh T. Guidance on the Introduction and Use of Video Consultations During Covid‐19: Important Lessons from Qualitative Research. BMJ Lead. 2020;18:1‐5. [Google Scholar]
- 16. Greenhalgh T, Wherton J, Shaw S, Morrison C. Video Consultations for Covid‐19. BMJ. 2020;368:m998. [DOI] [PubMed] [Google Scholar]
- 17. Peyvandi F, Berger K, Seitz R, et al. Kreuth V initiative: European consensus proposals for treatment of haemophilia using standard products, extended half‐life coagulation factor concentrates and non‐replacement therapies. Haematologica. 2020;105(8):2038‐2043. [DOI] [PMC free article] [PubMed] [Google Scholar]


