Abstract
Using objectively-measured height and weight data from academic years 2009–2013 (n = 1,114,010 student-year observations), we estimated the association between the food outlet in closest proximity to schools and the likelihood of obesity among New York City public high school students. Obesity risk was higher for students with a corner store as the nearest option to schools, regardless of whether other food outlet types were located within a quarter mile or a half mile of schools (i.e., benchmarks for zoning policies). Policymakers may want to consider introducing healthier food options near schools, in conjunction with programs to support changes within corner stores.
Keywords: Obesity, Body mass index, Adolescents, Schools, Corner stores, Fast food restaurants, Supermarkets, Food policy, Zoning laws, Food environment
1. Background
In 2015–16, the prevalence of obesity among U.S. adolescents aged 12–19 years was 20.9%, only slightly higher than in 2007–2008 (18.1%) (Hales et al., 2018), with a higher prevalence among Black and Hispanic adolescents (Skinner et al., 2018). Previous studies suggest that obesity in adolescence persists into adulthood (Simmonds et al., 2015) and a high body mass index (BMI) in childhood is linked to a higher incidence of diabetes and coronary heart disease in adulthood (Llewellyn et al., 2016). Further, the prevalence of several cardiometabolic risk factors (e. g., total cholesterol, blood pressure) is higher among obese adolescents (Skinner et al., 2015). Adolescent obesity is driven in part by unhealthy dietary behaviors, including the intake of energy-dense, nutrient-poor foods and beverages and large portion size (Brown et al., 2015), particularly among racial/ethnic minority groups (Haughton et al., 2016).
Several characteristics of obesogenic environments contribute to disparities in excess calorie consumption (Kumar and Kelly, 2017), including the proximity of schools to healthy and unhealthy food outlets (i.e., establishments primarily engaged in retailing a general line of food products or providing food services to patrons). Previous research indicates that schools located in socioeconomically disadvantaged areas have a higher availability of unhealthy outlets (e.g., fast food restaurants, corner stores) (Díez et al., 2019), and low-income and Black and Hispanic students have greater access to unhealthy outlets surrounding schools, regardless of school location (Elbel et al., 2019; Neckerman et al., 2010; Sturm, 2008). This is problematic because consumption of food at fast food restaurants is linked to higher total energy intake and poorer diet quality among adolescents (Poti et al., 2014; Powell and Nguyen, 2013). For example, youth with fast food restaurants within a half mile of school consume fewer fruits and vegetables and more soda than those without these (Davis and Carpenter, 2009). Previous studies also show that corner stores surrounding schools primarily stock high-calorie foods and few healthy snacks (Laska et al., 2010; Lucan et al., 2010; Findholt et al., 2014; Gebauer and Laska, 2011); and that youth make purchases from corner stores an average of two times per week, more than other types of food outlets (Dennisuk et al., 2011). The items students most frequently purchase in corner stores include soda, chips, candy, and pastries (Lent et al., 2015; Borradaile et al., 2009); and healthier options in corner stores are often more expensive than less healthy options (Cavanaugh et al., 2013).
Previous research also suggests that the presence and proximity of fast food restaurants and convenience stores near public schools are positively associated with childhood and adolescent obesity (Howard et al., 2011; Chen et al., 2016; Currie et al., 2010; Powell et al., 2007; Sanchez et al., 2012) though results are sometimes inconsistent (Harris et al., 2011; Heroux et al., 2012; Tang et al., 2014; Dunn et al., 2014; Rossen et al., 2013). The inconsistency in findings may be due to differences in analytic approach (e.g., buffer size) or study sample (e.g., grade level). Further, the majority of previous studies ignores potential endogeneity, such as residential self-selection and non-random siting of food outlets (Rummo et al., 2017, Rummo et al., 2017). To our knowledge, only a few studies have used sophisticated methods to address potential endogeneity related to fast food restaurant availability around schools (Currie et al., 2010; Dunn et al., 2014; Alviola et al., 2011). However, no studies have attempted to address bias related to other food outlet types, such as corner stores and bodegas.
There have been numerous changes to the food environment within schools during the past decade, including updated school meal standards and new requirements for competitive foods and beverages (Welker et al., 2016). Mimicking current bans on alcohol and tobacco outlets, a small number of U.S. municipalities have also prohibited fast food restaurants from locating near schools, including Detroit, MI and Arden Hills, MI (Municipal Code § 61–12–91, 2008; Municipal Code § 1325.04 (1)(A), 2006). In 2006 and 2009, two proposals were made to limit the proximity of fast food restaurants to schools in New York City (NYC), but the legislation did not pass (Buckley, 2009; Fernandez, 2006). Elsewhere, the mayor of London recently proposed a zoning restriction on fast food restaurants locating within a quarter mile of public schools (Reality Check Team, 2017). These efforts highlight potential opportunities to leverage the school food environment to improve the dietary behaviors of students, especially for those in sociodemographic groups with greater exposure to unhealthy food outlets. However, more evidence is needed to identify which aspects of the retail food environment around schools is driving the relationship with students’ weight status, and the potential impact of zoning policies targeting a wider array of food outlet types.
Using student-level demographic and weight data from the NYC Department of Education and public food outlet data, we sought to estimate the association between the food outlet type nearest to public high schools and the likelihood of obesity in academic years 2009–2013. We used census tract level fixed effects to control for unobserved differences across students’ residential neighborhoods. This strategy allows us to compare students living within the same census tract, thus controlling for unobserved selection into residential neighborhoods. We hypothesized that the likelihood of obesity would be higher for students who attended public high schools with a fast food restaurant or a corner store as the nearest food outlet type, and the strength of the association would increase as distance to the nearest food outlet type decreased.
2. Methods
2.1. Participants
Our sample included students in grades 9–12 enrolled in NYC public schools from academic years 2009–2013. We focused on high school students because we expect these students to have relatively greater freedom of movement and disposable income to purchase food from food outlets near their schools than younger students. In academic years 2009–2013, a total of 607,345 students (n = 1,435,103 student-year observations) were enrolled in non-special education or non-charter schools (n = 706 schools). Of these students, 78,511 were excluded for not having residential address data; 64,582 for missing school address data; 28,682 for living in a home or attending a school within 0.50 miles of a NYC border; 143,674 for attending a school with multiple food outlet types located nearest; and 89,756 for not having a food outlet of any type within 0.50 miles of their school.
2.2. Exposures
Based on prior research (Cobb et al., 2015), we included fast food restaurants and corner stores/bodegas as proxies for access to unhealthy foods, and wait-service restaurants and supermarkets as proxies for access to healthy foods. To determine the address of restaurants open at the beginning of each academic year, we used the NYC Department of Health and Mental Hygiene Restaurant Grading data. Restaurants are inspected at least once per calendar year. We defined wait-service restaurants as having wait/table service (39.9% of all restaurants in NYC from 2009 to 2013), and the remaining restaurants were defined as fast food restaurant as they either did not offer wait service or did not specify service type (60.1%). To determine the address of food stores open at the beginning of each academic year, we used the New York State Department of Agriculture and Markets, Licensing and Inspection data. In accordance with NYC’s Food Retail Expansion to Support Health Program (FRESH) initiative, we defined corner stores and bodegas as food stores with a floor area less than 6000 square feet (90.8% of all food stores) and supermarkets as food stores with a floor area over 6000 square feet (9.2%). We did not include other retail store types (e.g., pharmacies) in our analysis. Previous work has shown that the agreement between ground observations and food stores and restaurants in government inspection data was moderate (Lucan et al., 2020).
To reflect the intent of zoning laws restricting unhealthy food outlets from locating near schools, we created an indicator variable for the type of the nearest food outlet for each school. To reflect the idea that adolescents are more likely to purchase food items in closer proximity to their schools regardless of whether it is nearest, we created a variable capturing the street network distance (shortest path using street segments) from the school to that nearest food outlet. To estimate the potential impact of a proposed zoning law, we also created a set of mutually exclusive categories for the nearest food outlet based on distance, including <0.25 miles (~0–5 blocks in NYC) and 0.25–0.50 miles (~5–10 blocks). We used ArcGIS 10.5 to calculate the distance between school addresses and food outlets addresses each academic year.
2.3. Outcomes and measures
To measure BMI at each year, we used data from NYC FITNESSGRAM, an annual, school-based, standardized fitness assessment of every NYC public school student in grades K-12. FITNESSGRAM data has been shown to have strong reliability and validity (Morrow et al., 2010). Height and weight data were collected once per year by a physical education teacher or a school nurse throughout the year (n = 1.75 BMI measurements across 2009–2013). We calculated the BMI measurement for each student per year, then compared the score with Centers for Disease Control and Prevention growth charts grouped by age and gender. Those with a BMI ≥ 95 percentile on the chart were defined as obese. We also calculated zBMI by standardizing BMI by gender and age among all students.
Additional measures in our analysis included students’ gender, age, grade, race/ethnicity (Black, White, Hispanic/Latino, and Asian & Other), native born, special education status, whether English was spoken at home, and poverty status (defined as whether the student ever qualified for free/reduced-price lunch, as a proxy for family income below 185% of the Federal Poverty Level). These measures are self-reported by parents at the beginning of the school year.
2.4. Multiple imputation
To include students missing height or weight data (n = 255,175) and demographic data (n = 17,760) in our statistical analysis, we performed multiple imputation by chained equations (n = 5 imputations) (White et al., 2011). Our predictor variables included gender, age, race/ethnicity, native born, special education status, poverty status, and distances to food outlets by type; and auxiliary variables, including obesity status in previous or later academic years and whether the student ever lived in public housing in academic years 2009–2013. After imputation, the total number of students in our final analytic sample was 361,942 (n = 1,114,010 student-year observations).
2.5. Statistical analysis
In our primary analysis, we examined the association between the nearest food outlet type and students’ likelihood of obesity using Ordinary Least Squares (OLS) regression with robust standard errors. In our primary model, we used home census tract fixed effects (the inclusion of a separate indicator variable for each home census tract, excluding one reference tract), and clustered at the student level. To account for sociodemographic differences in obesity risk, we controlled for student sociodemographic characteristics, including gender, age, grade, race/ethnicity, native born, speaking English at home, special education status, and poverty status. We also controlled for year. To account for the proximity of the nearest food outlet type, we also included a main continuous variable for distance (in 1000 feet) to the nearest food outlet type, with an interaction effect between the nearest food outlet type and distance. The model is as follows:
| (1) |
where Dist is the distance to the nearest food outlet from a student’s school; FF, WS, BOD, and SUP are dichotomous variables that indicate the nearest food outlet type from a student’s school, including fast food restaurants, wait-service restaurants, corner stores/bodegas, and supermarkets, respectively; Demo is a vector of student demographic and housing control variables; NumOutlet is a vector of variables representing the count of each food outlet type (separately) within 0.50 miles of schools; and Year and HomeCT represent year and home census tract fixed effects, respectively, for student i in year t.
To estimate the potential impact of a zoning law restricting unhealthy food outlets (e.g., fast food restaurants, convenience stores) from locating <0.25 miles of schools, we also examined the association between our mutually exclusive categories of nearest food outlet type located <0.25 miles and within 0.25–0.50 miles of schools with the probability of obesity. The model is as follows:
| (2) |
where FFqtr, WSqtr, and SUPqtr indicate whether the nearest food outlet type was located <0.25 miles from a student’s school; and BODhalf, FFhalf, WShalf, and SUPhalf indicate whether the nearest food outlet was located within 0.25–0.50 miles from a student’s school. The remaining variables are identical to Eq. (1).
We performed pairwise contrasts (differences) of the predicted likelihood of obesity across the levels of our exposure variables (i.e., nearest food outlet type) and distance to nearest food outlet using a one degree of freedom test at α < 0.05 (Supplementary Table 1). We also performed supplementary analyses, including adding an interaction term for a) school borough (Bronx, Kings, New York, Queens and Richmond counties); b) gender; c) race/ethnicity; and d) eligibility for free or reduced-price lunch; not excluding schools with multiple food outlet types located nearest; and lagging outcome data by one year. We used Stata version 16 for all analyses. (Series StataCorp, 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC).
3. Results
Our sample of public high school students was predominately Hispanic/Latino (40.7%) and Black (30.5%), and eligible for free or reduced priced lunch (92.1%) (Table 1). In 2013, about 15.9% of the sample was obese and mean zBMI was 0.50 (SD = 1.10). On average, students attended schools that were located 563.4 (SD = 503.8) feet (~2 NYC blocks) from the nearest food outlet of any type, the majority of which were fast food restaurants (43.9%) or corner stores (40.5%) (Table 2). For a majority of students (89.0%), the nearest food outlet was located <0.25 miles of schools. Among students attending a school with multiple food outlet types located nearest (n = 82,467), the majority of their co-located food outlets were fast food restaurants and wait-service restaurants (54.5%), such as cafeterias and food courts.
Table 1.
Sample characteristics, overall and by food outlet type.
| Characteristic | Overall | Nearest food outlet type |
|||
|---|---|---|---|---|---|
| Fast food | Corner store | Wait-service | Supermarket | ||
| Female (%) | 49.3 | 50.8 | 47.0 | 51.7 | 44.4 |
| Age (mean (SD)) | 16.5 | 16.4 | 16.6 | 16.4 | 16.3 |
| Race/ethnicity (%) | |||||
| Asian & Other | 17.0 | 19.2 | 14.9 | 17.3 | 6.4 |
| Hispanic/Latino | 40.7 | 37.3 | 42.8 | 44.1 | 51.6 |
| Black | 30.5 | 31.0 | 31.6 | 25.3 | 35.6 |
| White | 11.9 | 12.5 | 10.8 | 13.3 | 6.3 |
| Eligibility for free or reduced priced lunch (%) | 92.6 | 91.7 | 94.4 | 90.3 | 95.8 |
| Speaks English at home (%)a | 53.4 | 54.3 | 52.0 | 53.0 | 66.3 |
| Special education (%) | 12.9 | 12.1 | 12.4 | 13.7 | 15.5 |
| Native born | 74.9 | 75.5 | 73.0 | 77.1 | 86.9 |
| zBMI (mean (SD))a | 0.50 (1.10) | 0.48 (1.10) | 0.52 (1.11) | 0.51 (1.09) | 0.55 (1.09) |
| Obesity (%) | 15.9 | 15.3 | 16.4 | 16.3 | 16.9 |
Note: The sample includes NYC public high school students (districts 1–32) with at least one food outlet of any type within 10 blocks from their school with home and school address data in Academic Year (2013). We excluded students enrolled in schools less than 0.50 miles from NYC boundaries and special education only schools or charter schools.
BMI = body mass index.
Not imputed due to multi-collinearity.
Table 2.
Distribution of students by distance to nearest food outlet from school, overall and by type.
| Distance to nearest food outlet | N (%) | Mean ft. (SD) |
|---|---|---|
| All food outlet types | 226,780 | 563.4 (503.8) |
| Overall | ||
| Corner store | 91,627 (40.5) | 530.2 (414.5) |
| Fast food restaurant | 99,627 (43.9) | 619.8 (566.5) |
| Wait-service restaurant | 32,315 (14.3) | 493.4 (530.6) |
| Supermarket | 3073 (1.4) | 485.8 (204.5) |
| Less than 0.25 miles | ||
| Corner store | 83,948 (37.0) | 436.0 (287.8) |
| Fast food restaurant | 88,240 (38.9) | 456.6 (348.1) |
| Wait-service restaurant | 26,566 (11.7) | 265.0 (177.3) |
| Supermarket | 3073 (1.4) | 485.8 (204.5) |
| 0.25 – 0.50 miles | ||
| Corner store | 11,387 (5.0) | 1878.7 (279.1) |
| Fast food restaurant | 7817 (3.5) | 1540.7 (103.7) |
| Wait-service restaurant | 5749 (2.5) | 1548.8 (286.5) |
| Supermarket | 0 | – |
Note: The sample includes NYC public high school students with at least one food outlet of any type within 10 blocks from their school with home and school address data in Academic Year (2013). We excluded students enrolled in schools less than 0.50 miles from NYC boundaries and special education only schools or charter schools.
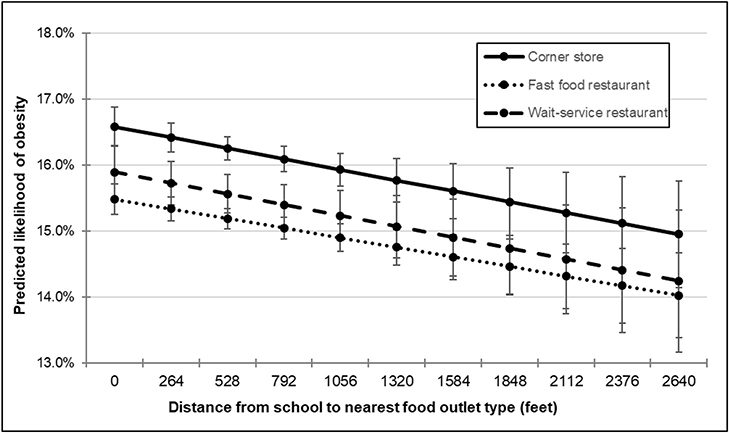
We observed that students who attended schools located nearest to a corner store had a statistically significantly higher predicted likelihood of obesity (16.2%; 95% CI: 16.0, 16.4) relative to students located nearest to fast food restaurants (15.2%; 95% CI: 15.0, 15.3) and wait-service restaurants (15.5%; 95% CI: 15.2, 15.8) (Supplementary Table 1). We did not observe a difference between corner stores and supermarkets (15.6%; 95% CI: 14.8, 16.4), possibly due to insufficient variation in students’ proximity to supermarkets.
On average, the distance from schools to the nearest food outlet of any type was inversely associated with the probability of obesity. For example, the predicted likelihood of obesity was 0.7 (95% CI: −1.1, −0.2) percentage points lower for students with a corner store as the nearest option located ~5 blocks from school versus ~1 block from school (Supplementary Table 2). The estimates for the interaction between distance and nearest food outlet type were not statistically significant, indicating that the magnitude of the inverse association between distance to the nearest food outlet and obesity was similar among food outlet types.
In Fig. 1, we also observe that the predicted likelihood of obesity was meaningfully higher among students attending a school with a corner store as their nearest option (compared to fast food restaurants and wait-service restaurants), regardless of the distance to the nearest food outlet type. For example, compared to fast food restaurants, the predicted likelihood of obesity was similar for students with a corner store as the nearest option ~1 block from school [−1.1% (95% CI: −0.8, −1.4)] versus ~5 blocks from school [1.2% (95% CI: −1.5, −1.0)]. In supplementary analyses, we observed similar findings by borough, gender, race/ethnicity, and eligibility for free or reduced-price lunch (Supplementary Tables 3–10). We also observed similar findings in analyses where we did not exclude schools with multiple food outlet types located nearest and lagged outcome data by one year (Supplementary Tables 11–12).
Fig. 1.
Predicted likelihood of obesity by food outlet typea and distance to nearest food outlet type.b.
Note: The sample includes NYC public high school students with at least one food outlet of any type within 10 blocks from their school with home and school address data in Academic Years 2009–2013. We exclude students enrolled in schools less than 0.50 miles from NYC boundaries, and special education only schools.
aSupermarkets omitted due to wide confidence interval estimates.
bEffects were estimated using a linear regression model with census tract level and year fixed effects, controlling for students demographic and housing characteristics, which includes race/ethnicity, gender, eligibility for free or reduced-price lunch, native born, special education, speaking English at home, age, grade and the building type of their home. Predicted likelihood is calculated using post-estimation marginal commands.
Relative to students with a corner store as the nearest food outlet type located <0.25 miles of school, students with a supermarket, fast food restaurant, or wait-service restaurant located <0.25 miles of school had a significantly lower likelihood of obesity (Table 3). The same pertains to students with a fast food restaurant or wait-service restaurant located within 0.25–0.50 miles of school. However, we observed no difference between students with a corner store as the nearest food outlet type located <0.25 miles of school compared to students with a corner store as the nearest food outlet type within 0.25–5.0 miles of school.
Table 3.
Estimated effect of nearest food outlet type on obesity, <0.25 miles versus 0.25–0.50 miles.a
| Food outlet type, by distance from high school | Coefficient (β (SE)) | Predicted likelihood (95% CI)b |
|---|---|---|
| Corner store (<0.25 miles) | REF | 0.162 (0.160, 0.164) |
| Fast food restaurant (<0.25 miles) | −0.013 (0.001)*** | 0.152 (0.150, 0.153) |
| Wait-service restaurant (<0.25 miles) | −0.009 (0.001)*** | 0.156 (0.153, 0.159) |
| Supermarket (<0.25 miles) | −0.012 (0.003)*** | 0.155 (0.148, 0.163) |
| Corner store (0.25–0.50 miles) | −0.001 (0.002) | 0.16 (0.155, 0.166) |
| Fast food restaurant (0.25–0.50 miles) | −0.025 (0.002)*** | 0.153 (0.146, 0.160) |
| Wait-service restaurant (0.25–0.50 miles) | −0.009 (0.003)*** | 0.162 (0.160, 0.164) |
| Supermarketc (0.25–0.50 miles) | – | – |
| Student-observations (N) | 780,950 | 780,950 |
Note: Boldface indicates statistical significance (*p < 0.05, **p < 0.01, ***p < 0.001). The sample includes NYC public high school students with at least one food outlet of any type within 0.50 miles (about 10 NYC blocks) from their school with home and school address data in Academic Years 2009–2013. We exclude students enrolled in schools less than 0.50 miles from NYC boundaries and special education only schools or charter schools.
Effects were estimated using a linear regression model with census tract level and year fixed effects, controlling for students demographic and housing characteristics, which includes race/ethnicity, gender, eligibility for free or reduced-price lunch, native born, special education, speaking English at home, age, grade and the building type of their home. We also controlled for the overall food environment around the school, accounting for the number of total food outlet within 10 blocks.
Predicted likelihood was calculated using post-estimation marginal commands.
Omitted due to lack of observations.
4. Discussion
Using five years of objectively-measured height and weight data linked to comprehensive food outlet data, we found that the likelihood of obesity was higher for students who attended public high schools with a corner store as the nearest food outlet type (approximately 0.8–1.2% points higher), especially if the corner store was located closer to schools. This finding is consistent with our previous work showing that very near distances to fast food restaurants and corner stores around students’ homes had a positive impact on childhood obesity (Langellier et al., 2013). Both fast food restaurants and corner stores sell energy-dense, nutrient-poor food items and few healthy options (Cavanaugh et al., 2013; Gebauer and Laska, 2011; Laska et al., 2010; Lucan et al., 2010; Poti et al., 2014), including those located in NYC (Neckerman et al., 2014). However, adolescents may visit corner stores more frequently than fast food restaurants (Dennisuk et al., 2011) and the close proximity of corner stores may contribute to increased snacking behavior among students, especially of unhealthy food items (Borradaile et al., 2009).
Substantively, our results are consistent with findings reported in a review article showing that the presence and proximity of convenience stores near schools is positively associated with adolescent obesity (Williams et al., 2014). However, comparisons with previous findings are limited by the dearth of existing studies addressing unmeasured confounding. A notable exception is a study that used the transition of students to higher grades as an identification strategy, and found no association between fast food restaurants located along the commute from home to school and obesity rates (Dunn et al., 2014). Other studies have used the distance between schools and major highways as an instrument to estimate the effects of fast food availability on school-level obesity rates (Alviola et al., 2011), or school fixed effects to address potential endogeneity (Currie et al., 2010; Alviola et al., 2011). However, these studies did not include corner stores in their analyses. To our knowledge, our study is the first to consider the impact of multiple food outlets around schools on adolescent obesity, with an estimation strategy to mitigate potential bias due to unmeasured confounding at the neighborhood level.
We also used a similar approach to mimic a potential zoning policy that would restrict unhealthy food outlet types from locating near public schools. Our results indicate that the probability of obesity was higher for students with a corner store as the nearest option relative to other food outlet types (including supermarkets), regardless of whether other food outlet types were located within a quarter or half mile of schools. In contrast, the probability of obesity did not differ for students with a corner store as the nearest option within a quarter versus half mile of schools. Taken together, these findings suggest that a zoning law restricting corner stores from locating within a quarter mile of schools might help mitigate obesity risk if a different food outlet type were located the nearest. Our recent work also shows that low-income and Black, Hispanic, and Asian students had greater access from school to all food outlets compared to low-income and White students in NYC (Elbel et al., 2019), which suggests that equitable policies and programs focused on eliminating disparities might be most effective. Complementary approaches include supporting programs that improve the food environment within schools themselves, such as reducing the presence of competitive foods and increasing water access, and expanding the availability and quality of healthy foods within existing corner stores (vs. focusing on access to corner stores) (Langellier et al., 2013).
Our study had several limitations, including a lack of data on food purchasing and consumption behaviors. Similarly, we did not capture what food items were actually sold within food outlets surrounding schools. We also did not have access to individual-level data on students attending non-public schools. However, we were able to obtain comprehensive, time-varying data for the vast majority of public school students and their school food environment, with low levels of missingness. Further, we were able to control for unobserved differences across students’ residential neighborhoods using students’ home addresses. Though a model with census tract fixed effects is an effective strategy to address potential endogeneity, our estimates only address one source of potential confounding (i.e., sorting into neighborhoods) and should be interpreted with caution. We also acknowledge that school and residential mobility may have contributed to misclassification of students’ retail food measures and neighborhood sociodemographic characteristics. Lastly, our results may not be generalizable to students attending schools located in non-urban areas.
In sum, our results suggest that close proximity of corner stores to public high schools is associated with higher obesity risk among adolescents in NYC, which may contribute to higher chronic disease risk, especially at the population level (Hruby and Hu, 2015). In addition, our findings suggest that a potential policy to restrict corner stores from siting near schools may reduce their impact on adolescent obesity rates, if alternative food outlet types were located in closest proximity to schools. Policymakers may want to consider complementary solutions to mitigate obesity risk among adolescents in public high schools, such as programs supporting policies to increase the availability, acceptability, and affordability of healthy meals and snacks within public schools.
Supplementary Material
Acknowledgments
Funding
This study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (R01DK097347; PI: B. Elbel).
List of abbreviations
- NYC
New York City
- BMI
body mass index
Footnotes
Declaration of competing interest
The other authors have indicated they have no potential conflicts of interest to disclose.
Financial disclosure
The other authors have indicated they have no financial relationships relevant to this article to disclose.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.healthplace.2020.102408.
References
- Alviola P, Nayga R, Thomsen M, Danforth D, Smartt J, 2011. The Effect of Fast-Food Restaurants on School-Level Obesity. Department of Agricultural Economics and Agribusiness, University of Arkansas. [Google Scholar]
- Borradaile KE, Sherman S, Vander Veur SS, Mccoy T, Sandoval B, Nachmani J, Karpyn A, Foster GD, 2009. Snacking in children: the role of urban corner stores. Pediatrics 124, 1293–1298. [DOI] [PubMed] [Google Scholar]
- Brown CL, Halvorson EE, Cohen GM, Lazorick S, Skelton JA, 2015. Addressing childhood obesity: opportunities for prevention. Pediatr. Clin. 62, 1241–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley C, 2009. A Proposal to Separate Fast Food and Schools. The New York Times. [Google Scholar]
- Cavanaugh E, Mallya G, Brensinger C, Tierney A, Glanz K, 2013. Nutrition environments in corner stores in Philadelphia. Prev. Med. 56, 149–151. [DOI] [PubMed] [Google Scholar]
- Chen D, Thomsen MR, Nayga RM, Bennett JL, 2016. Persistent disparities in obesity risk among public schoolchildren from childhood through adolescence. Prev. Med. 89, 207–210. [DOI] [PubMed] [Google Scholar]
- Cobb LK, Appel LJ, Franco M, Jones-Smith JC, Nur A, Anderson CA, 2015. The relationship of the local food environment with obesity: a systematic review of methods, study quality, and results. Obesity 23, 1331–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J, Dellavigna S, Moretti E, Pathania V, 2010. The effect of fast food restaurants on obesity and weight gain. Am. Econ. J. Econ. Pol. 2, 32–63. [Google Scholar]
- Davis B, Carpenter C, 2009. Proximity of fast-food restaurants to schools and adolescent obesity. Am. J. Publ. Health 99, 505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennisuk LA, Coutinho AJ, Suratkar S, Surkan PJ, Christiansen K, Riley M, Anliker JA, Sharma S, Gittelsohn J, 2011. Food expenditures and food purchasing among low-income, urban, African-American youth. Am. J. Prev. Med. 40, 625–628. [DOI] [PubMed] [Google Scholar]
- Díez J, Cebrecos A, Rapela A, Borrell LN, Bilal U, Franco M, 2019. Socioeconomic inequalities in the retail food environment around schools in a southern European context. Nutrients 11, 1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn RA, Nayga RM Jr., Thomsen M, Rouse HL, 2014. A longitudinal analysis of fast-food exposure on child weight outcomes: identifying causality through school transitions. Work. Pap. 34 10.22004/ag.econ.290100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbel B, Tamura K, McDermott ZT, Duncan DT, Athens JK, Wu E, Mijanovich T, Schwartz AE, 2019. June Disparities in food access around homes and schools for New York City children. PLoS One 1214 (6), e0217341 10.1371/journal.pone.0217341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez M, 2006. Pros and Cons of a Zoning Diet: Fighting Obesity by Limiting Fast-Food Restaurants. The New York Times. https://www.nytimes.com/2006/09/24/nyregion/24fast.html Accessed: April 2020.
- Fresh Nyc. Zoning districts & tools: fresh food stores -DCP [Online]. Available: https://www1.nyc.gov/site/planning/zoning/districts-tools/fresh-food-stores.page. Accessed: 2018.
- Findholt NE, Izumi BT, Nguyen T, Pickus H, Chen Z, 2014. Availability of healthy snack foods and beverages in stores near high-income urban, low-income urban, and rural elementary and middle schools in Oregon. Child. Obes. 10, 342–348. [DOI] [PubMed] [Google Scholar]
- Gebauer H, Laska MN, 2011. Convenience stores surrounding urban schools: an assessment of healthy food availability, advertising, and product placement. J. Urban Health 88, 616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL, 2018. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. J. Am. Med. Assoc. 319, 1723–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris DE, Blum JW, Bampton M, O’brien LM, Beaudoin CM, Polacsek M, O’rourke KA, 2011. Location of food stores near schools does not predict the weight status of Maine high school students. J. Nutr. Educ. Behav. 43, 274–278. [DOI] [PubMed] [Google Scholar]
- Haughton CF, Wang ML, Lemon SC, 2016. Racial/ethnic disparities in meeting 5–2-1–0 recommendations among children and adolescents in the United States. J. Pediatr. 175, 188–194.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heroux M, Iannotti RJ, Currie D, Pickett W, Janssen I, 2012. The food retail environment in school neighborhoods and its relation to lunchtime eating behaviors in youth from three countries. Health Place 18, 1240–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard PH, Fitzpatrick M, Fulfrost B, 2011. Proximity of food retailers to schools and rates of overweight ninth grade students: an ecological study in California. BMC Publ. Health 11, 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hruby A, Hu FB, 2015. The epidemiology of obesity: a big picture. Pharmacoeconomics 33, 673–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S, Kelly AS, 2017. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin. Proc. 92, 251–265. [DOI] [PubMed] [Google Scholar]
- Langellier BA, Garza JR, Prelip ML, Glik D, Brookmeyer R, Ortega AN, 2013. Corner store inventories, purchases, and strategies for intervention: a review of the literature. Calif. J. Health Promot 11, 1. [PMC free article] [PubMed] [Google Scholar]
- Laska MN, Borradaile KE, Tester J, Foster GD, Gittelsohn J, 2010. Healthy food availability in small urban food stores: a comparison of four US cities. Publ. Health Nutr. 13, 1031–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lent MR, Vander Veur S, Mallya G, Mccoy TA, Sanders TA, Colby L, Rauchut Tewksbury C, Lawman HG, Sandoval B, Sherman S, Wylie-Rosett J, Foster GD, 2015. Corner store purchases made by adults, adolescents and children: items, nutritional characteristics and amount spent. Publ. Health Nutr. 18, 1706–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llewellyn A, Simmonds M, Owen CG, Woolacott N, 2016. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes. Rev. 17, 56–67. [DOI] [PubMed] [Google Scholar]
- Lucan SC, Karpyn A, Sherman S, 2010. Storing empty calories and chronic disease risk: snack-food products, nutritive content, and manufacturers in Philadelphia corner stores. J. Urban Health 87, 394–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucan SC, Maroko AR, Abrams C, Rodriguez N, Patel AN, Gjonbalaj I, Schechter CB, Elbel B, 2020. Jun. Government data v. ground observation for food-environment assessment: businesses missed and misreported by city and state inspection records. Public Health Nutr 23 (8), 1414–1427. 10.1017/S1368980019002982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow JR Jr., Martin SB, Jackson AW, 2010. Reliability and validity of the FITNESSGRAM: quality of teacher-collected health-related fitness surveillance data. Res. Q. Exerc. Sport 81, S24–S30. [DOI] [PubMed] [Google Scholar]
- Municipal Code § 1325.04, 2006. Arden Hills, Minnesota, vol. 1. A. [Google Scholar]
- Municipal Code § 61–12-91, 2008. Detroit, Michigan. [Google Scholar]
- Neckerman KM, Bader MD, Richards CA, Purciel M, Quinn JW, Thomas JS, Warbelow C, Weiss CC, Lovasi GS, Rundle A, 2010. Disparities in the food environments of New York City public schools. Am. J. Prev. Med. 39, 195–202. [DOI] [PubMed] [Google Scholar]
- Neckerman KM, Lovasi L, Yousefzadeh P, Sheehan D, Milinkovic K, Baecker A, Bader MD, Weiss C, Lovasi GS, Rundle A, 2014. Comparing nutrition environments in bodegas and fast-food restaurants. J. Acad. Nutr. Diet. 114, 595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NYC FITNESSGRAM. New York City (NYC) school wellness programs. New York City Department of Education. Available: http://nycphysicaleducation.com/nyc-fitnessgram/. Accessed: 2018.
- Poti JM, Slining MM, Popkin BM, 2014. Where are kids getting their empty calories? Stores, schools, and fast-food restaurants each played an important role in empty calorie intake among US children during 2009–2010. J. Acad. Nutr. Diet. 114, 908–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Auld MC, Chaloupka FJ, O’malley PM, Johnston LD, 2007. Associations between access to food stores and adolescent body mass index. Am. J. Prev. Med. 33, S301–S307. [DOI] [PubMed] [Google Scholar]
- Powell LM, Nguyen BT, 2013. Fast-food and full-service restaurant consumption among children and adolescents: effect on energy, beverage, and nutrient intake. JAMA Pediatr. 167, 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reality Check Team, 2017. Why ban fast food within 400m of schools? BBC News. Available: https://www.bbc.com/news/health-42172579.
- Rossen LM, Curriero FC, Cooley-Strickland M, Pollack KM, 2013. Food availability en route to school and anthropometric change in urban children. J. Urban Health 90, 653–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rummo Pasquale, Guilkey David, Ng Shu Wen, Popkin Barry, EvensonKellyGordon-Larsen Penny, 2017. Beyond Supermarkets: Food Outlet Location Selection in Four U.S. Cities Over Time. Am J Prev Med 52 (3), 300–310. 10.1016/j.amepre.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rummo Pasquale, Guilkey David, Shikany James, ReisJaredGordon-Larsen Penny, 2017. How do individual-level sociodemographics and neighbourhood-level characteristics influence residential location behaviour in the context of the food and built environment? Findings from 25 years of follow-up in the CARDIA Study. J Epidemiol Community Health 71 (3), 261–268. 10.1136/jech-2016-207249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez BN, Sanchez-Vaznaugh EV, Uscilka A, Baek J, Zhang L, 2012. Differential associations between the food environment near schools and childhood overweight across race/ethnicity, gender, and grade. Am. J. Epidemiol. 175, 1284–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmonds M, Burch J, Llewellyn A, Griffiths C, Yang H, Owen C, Duffy S, Woolacott N, 2015. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: a systematic review and meta-analysis. Health Technol. Assess. 19, 1–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner AC, Perrin EM, Moss LA, Skelton JA, 2015. Cardiometabolic risks and severity of obesity in children and young adults. N. Engl. J. Med. 373, 1307–1317. [DOI] [PubMed] [Google Scholar]
- Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC, 2018. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp, 2017. Stata Statistical Software: Release, vol. 15 StataCorp LLC, College Station, TX. [Google Scholar]
- Sturm R, 2008. Disparities in the food environment surrounding US middle and high schools. Publ. Health 122, 681–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang X, Ohri-Vachaspati P, Abbott JK, Aggarwal R, Tulloch DL, Lloyd K, Yedidia MJ, 2014. Associations between food environment around schools and professionally measured weight status for middle and high school students. Child. Obes. 10, 511–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welker E, Lott M, Story M, 2016. The school food environment and obesity prevention: progress over the last decade. Curr. Obes. Rep. 5, 145–155. [DOI] [PubMed] [Google Scholar]
- White IR, Royston P, Wood AM, 2011. Multiple imputation using chained equations: issues and guidance for practice. Stat. Med. 30, 377–399. [DOI] [PubMed] [Google Scholar]
- Williams J, Scarborough P, Matthews A, Cowburn G, Foster C, Roberts N, Rayner M, 2014. A systematic review of the influence of the retail food environment around schools on obesity-related outcomes. Obes. Rev. 15, 359–374. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.