FIGURE 1.
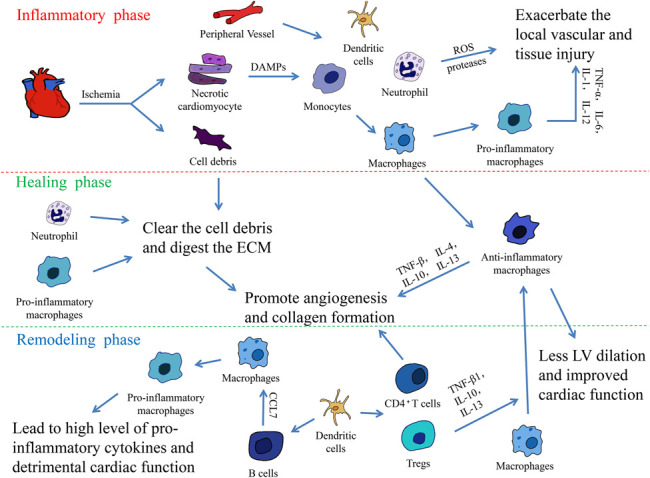
The 3 overlapping phases in the heart healing following MI. The inflammatory response following MI can be divided into 3 overlapping phases: The inflammatory, healing, and remodeling phases. In the inflammatory phase, the necrotic cardiomyocytes release DAMPs, HMGB1, extracellular RNA/eRNA, IL-1α, and other danger signals. These signals attract the innate immune cells, monocytes, neutrophils, and dendritic cells, which infiltrate into the infarct area from the peripheral vessels. At the early stage of MI, monocytes are quickly transformed into mature macrophages and they polarize into proinflammatory macrophages. The macrophages secrete various proinflammatory cytokines, including TNF-α, IL-1, IL-6, and IL-12, and contribute to the acute inflammatory response. Meanwhile, neutrophils generate high levels of reactive oxygen species and proteases, which exacerbates the injury of local vessels and tissue. After the inflammatory phase, neutrophils and proinflammatory monocytes promote the clearance of cell debris and digestion of ECM, preparing for wound healing. At the same time, local macrophages switch their phenotypic polarization to anti-inflammatory macrophages and promote angiogenesis and collagen formation via the secretion of anti-inflammatory cytokines, including TNF-β, IL-4, IL-10, and IL-13. At the terminal stage of MI, T and B lymphocytes massively infiltrate into the infarct area. Activated by DCs, CD4+ T cells facilitate wound healing of the myocardium, and regulatory CD4+ T cells (Tregs) improve healing after MI by producing TGF-β1, IL-13, and IL-10 to induce M2-like differentiation. The recruitment of B lymphocytes induces the mobilization of proinflammatory monocytes and leads to tissue injury and the deterioration of the myocardial function.
