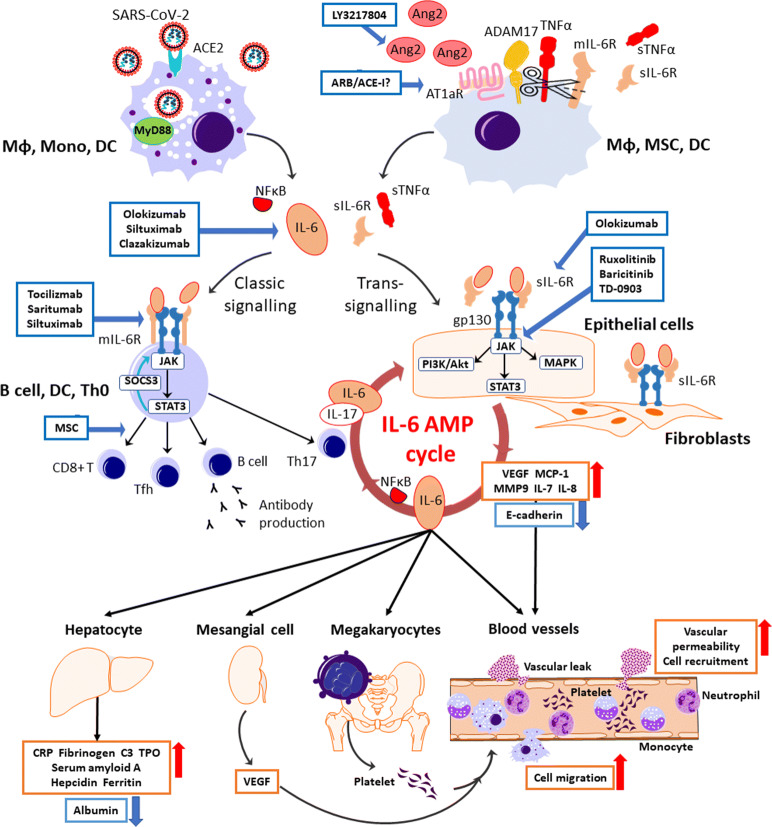
Fig. 2.
The therapeutics under clinical trials targeting the cytokine storm in SARS-CoV-2 infection. SARS-CoV-2 attaches to ACE2 and enters the host cell. Viral components are recognized by the MyD88 pathway in the endosome, leading to the releases of IL-6 and NFκB from immune cells including macrophages, monocytes, and dendrites. The possession of ACE2 by the virus causes the accumulation of Ang2 in the extracellular space. After the activation of AT1aR by excess Ang2 binding, sIL-6R is produced from the shedding of mIL-6R by ADAM10 and ADAM17 with a release of sTNFα from macrophages, mesenchymal stem cells (MSCs), and dendritic cells (DCs). IL-6 binds to the target cells via two signaling pathways: classic signaling only for specific immune cells, and trans-signaling for any cells including the immune cells, epithelial cells, and fibroblasts. In the classic signaling pathway, IL-6 binds to mIL-6R on the immune cells and activates B cells or differentiates CD8+ T cells, helper T cells, and Th17 cells, which triggers an anti-inflammation response. There is a negative feedback mechanism to the JAK-STAT pathway by SOCS3. In trans-signaling, IL-6/sIL-6R complex can bind to gp130 following the release of proinflammatory cytokines and IL-6 via three intracellular pathways without SOCS3 negative feedback. Since gp130 is highly expressed on almost all types of cells including the immune cells, sIL-6R shedding by ADAM17 provokes a surge of IL-surge mostly via trans-signaling. IL-6 stimulates the production of IL-6 and IL-17α from Th17 cells, resulting an IL-6 burst in its amplification cycle. The proinflammation cytokines increase vascular permeability and cell migration, enhancing the inflammation response. IL-6 also stimulates megakaryocytes, renal mesangial cells, and hepatocytes with the subsequent inflammatory response and vital organ injury. ARB/ACE-I, angiotensin receptor blocker/ACE2 inhibitor; AT1aR, angiotensin receptor subtype 1a; C3, complement component 3; E-cadherin, epithelial cadherin; gp130, glycoprotein 130; IL, interleukin; JAK, Janus kinase; MAPK, mitogen-activated protein kinase; MCP-1, monocyte chemoattractant protein 1; mIL-6R, membrane interleukin 6 receptor; MMP9, matrix metallopeptidase 9; MyD88, myeloid differentiation primary response 88; NFκB, nuclear factor kappa-light-chain-enhancer of activated B cells; NFκB, nuclear factor kappa B; PI3K/Akt, phosphoinositide-3-kinase/protein Kinase B; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; sIL-6R, soluble interleukin 6 receptor; SOCS3, the suppressor of cytokine signaling-3; STAT3, signal transducers and activators of transcription; sTNFα, soluble tumor necrosis factor alpha; Tfh, follicular helper T cell; Th0, naive T cell; Th17, T helper 17 cell; TMPRSS2, transmembrane protease serine 2; TNFα, tumor necrosis factor alpha; TPO, thrombopoietin; VEGF, vascular endothelial growth factor.