Fig. 2.
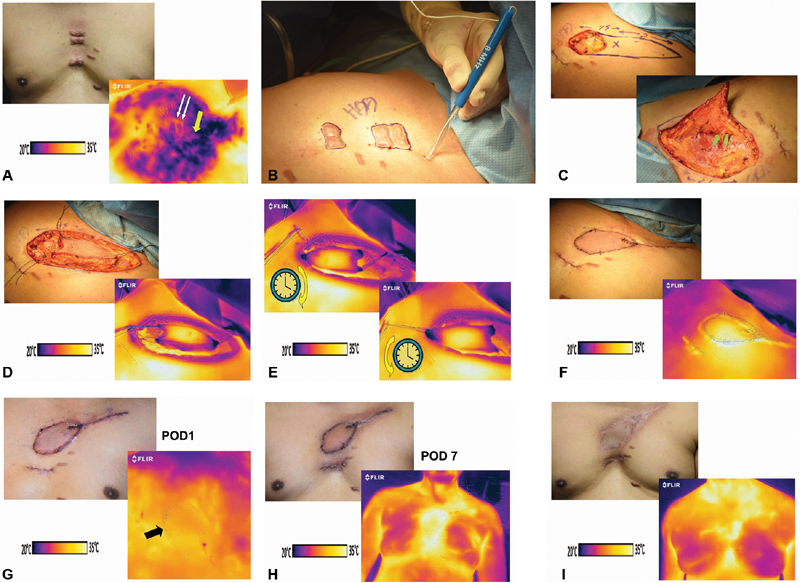
( A ) Painful midsternal keloids for planned excision (above) with “cold challenge” encompassing left second intercostal space that revealed a “hot spot” (yellow arrow) between left 2nd and 3rd ribs (white arrows show location of keloids; below). ( B ) Audible Doppler-confirmed presence of perforator at the marked “hot spot.” ( C ) Propeller flap designed using the identified perforator as hub (above), then precisely identified on green microgrid via exploratory incision (below). ( D ) Propeller flap in situ (above) and corresponding thermogram show dark color only at tips on either end, suggesting limited diminished perfusion (below). ( E ) Comparison of thermograms after clockwise rotation (above) and counterclockwise (below). The overall appearance revealed perhaps slightly larger area of darker colors after the clockwise rotation, so a counterclockwise rotation was performed. ( F ) Flap upon insetting had a slightly violaceous hue on clinical examination, suggesting venous congestion (above), but the thermogram had brilliant heterogenous colors throughout implying adequate perfusion at this time (below). ( G ) Minimal resolution of skin color on first postoperative day (above) with thermogram not quite as brilliant perhaps, but adequate (arrow = medial border of flap). ( H ) Skin color reflected a significant radiation effect at postoperative day 7 (above), yet with excellent sign of total flap perfusion on thermogram (below). ( I ) Satisfactory surgical defect coverage with left 2nd intercostal internal mammary artery perforator pedicled propeller flap at 3 months (above), and adequacy of perfusion of flap in midsternal region confirmed as expected by thermogram (below).
