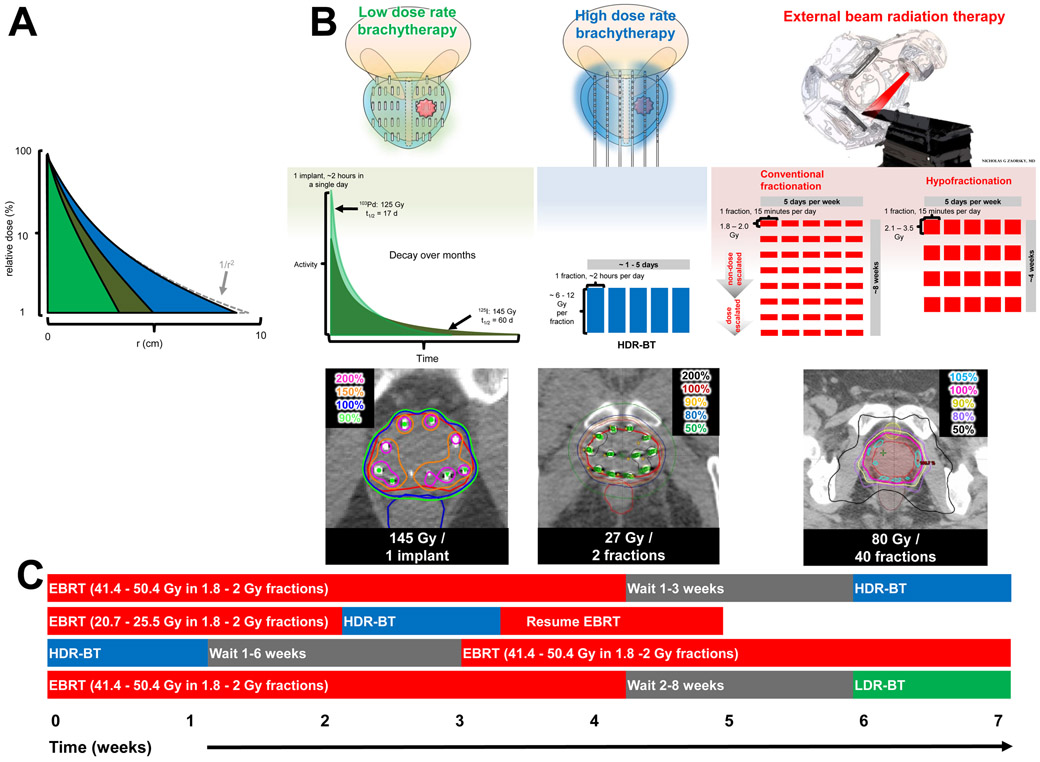
FIG 1 ∣. Comparison of LDR-BT, HDR-BT, and EBRT.
a∣ The dose distribution in water as a function of distance from a point source of three isotopes commonly used for prostate brachytherapy: LDR-BT with 103Pd (light green), LDR-BT with 125I (dark green), and HDR-BT with 192Ir (blue). The dose has been normalized to 100% at a distance of 1.0 cm (note log scale). The high energy 192Ir departs slightly from the inverse square law (1/r2), whereas the lower energy isotopes of LDR-BT have more absorption over a lower range. b∣ Comparison of LDR-BT, HDR-BT, and conventional or hypofractionated EBRT. The doses (with respect to the patient) are shown in colour (top panel). The dose fractionation of LDR-BT with decay using 103Pd (light green) or 125I (dark green) compared with HDR-BT (shown as blue fractions); and EBRT (red fractions) are shown in the middle panel. Notably, brachytherapy requires only 1–5 insertions compared with up to 40 fractions of EBRT. The isodose distributions (lower panel) of brachytherapy are superior to that of EBRT, as X-rays do not pass through the skin.
c∣ Brachytherapy boost is defined as the combination of EBRT with HDR-BT or LDR-BT. If EBRT is delivered first, HDR-BT is typically delivered 1–6 weeks later. A possible benefit of this method is to use the HDR-BT to account for suboptimal dosimetry of EBRT. Alternatively, EBRT can be interdigitated with HDR-BT. Finally, HDR-BT can be delivered first and EBRT delivered 1–3 weeks later.