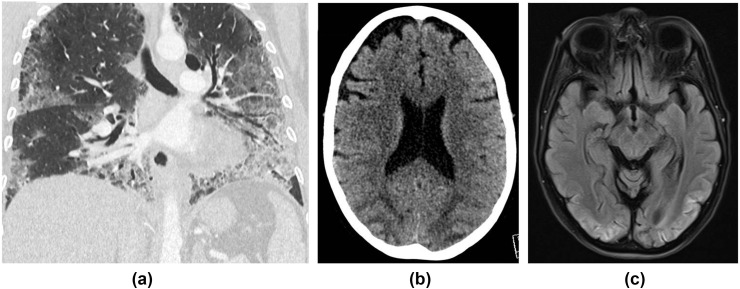
Figure 14.
A 53-year-old woman was admitted with a 2-week history of fever, cough, diarrhoea, and shortness of breath. She tested positive for COVID-19 and was ventilated for 2 weeks. (a) CT chest showed typical features of COVID-19 pneumonitis (peripheral basal ground glass with septal lines and bronchial dilatation). During her stay in critical care, she had a generalised tonic–clonic seizure. (b) CT head showed bilateral symmetrical occipital and posterior parietal low attenuation with sulcal effacement in keeping with oedema, which was confirmed on MRI (c), which showed corresponding high signal posteriorly on fluid-attenuated inversion recovery (FLAIR) sequences. A diagnosis of PRES was made. She remained delirious for a few days post-extubation, and was found to have cortical blindness on examination. She has made a good recovery since and is currently undergoing neuro-rehabilitation.