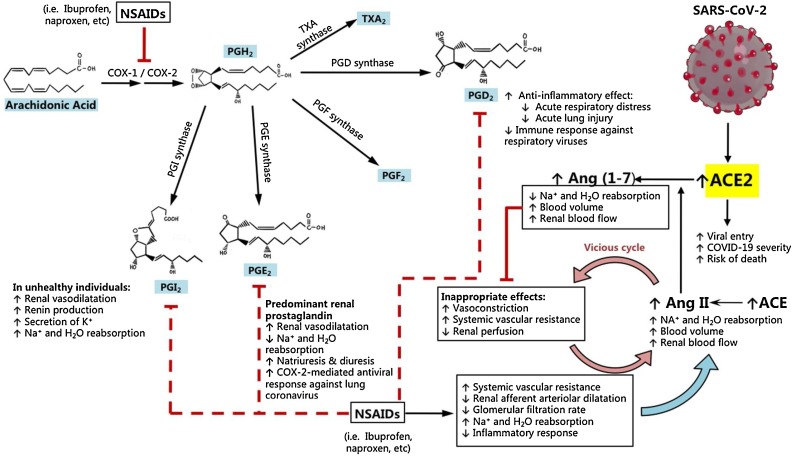
Fig. 2.
NSAIDs inhibit the synthesis of prostaglandins that protect against COVID-19. Arachidonic acid is converted to the prostaglandins and thromboxanes by the action of cyclooxygenases COX-1 and COX-2. Of the four prostaglandins, PGE2 and PGI2 promote optimal renal function by dilating afferent renal arterioles and promoting natriuresis in normal conditions, with PGI2-mediated Na+ and H2O reabsorption seen more evidently in unhealthy individuals with reduced renal perfusion. When NSAIDs like ibuprofen or naproxen are taken continuously, the net effects of COX inhibition are (1) increased Na+ and H2O reabsorption, (2) reduced renal afferent arteriolar dilatation, (3) reduced glomerular filtration rate (GFR), and (4) an increase in systemic vascular resistance. Due to reduced GFR and renal perfusion, the body produces greater amounts of angiotensin II (Ang II) to increase blood flow via increased plasma volume. However, increased Ang II levels leads to inappropriate vasoconstriction and increased systemic vascular resistance, which may ultimately result in a vicious cycle due to feedback compensation from Ang II in susceptible patients. Subsequently, an upregulation of ACE2 expression is expected to counteract Ang II providing its catabolic pathway to produce vasodilator and natriuretic angiotensins (1-7). This compensatory increase in ACE2 expression from NSAID intake, which is aggravated in unhealthy individuals such as those with hypertension, is the proposed mechanism by which SARS-CoV-2 can more aggressively infect the cell, by binding to greater amounts of ACE2 for viral entry. The concomitant immunosuppression by NSAIDs also promotes viral replication and shedding of SARS-CoV2, which can complicate the early phases of COVID-19.