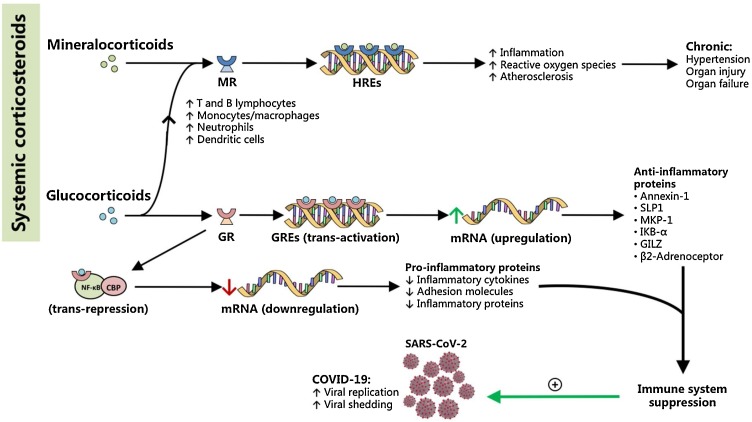
Fig. 4.
Corticosteroids mediate pro-inflammatory and anti-inflammatory pathways directed at the aggravation of COVID-19. Mineralocorticoids bind to nuclear mineralocorticoid receptors (MR) to interact with hormonal response elements (HREs), and are thought to mediate pro-inflammatory cascades that ultimately increase oxidative stress and contribute to pathologic inflammation and atherosclerosis. Chronic mineralocorticoid levels are thought to cause end-organ damage resulting in hypertension and end-organ failure. Meanwhile, glucocorticoids mediate anti-inflammatory pathways that result in the immunosuppressive actions of most corticosteroid drugs in medicine. Glucocorticoids bind to their nuclear glucocorticoid receptors (GR), but also to MR, and affect gene transcription via two important mechanisms: (1) transactivation, which is the direct interaction of the glucocorticoid-GR complex with genetic material, or (2) trans-repression, in which the complex interacts with other proteins such as CREB-binding protein (CBP) and NF-κB. Trans-activation leads to an upregulation of anti-inflammatory proteins, while trans-repression leads to decreased expression of inflammatory proteins. Together, these pathways converge to result in immunosuppression, which may aggravate COVID-19 by promoting SARS-CoV-2 replication and shedding, especially in the early stages of the disease. In effect, glucocorticoids as well as more specific therapies (i.e. monoclonal antibodies) may be better reserved for complications such as acute respiratory distress or acute lung inflammation where immunosuppression can be lifesaving.