Abstract
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is the cause of Coronavirus Disease (COVID-19) that has resulted in a global pandemic. At the time of writing, approximately 16.06 million cases have been reported worldwide. Like other coronaviruses, SARS-CoV-2 relies on the surface Spike glycoprotein to access the host cells, mainly through the interaction of its Receptor Binding Domain (RBD) with the host receptor Angiotensin-Converting Enzyme2 (ACE2). SARS-CoV-2 infection induces a profound downstream pro-inflammatory cytokine storm. This release of the pro-inflammatory cytokines is underpinning lung tissue damage, respiratory failure, and eventually multiple organ failure in COVID-19 patients. The phosphorylation status of ERK1/2 is positively correlated with virus load and ERK1/2 inhibition suppressed viral replication and viral infectivity. Therefore, molecular entities able to interfere with binding of the SARS-CoV-2 Spike protein to ACE2, or damping hyperinflammatory cytokines storm, blocking ERK1/2 phosphorylation have a great potential to inhibit viral entry along with viral infectivity. Herein, we report that the FDA-approved non-peptide opioid antagonist drug, naltrexone suppresses high fat/LPS induced pro-inflammatory cytokine release both from macrophage cells and Adipose Tissue Macrophage. Moreover, Low Dose Naltrexone (LDN) also showed its activity as an ERK1/2 inhibitor. Notably, virtual docking and simulation data also suggest LDN may disrupt the interaction of ACE2 with RBD. LDN may be considered as a target as the treatment and (or) adjuvant therapy for coronavirus infection. Clinical toxicity measurements may not be required for LDN since naltrexone was previously tested and is an approved drug by the FDA.
Communicated by Ramaswamy H. Sarma
Keywords: COVID-19, drug repurposing, molecular docking, naltrexone, SARS-CoV-2, structural bioinformatics
Introduction
Coronavirus Disease 2019 (COVID-19) is a major health concern, clinical symptoms of the disease vary from a mild illness, acute respiratory issues to multi-organ failure (Wang et al., 2020; Zaim et al., 2020). Older age, diabetes, cardiac diseases predict poor prognosis in COVID-19 patients (Fang et al., 2020; Madjid et al., 2020). Although much is known about the mortality of the COVID-19, however, details of the cellular responses to this virus are not known.
Several preclinical and clinical trials data have indicated an elevated cytokine/chemokine response in severe COVID-19 patients and identifies cytokine storm as the most potentially dangerous event for mortality (Coperchini et al., 2020; Rahmati & Moosavi, 2020; Zhang et al., 2020). Several kinases in the MAPK/ERK (mitogen-activated protein kinases/extracellular signal-regulated kinases) pathway are essential for viral replication. ERK1 and ERK2 phosphorylate HIV-1 proteins and enhance viral infectivity (Cai et al., 2007). The phosphorylation status of ERK1/2 is positively correlated with virus load and ERK1/2 inhibition suppressed viral replication and viral infectivity (Cai et al., 2007). Some preclinical findings have suggested targeting the ERK1/2 pathway to halt the viral replication and severity of SARS-COV-2 (Mizutani, 2010).
SARS-CoV-2 uses the homotrimeric spike glycoprotein as the main protein that interacts with the host by binding to host cell receptors (ACE2) to mediate virus invasion for cell entry. Some recent studies have highlighted the important role of ACE2 in mediating entry of SARS-CoV-2 (Hoffmann et al., 2020; Walls et al., 2020). A recent report also recognized several critical residues in RBD, including its Receptor-Binding Motif (RBM) that directly contacts with human ACE2 (Lan et al., 2020). An in-vitro study using HeLa cells also reinforced the role of ACE2 in mediating entry of SARS-CoV-2, where HeLa cells expressing ACE2 are susceptible to SARS-CoV-2 infection whereas those without ACE2 are not. Furthermore, in-vitro binding measurements, experiments showed that the SARS-CoV-2 RBD binds to ACE2 with an affinity in the nanomolar range, indicating that the RBD is a key functional component that is responsible for the binding of SARS-CoV-2 by ACE2 and can be considered as a target for the treatment of coronavirus infection to block SARS-CoV-2 from entering host cells (Lan et al., 2020; Walls et al., 2020).
There is a very fast ongoing search for therapeutics acting on SARS-CoV-2 (Hussain, 2020). Depending on the activity, the therapies can be divided into majorly main categories: (1) Inhibiting the viral RNA synthesis and replication, (2) Deterring the virus from binding to human cell ACE2 receptors, (3) Reinstating the innate immunity, and (4) Blocking the host’s specific receptors or enzymes. Despite many experimental and computational studies currently exploring all of these categories, to date, there is no confirmed effective treatment specifically available for COVID-19.
In this study, we report that the FDA-approved non-peptide opioid antagonist drug (Vickers & Jolly, 2006), naltrexone in low dose (LDN) suppresses high fat/LPS induced pro-inflammatory cytokine release both from macrophage cells and Adipose tissue macrophages (ATMs). The naltrexone is already an FDA approved drug and thus the pharmacology (pharmacokinetics and pharmacodynamics) of naltrexone is well known and reported elsewhere (Gonzalez & Brogden, 1988; Toljan and Vrooman, 2018). LDN also showed activity as an ERK1/2 inhibitor. Moreover, virtual docking and simulation data also suggest LDN may disrupt the interaction of ACE2 with RBD. As a reliable COVID-19 vaccine is unlikely to available before the maximal infection of COVID-19 has occurred, it is essential to establish therapeutics for the COVID-19 patients, based on our data, we proposed FDA-approved LDN can be used in combination or as an adjuvants therapy to treat mild to moderate symptomatic COVID-19 patients
Research design and methods
Drugs and chemicals
Naltrexone hydrochloride was obtained from MP Biomedicals (151725).
Cell lines and culture treatment
Murine macrophage (Raw264.7) cell line was cultured in RPMI media supplemented with 10% fetal bovine serum and 1% penicillin-streptomycin
Cell viability
Cell viability assay was carried out in Raw264.7 cells using MTT dye (3-(4, 5-dimethyl thiazol-2yl)-2, 5-diphenyl tetrazolium bromide) as reported earlier (Dogra et al., 2019). Cells were seeded in a 96-well plate and allowed to grow overnight. Further cells were treated with varying doses (0, 2, 5, 10, 15, 20, 30, and 40 µM) of the LDN for 24 h. Post-treatment, 10 µl of MTT (5 mg/ml stock in PBS) was added to all the wells. The formazan crystals thus formed were solubilized in 200 µl DMSO and the absorbance was recorded using (Infinite M200 Pro TECAN).
RNA isolation and gene expression profile
Raw264.7 cultured cells were treated with 5 μM of LDN in the presence and absence of LPS. RNA was isolated from the cells using RNA-Xpress reagent (HiMedia-MB601) and 1 µg of RNA was reverse-transcribed (using iScript cDNA Synthesis kit- Bio-Rad). Real time PCR was carried out following standard procedures using SYBR green (Bio-Rad) using mouse primers indicated in Supplementary table S4. Expression levels were calculated using the 2-ΔΔCT method with 18S rRNA as an internal control (Livak and Schmittgen, 2001).
Western blot analysis
Raw264.7 cultured cells were incubated with LDN (0 and 5 µM) in the presence or absence of LPS. After treatment, cells were lysed in RIPA buffer containing 1% protease- phosphatase inhibitors. Protein concentration was determined by BCA assay reagent as described in the manufacturer’s (Thermo Scientific-23227) manual. Protein was loaded on SDS-PAGE and electro-blotted on to PVDF membranes. The membrane was incubated in 5% milk blocking solution for 2 h at room temperature (RT) and probed against primary antibody (1:2000 diluted in TBST; After washing with TBST, the membrane was incubated with HRP conjugated IgG secondary antibody for 2 h and visualized by chemiluminescence. A list of antibodies is provided in supplemental experimental procedures (Table S3).
ATM isolation and analysis
Mice were euthanized chemically and epididymal fat was processed for isolation of ATM. 1 gram of adipose fat was rinsed in PBS and minced to small pieces in HEPES-DMEM buffer containing 10 mg/ml BSA. The suspension was centrifuged at 1000 g for 10 min and the resultant supernatant was pipette off to fresh tubes. 1 mg/ml of collagenase type-IV and 50 U/ml DNAse-II were added to this suspension and incubated at 37 °C for 45 mins with moderate shaking, filtered through 250-micron filter and the resultant solution was centrifuged again at 1000 g for 10 mins. Floating cells contained adipocyte and pellet are SVC. RBC lysis buffer was added gently to disrupt the sedimented pellets and centrifuged at 1000 g for 10 min at 4 °C. Fat macrophage cells were isolated by using BD IMag anti-mouse CD11b + magnetic beads through positive selection under the magnetic field. The percentage purity of macrophage isolation was determined by FACSCANTO II flow cytometer using APC tagged CD11b monoclonal antibody. The isolated macrophage was processed for RNA isolation, cDNA synthesis and various M1-M2 markers were evaluated using real-time PCR.
Structure preparation and molecular docking
The experimentally solved SARS CoV-2 RBD-ACE2 complex (PDB ID: 6M0J solved at 2.45 Å) was obtained from PDB (Lan et al., 2020). The ligand naltrexone (PubChem CID: 5360515) was extracted from the PubChem database. An attempt was made to dock to explore the binding mode of naltrexone onto the binding interface of the RBD-ACE2 complex using AutoDock version 4.2 (Morris et al., 2009) and AUTODOCK tools 1.5.6. Before docking, the protein was prepared by the removal of small molecules and waters. Then, polar-hydrogen atoms were added to the structure followed by Gasteiger charges calculation. Ligand centered map was generated with a spacing of 0.375 Å and grid dimensions of 46 × 46 × 46 Å3 (x-y-z) covering the biding interfaces residues (which includes the receptor-binding motif viz., RBM) of the complex (coordinates of central grid point of maps:-34.512, 20.978, 4.521). Default settings were used for all other parameters while performing docking with the number of GA run to 100. From the resultant docked conformations, the top-ranked conformation with the least free energy of binding, hydrogen-bonding and interatomic-bonding pattern was selected for further optimization by employing long term MD simulation. PyMOL (The PyMOL Molecular Graphics System, Version 2.0 Schrödinger, LLC.) and BIOVIA Discovery Studio Visualizer version4.5 were employed used to visualize the inter-molecular contacts between naltrexone with RBD-ACE2 complex.
In order to perform target prediction calculation and comparative analysis, we docked two reported inhibitors of ACE2 named SSAA09E2 (CID: 2738575) and Bisoctrizole (CID: 3571576) using the same parameters employed for naltrexone with ACE2-RBD complex through AutoDock (Adedeji et al., 2013; Patil, 2020).
Molecular dynamics simulation
To study the dynamic behavior, stability, and conformational flexibility RBD-ACE2- naltrexone complex, all-atoms MD simulations were performed as reported previously (Dehury et al., 2014; 2017; Girdhar et al., 2019). CHARMM36 force fields were used for topology building of protein in GROMACSv2019.4 package (Abraham et al., 2015). The ligand topology was derived from CHARMM General Force Field (https://cgenff.umaryland.edu/) (Vanommeslaeghe and MacKerell, 2012). The structure was solvated in a cubic water box in TIP3P water model. The system charge was electro-neutralized by adding 0.15 M NaCl to the solvated system. To eliminate bad contacts in the complex system energy minimization was done with the steepest descent algorithm in 5,000 steps. The non-hydrogen atoms of the ligands were restrained, and system equilibration was done in two steps including NVT and NPT ensembles in 10 ns at 300 K in atmospheric condition (1 atm). Finally, production MD was performed 100 ns at 300 K with a 2-femtosecond (fs) time step using Leapfrog integrator. The resultant trajectory was explored to understand the structural dynamics of the complex system through various utility toolkits of GROMACS. Stability parameters including backbone root mean square deviation (RMSD), the radius of gyration (Rg), Cα-root mean squared fluctuations (RMSF), and intermolecular hydrogen bond (H-bond) distributions were computed for the complex system. 2D graphs were plotted using XMGrace, while, interaction images were plotted using BIVIA DSV and PyMOL.
Statistical analysis
All the data presented is as mean ± SEM of three individual experiments unless specified. Comparisons between means were performed using Student t-test for unpaired data within two conditions.
Results
LDN treatment diminishes LPS induced cytokine storm
Cytokine storm is a very commonly observed factor in most severe COVID-19 patients and also one of the leading causes of mortality (Coperchini et al., 2020; Rahmati and Moosavi, 2020; Zhang et al., 2020). Peripheral blood of severe COVID-19 patients has also shown a high level of cytokine storm (Wu and Yang, 2020). Keeping in mind the ability of lipopolysaccharide (LPS) to cause sepsis and triggers an uncontrolled systemic inflammatory response in murine macrophage cells (Ramos-Benitez et al., 2018), we treated macrophage cells with LPS (1 µg/ml) in the presence and absence of LDN (5 µM). The dose of LDN chosen is non-toxic (Figure S2) as found in cell viability using MTT (4,5-dimethylthiazol-2-yl-2,5-diphenyltetrazolium bromide) assay following the standard protocol (Dogra et al., 2019).
Figure 2.
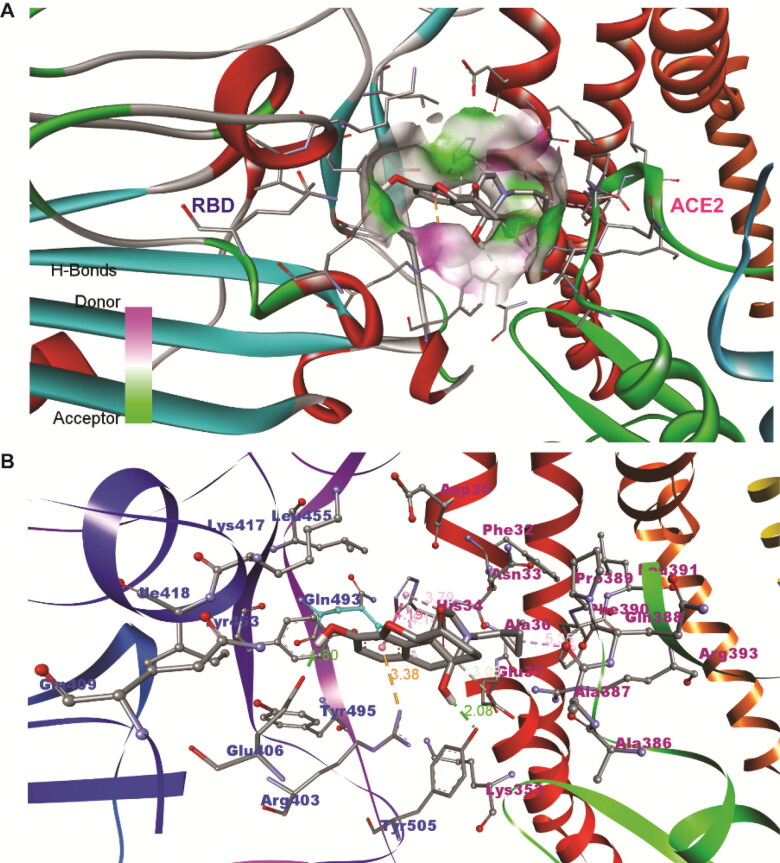
The docked conformation of naltrexone at the binding interface of RBD-ACE2 complex obtained from AutoDock (A) and interface amino acid residues involved in non-bonded contacts are labelled (B). The residues labeled in blue represent RBD and in pink are ACE2.
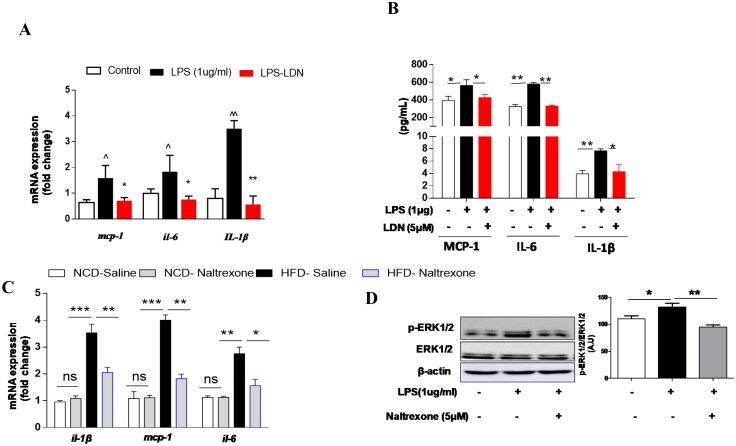
Results demonstrated that LPS treatment significantly induced expression on pro-inflammatory cytokines (IL-1β, IL-6 and mcp-1) whereas, LDN significantly inhibited LPS expression of IL-1β, IL-6 and mcp-1 in macrophage cells (Figure 1(A)). Next, we tested the possible involvement of LPS in inducing the release of pro-inflammatory cytokines, and we also determine the effects of LDN on release of pro-inflammatory mediators in LPS induced macrophage cells (Figure 1(B)). Conditioned media from LPS challenged macrophage cells showed a significantly enhanced release pro-inflammatory mediators (IL-1β, MCP-1 and IL-6) and interestingly we found that LDN treatment attenuated LPS induced IL-1β, MCP1 and IL-6 level (Figure 1(B)). These data suggest that LPS induced macrophage cells, to release - pro-inflammatory mediators, and LDN treatment can significantly abrogate LPS induced release of pro-inflammatory mediators in media. Adipose tissue macrophages (ATMs) is closely linked to this inflammatory condition which leads to numbers of diseases and the ability of High Fat Diet (HFD) feeding on increased LPS uptake and trafficking to macrophages and other targets are well known (Hersoug et al., 2016). Hence in this study, we investigated the effect of HFD on proinflammatory markers expression in purified ATMs. Expression of pro-inflammatory markers such as IL-1β, MCP-1 and IL-6 was induced (Figure 1(C)) whereas LDN attenuates HFD induced pro-inflammatory cytokines expression. Altogether, this data clearly shows that LDN treatment may protect (by reducing elevated M1 cytokines) against inflammation.
Figure 1.
(A) LDN prevents LPS induced pro-inflammatory cytokines expression and release Quantitative mRNA expression of indicated genes (mcp-1, il-6 and Il1b) in murine macrophage cells. (B) ELISA of pro-inflammatory proteins (MCP-1, IL-6 and IL-1β) in conditioned media from LPS challenged murine macrophage cells in the present and absence of LDN (C) Quantitative mRNA expression of IL-1β, mcp-1 and IL-6 in purified ATMs from all group mice. Values are expressed as mean ± SEM (n = 3) from three independent sets of repeats (mean ± SEM ***p < 0.001, **p, ^^p < 0.01 *p,^p < 0.05.) (D) LDN acts as EKR1 inhibitor and improved insulin sensitivity in LPS treated macrophage cells. ERK1/2 (Immunoblot) in RAW cells treated with LPS (1ug/ml) in the presence and absence of LDN.
LDN treatment attenuates LPS induced ERK1/2 phosphorylation
ERK1 and ERK2 mitogen-activated protein kinases (MAPK) play a critical role in the regulation of cell proliferation and differentiation in response to mitogens and other extracellular stimuli. Mitogens and cytokines that activate MAPK in cells have been shown to activate virus replication (Cai et al., 2007). The cytokine storm is a well-known factor that is increasing the severity and mortality in COVID19 (Coperchini et al., 2020; Rahmati and Moosavi, 2020; Zhang et al., 2020). Moreover, the phosphorylation status of ERK1/2 is positively correlated with virus load and reduced ERK1/2 phosphorylation suppressed viral replication significantly, thus reduced viral load (Cai et al., 2007). We pre-treated the cells with LDN and were exposed to LPS for 18 h. As shown in Figure 1(D), the phosphorylation of ERK 1/2 was increased after LPS exposure which was significantly suppressed by LDN treatment (Figure 1(D)). This finding suggests that LDN can acts as an inhibitor for ERK1/2 activation and may reduce the infectivity of virions.
In-silico studies revealed LDN interacts with the receptor-binding motif of SARS-CoV-2-RBD
The latest research shows that the spike-receptor binding domain (RBD) sequence of SARS-CoV-2 interacts with host receptor ACE2 and this RBD-ACE2 complex plays a key role in virus invasion and virulence. Based on the current research progress, the RBD-ACE2 complex is considered as a target for the treatment of coronavirus infection to block SARS-CoV-2 from entering host cells.
To understand the mode of interaction naltrexone in the binding interface of RBD-ACE2 complex, molecular docking was performed using AutoDock. The docking scores of the top ten complexes have been summarized in Table S1. As evidenced by the top-ranked conformation (as shown in Figure 2), the naltrexone prefers to bind in the cavity formed RBD and ACE2 receptor. Tyr505 and Glu406 of RBD formed two crucial hydrogen bonds with the naltrexone with an atomic distance of 2.08 and 1.80, while, Arg403 formed electrostatic contact. While the His34, Glu37, and Phe390 of ACE2 displayed several hydrophobic contacts (mostly pi-alkyl contacts) with naltrexone.
Further, we compared ACE2-RBD/Naltrexone binding affinity with some recently reported potential ACE2-RBD inhibitors. Both (SSAA09E2 and Bisoctrizole) displayed an affinity score of −6.7 kcal/mol and −8.5 kcal/mol respectively with the ACE2-RBD complex as compared to Naltrexone which shows an affinity score of −6.01 kcal mol−1 (Figure S3). Comparative analysis of docked conformation of two reported inhibitors as compared to Naltrexone revealed that the former two prefers to occupy the inner central cavity in ACE2-RBD complex (close to the N-terminus contact interface) and while Naltrexone occupied the core central surface with a greater number of contacts with the RBD of SARS Cov-2. As Naltrexone occupies the central interface of ACE2-RBD complex, thus, it can be expected to break a greater number of crucial contacts which in turn can inhibit the binding of RBD to host receptor ACE2. Further in-vitro and in-vivo studies are required to understand the efficacy of these compounds to understand the molecular basis of anti-coronavirus activity or inhibitory potential.
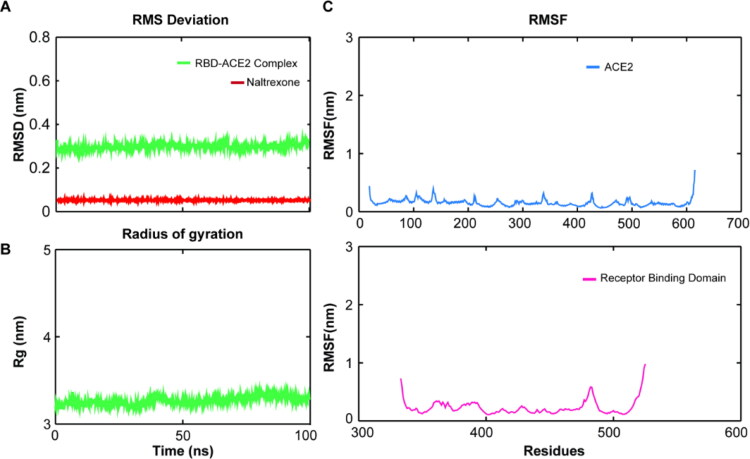
Figure 3.
Dynamics stability of RBD-ACE2-Naltrexone complex during 100 ns molecular dynamics simulation. (A) The root-mean square deviation (RMSD) of RBD-ACE2-Naltrexone complex during 100 ns MD in aqueous solution. (B) The compactness of the measured by the radius of gyration profile of complex with respect to time (C) The Cα-root mean squared fluctuation profile of the ACE2 and RBD during MD.
Trajectory analysis
The dynamics stability of the RBD-ACE2-naltrexone complex was analyzed by performing all-atoms MD simulations of 100 ns in GROMACS. The backbone RMSD analysis provides important information on the stability of protein and protein-ligand complexes and the time when simulation reached equilibrium. The RMSD of the RBD-ACE2-naltrexone complex displayed an average RMSD ∼2.46 Å throughout the entire simulation (Figure 3(A)). Besides, the RMSD of ligand was also found to be stable (red line in Figure 3(A)) with very minimal deviation as compared to the starting conformation. Overall, the complex system displayed the least backbone deviation, indicates that docked conformation is accurate and remained stable over the 100 ns timescale. Radiuses of gyration assess the compactness of the system, where a compact gyradius of ∼3.24 nm for the complex indicates the consistent shape and size of the system during the simulation (Figure 3(B)). The residue flexibility of protease and RBD-ACE2/Naltrexone complex was examined by performing Cα RMSF analysis of both the sub-units (Figure 3(C)). The average RMSF of ACE2 was found to be 0.14 nm, while for the RBD it was reported to be 0.17 nm (for the receptor-binding motif ∼0.16 nm). The receptor-binding motif of RBD displayed a high degree of flexibility and the residues participated in the ligand interaction also portrayed higher RMSF indicating their participation in ligand recognition.
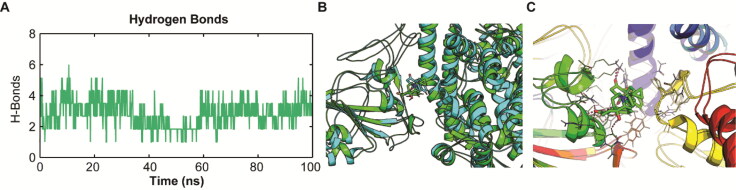
The intermolecular hydrogen bonds (H-bonds) between interacting atom pairs in a protein-ligand complex plays a vital role in the stability and molecular recognition process (Dehury et al., 2014). The intermolecular H-bonds were calculated with respect to time during the 100 ns MD simulation to see the dynamics stability RBD-ACE2-Naltrexone complex (Figure 4(A)). Though we observed an increased differential H-bonding during the initial 20 ns equilibration phase, however a stable trend with an average of ∼4.13 H-bonds are noticed from 60 to 100 ns. Close inspection of snapshots from MD revealed that some of the H-bonds were broken out during MD simulation, but at a later stage they well rewarded by new H-bonds, and hydrophobic contacts. This may be due to the structural re-orientation of ligand naltrexone in the binding pocket. The structural superposition of the docked complex with the cluster representative obtained from clustering analysis displayed Cα RMSD of 0.65 Å indicated that the complex retained its structural integrity throughout the simulation (Figure 4(B)). However, close observation of the ligand for the initial starting structure used MD revealed that the ligand tends to reorient within the binding site during MD (as shown in Figure 4(C)) but form a close tight network of hydrogen bonds and non-bonded contact with ACE and RBM of RBD. Analysis of the cluster representative revealed the crucial residues of RBD and ACE2 involved in the crucial interaction with naltrexone. Lys417 and Asp405 from RBD formed two hydrogen bonds with naltrexone, while Glu37 of ACE2-formed the lone hydrogen bond (Figure S2). Many electrostatic and hydrophobic contacts were also observed in the complex (Figure S2) where, Ile418, Gln409, and Tyr505 from RBD consistently formed close contact with ligand indicates their strong participation in the interaction mediated by naltrexone.
Figure 4.
Inter-molecular hydrogen bond dynamics and structural superposition of the initial complex with the simulated RBD-ACE2-naltrexone complex during 100 ns MD. (A) Dynamics stability of RBD-ACE2-naltrexone complex with respect to inter-molecular hydrogen bonds along the 100 ns time scale. (B) Structural superimposed view of the starting complex used for MD (green) and the snapshot obtained from clustering analysis (cyan) of MD trajectory during the last 50 ns. (C) Inter-molecular contacts of the docked complex and MD simulated complex.
Discussion
As a reliable COVID-19 vaccine is unlikely to available before the maximal infection of COVID-19 has occurred, it is essential to establish therapeutics for the individuals at moderate and high risk of the disease. So far, anti-viral medication is a major available option for COVID19 patients (Madjid et al., 2020). LDN which showed properties like anti-inflammatory, ERK1/2 inhibitory, and as well virtual docking and simulation data also suggested LDN may disrupt the interaction of ACE2 with RBD. LDN has been gaining credibility in its ability to halt the progression of several diseases without significant side effects when administered in low dosage ( Toljan and Vrooman, 2018; Younger et al., 2014; Low-Dose Naltrexone for Pruritus in Systemic Sclerosis, XXXX ).
Spike is the main structural protein of coronavirus and assembles into a special corolla structure on the surface of the virus as a trimer. Spike is the main protein that interacts with the host by binding to host cell receptors to mediate virus invasion (Walls et al., 2020). Spike is cleaved into S1 and S2 by the host cell protease like TMPRSS2, etc. The main function of S1 is to bind with host cell surface receptor; ACE2 and the S2 subunit mediates virus-cell and cell-cell membrane fusion (Walls et al., 2020). Spike structural integrity and cleavage activation play a key role in virus invasion and virulence (Lu et al., 2020; Walls et al., 2020). Therapeutic strategies to block coronavirus from entering host cells by targeting Spike proteins or specific receptors (ACE2) on the host surface are valuable for the development of anti-viral drugs (Hussain, 2020). It is anticipated that potential ACE2 inhibitors may not be suitable to use as drugs for treating SARS-CoV-2 infection because the poor prognosis would be induced by the inhibition of ACE2 enzyme activities, considering ACE2 is a protective role against lung injury. Recently, the crystal structure of the receptor-binding domain (RBD) of the spike protein of SARS-CoV-2 bound to the cell receptor ACE2 has been reported (Lan et al., 2020). Lan et al mentioned there are 13 hydrogen bonds at the SARS-CoV-2 RBD–ACE2 interface, this involves multiple tyrosine residues (Tyr436, Tyr449, Tyr489, and Tyr505) from the SARS-CoV-2 RBD to form hydrogen-bonding interactions with the polar hydroxyl group (Lan et al., 2020).
The latest research further strengthened that the spike-RBD sequence of SARS-CoV-2 interacts with host receptor ACE2 and this RBD-ACE2 complex plays a key role in virus invasion and virulence (Walls et al., 2020). Based on virtual screening results, LDN interacts with ACE2. Naltrexone prefers to bind in the central cavity formed SARS-CoV-2 RBD and ACE2 receptor. Tyr505 and Glu406 of RBD formed two crucial hydrogen bonds with the naltrexone with an atomic distance of 2.08 and 1.80, while, Arg403 formed electrostatic contact. While the His34, Glu37, and Phe390 of ACE2 displayed some hydrophobic contacts (mostly pi-alkyl contacts) with naltrexone. Overall this suggests LDN can strongly interact with SARS-CoV-2 RBD, including its RBM may further influence RDB- ACE2 binding, and host cell infectivity.
Therapeutic options for severe COVID-19 remain limited to date, immunomodulatory agents that directly target the crucial cytokines involved in COVID-19 may also help in alleviating hyperinflammation symptoms, mild and severe cases in particular(Zha, 2020). Corticosteroids are among the most commonly used drugs for immunomodulatory therapy of infectious diseases. However, the use of corticosteroids in the treatment of COVID-19 can cause host immune suppression and may delay viral clearance (Stockman et al., 2006). Combination of antibiotic, antiviral and steroid therapy exhibited respiratory failure and required non-invasive ventilation (Wu et al., 2020). Elevated plasma IL-6 levels have been reported and to be predictive of a fatal outcome in COVID-19 patients (Coperchini et al., 2020; Zhao, 2020). Other than corticosteroids, Tocilizumab, a specific monoclonal antibody that blocks IL-6, has been recommended for use in severe or critically ill patients. Tocilizumab specifically binds to IL-6 receptor and blocks its signaling cascade (Tanaka et al., 2016). However, clinical experience with tocilizumab in viral disease is very limited. Moreover, high costs and safety risks may be a barrier to the wide use of tocilizumab in the treatment of COVID-19.
Naltrexone hydrochloride is an FDA-approved non-peptide opioid antagonist (Cornish et al., 1997). In 1995, the FDA approved 50 mg naltrexone (ReVia) for the treatment of alcohol addiction. Low Dose Naltrexone (LDN; dose between 1 and 5 mg) is an immune-modulator, and a known TLR4 and opioid receptor antagonist (Cant et al., 2017; Hutchinson et al., 2008; Wang et al., 2016). Although naltrexone was synthesized as an orally active competitive opioid receptor antagonist, however, LDN exhibits paradoxical properties, including analgesia and anti-inflammatory actions, where, LDN simultaneously has an antagonist effect on non-opioid receptors (TLR4) which have not been reported at higher doses (Cant et al., 2017; Hutchinson et al., 2008; Wang et al., 2016; Younger et al., 2014). Unlike high doses of naltrexone, LDN has several mechanisms of action reported in the literature (The Uses of Low-Dose Naltrexone in Clinical Practice, 2020). LDN stimulates the release of β-endorphins by acting on the opioid receptor (Gold et al., 1982; The Uses of Low-Dose Naltrexone in Clinical Practice, 2020). LDN acts as a TLR4 antagonist, in a human pilot study (4.5 mg of LDN daily) significantly reduced serum pro-inflammatory cytokines (IL)-1, IL-2, IL-12, IL-18, etc (Parkitny and Younger, 2017). Importantly, low cost, low side effects, no reports of LDN interactions with other medications, and oral availability make LDN as a lucrative option to be used as an immunomodulatory agent and may be considered for use in combination with antiviral drugs or hydroxychloroquine for the treatment of severe or critical cases of COVID-19.
Our data provide a proof-of-concept for the potential feasibility of repurposing of FDA approved non-peptide opioid antagonist; naltrexone as host-targeted broad-spectrum antiviral therapies to combat COVID-19 infections. The next step will be to confirm data in COVID-19 patients. LDN alone or as an adjuvant therapy with hydroxychloroquine or an antiviral agent may give physicians more time to provide supportive treatment for patients with COVID-19.
Supplementary Material
Acknowledgements
We sincerely thank the BioX Centre of IIT Mandi for use of different analytical instruments. AC thank Department of Science & Technology (DST) INSPIRE fellowship, for his research fellowship. The authors received no funding from an external source.
Disclosure statement
No potential conflicts of interest relevant to this article were reported.
Author contributions
AC conducted the majority of the experiments and analyzed the data. BD and SK conducted in silico studies. PM, designed the study and supervised the project. PM and AC, wrote the manuscript with support from BD, SK and BM. PM is the guarantor of this work and, as such, has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- Abraham, M. J., Murtola, T., Schulz, R., Páll, S., Smith, J. C., Hess, B., & Lindahl, E. (2015). Gromacs: High performance molecular simulations through multi-level parallelism from laptops to supercomputers. SoftwareX, 1-2, 19–25. 10.1016/j.softx.2015.06.001 [DOI] [Google Scholar]
- Adedeji, A. O., Severson, W., Jonsson, C., Singh, K., Weiss, S. R., & Sarafianos, S. G. (2013). Novel inhibitors of severe acute respiratory syndrome coronavirus entry that act by three distinct mechanisms. Journal of Virology, 87(14), 8017–8028. 10.1128/JVI.00998-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai, Y., Liu, Y., & Zhang, X. (2007). Suppression of coronavirus replication by inhibition of the MEK signaling pathway. Journal of Virology, 81(2), 446–456. 10.1128/JVI.01705-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cant, R., Dalgleish, A. G., & Allen, R. L. (2017). Naltrexone inhibits IL-6 and TNFα production in human immune cell subsets following stimulation with ligands for intracellular toll-like receptors. Frontiers in Immunology, 8, 809. 10.3389/fimmu.2017.00809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coperchini, F., Chiovato, L., Croce, L., Magri, F., & Rotondi, M. (2020). The cytokine storm in COVID-19: An overview of the involvement of the chemokine/chemokine-receptor system. Cytokine & Growth Factor Reviews. 10.1016/j.cytogfr.2020.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornish, J. W., Metzger, D., Woody, G. E., Wilson, D., McLellan, A. T., Vandergrift, B., & O'Brien, C. P. (1997). Naltrexone pharmacotherapy for opioid dependent federal probationers. Journal of Substance Abuse Treatment, 14(6), 529–534. 10.1016/S0740-5472(97)00020-2 [DOI] [PubMed] [Google Scholar]
- Dehury, B., Behera, S. K., & Mahapatra, N. (2017). Structural dynamics of Casein Kinase I (CKI) from malarial parasite Plasmodium falciparum (Isolate 3D7): Insights from theoretical modelling and molecular simulations. Journal of Molecular Graphics & Modelling, 71, 154–166. 10.1016/j.jmgm.2016.11.012 [DOI] [PubMed] [Google Scholar]
- Dehury, B., Patra, M. C., Maharana, J., Sahu, J., Sen, P., Modi, M. K., Choudhury, M. D., & Barooah, M. (2014). Structure-based computational study of two disease resistance gene homologues (Hm1 and Hm2) in Maize (Zea mays L.) with implications in plant-pathogen interactions. PLoS One, 9(5), e97852. 10.1371/journal.pone.0097852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogra, S., Kar, A. K., Girdhar, K., Daniel, P. V., Chatterjee, S., Choubey, A., Ghosh, S., Patnaik, S., Ghosh, D., & Mondal, P. (2019). Zinc oxide nanoparticles attenuate hepatic steatosis development in high-fat-diet fed mice through activated AMPK signaling axis. Nanomedicine : nanotechnology, Biology, and Medicine, 17, 210–222. 10.1016/j.nano.2019.01.013 [DOI] [PubMed] [Google Scholar]
- Fang, L., Karakiulakis, G., & Roth, M. (2020). Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?. The Lancet. Respiratory Medicine, 8(4), e21. 10.1016/S2213-2600(20)30116-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girdhar, K., Dehury, B., Kumar Singh, M., Daniel, V. P., Choubey, A., Dogra, S., Kumar, S., & Mondal, P. (2019). Novel insights into the dynamics behavior of glucagon-like peptide-1 receptor with its small molecule agonists . Journal of Biomolecular Structure & Dynamics, 37(15), 3976–3986. 10.1080/07391102.2018.1532818 [DOI] [PubMed] [Google Scholar]
- Gold, M. S., Dackis, C. A., Pottash, A. L., Sternbach, H. H., Annitto, W. J., Martin, D., & Dackis, M. P. (1982). Naltrexone, opiate addiction, and endorphins. Med Res Rev, 2(3), 211–246. 10.1002/med.2610020302 [DOI] [PubMed] [Google Scholar]
- Gonzalez, J. P., & Brogden, R. N. (1988). Naltrexone. A review of its pharmacodynamic and pharmacokinetic properties and therapeutic efficacy in the management of opioid dependence. Drugs, 35(3), 192–213. 10.2165/00003495-198835030-00002 [DOI] [PubMed] [Google Scholar]
- Hersoug, L.-G., Møller, P., & Loft, S. (2016). Gut microbiota-derived lipopolysaccharide uptake and trafficking to adipose tissue: Implications for inflammation and obesity. Obesity Reviews : An Official Journal of the International Association for the Study of Obesity, 17(4), 297–312. 10.1111/obr.12370 [DOI] [PubMed] [Google Scholar]
- Hoffmann, M., Kleine-Weber, H., Schroeder, S., Krüger, N., Herrler, T., Erichsen, S., Schiergens, T. S., Herrler, G., Wu, N.-H., Nitsche, A., Müller, M. A., Drosten, C., & Pöhlmann, S. (2020). SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell, 181(2), 271–280.e8. 10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain, A. (2020). Targeting SARS-CoV2 spike protein receptor binding domain by therapeutic antibodies. Biomedicine and Pharmacotherapy, 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson, M. R., Zhang, Y., Brown, K., Coats, B. D., Shridhar, M., Sholar, P. W., Patel, S. J., Crysdale, N. Y., Harrison, J. A., Maier, S. F., Rice, K. C., & Watkins, L. R. (2008). Non-stereoselective reversal of neuropathic pain by naloxone and naltrexone: Involvement of toll-like receptor 4 (TLR4). The European Journal of Neuroscience, 28(1), 20–29. 10.1111/j.1460-9568.2008.06321.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan, J., Ge, J., Yu, J., Shan, S., Zhou, H., Fan, S., Zhang, Q., Shi, X., Wang, Q., Zhang, L., & Wang, X. (2020). Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature, 581(7807), 215–220. 10.1038/s41586-020-2180-5 [DOI] [PubMed] [Google Scholar]
- Li, Z., You, Y., Griffin, N., Feng, J., & Shan, F. (2018). Low-dose naltrexone (LDN): A promising treatment in immune-related diseases and cancer therapy. International Immunopharmacology, 61, 178–184. 10.1016/j.intimp.2018.05.020 [DOI] [PubMed] [Google Scholar]
- Livak, K. J., & Schmittgen, T. D. (2001). Analysis of Relative Gene Expression Data Using Real-Time Quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods (San Diego, Calif.).), 25(4), 402–408. 10.1006/meth.2001.1262 [DOI] [PubMed] [Google Scholar]
- Low-Dose Naltrexone for Pruritus in Systemic Sclerosis . https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3171757/. (Accessed 24th May 2020) [DOI] [PMC free article] [PubMed]
- Lu, R., Zhao, X., Li, J., Niu, P., Yang, B., Wu, H., Wang, W., Song, H., Huang, B., Zhu, N., Bi, Y., Ma, X., Zhan, F., Wang, L., Hu, T., Zhou, H., Hu, Z., Zhou, W., Zhao, L., … Tan, W. (2020). Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet (London, England), 395(10224), 565–574. 10.1016/S0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madjid, M., Safavi-Naeini, P., Solomon, S. D., & Vardeny, O. (2020). Potential effects of coronaviruses on the cardiovascular system: A review. JAMA Cardiology, 5(7), 831. 10.1001/jamacardio.2020.1286 [DOI] [PubMed] [Google Scholar]
- Mizutani, T. (2010). Signaling pathways of SARS-CoV in vitro and in vivo. Molecular Biology of the SARS-Coronavirus (pp. 305–322). Heidelberg, Berlin: Springer. 10.1007/978-3-642-03683-5_19 [DOI] [Google Scholar]
- Morris, G. M., Huey, R., Lindstrom, W., Sanner, M. F., Belew, R. K., Goodsell, D. S., & Olson, A. J. (2009). Software news and updates AutoDock4 and AutoDockTools4: Automated docking with selective receptor flexibility. Journal of Computational Chemistry, 30(16), 2785–2791. 10.1002/jcc.21256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkitny, L., & Younger, J. (2017). Reduced pro-inflammatory cytokines after eight weeks of low-dose naltrexone for fibromyalgia. Biomedicines, 5(4), 16. 10.3390/biomedicines5020016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patil, S. (2020). Drug repurposing for Covid-19: Discovery of potential small-molecule inhibitors of spike protein-ACE2 receptor interaction through virtual screening and consensus scoring. 10.26434/CHEMRXIV.12482435.V1 [DOI]
- Rahmati, M., & Moosavi, M. A. (2020). Letter to the editor cytokine-targeted therapy in severely ill COVID-19 patients: Options and cautions. Eurasian Journal of Medicine and Oncology, 4, 179–180. [Google Scholar]
- Ramos-Benitez, M. J., Ruiz-Jimenez, C., Rosado-Franco, J. J., Ramos-Pérez, W. D., Mendez, L. B., Osuna, A., & Espino, A. M. (2018). Fh15 blocks the lipopolysaccharide-induced cytokine storm while modulating peritoneal macrophage migration and CD38 expression within spleen macrophages in a mouse model of septic shock. mSphere, 3(6) e00548-18. 10.1128/mSphere.00548-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockman, L. J., Bellamy, R., & Garner, P. (2006). SARS: Systematic Review of Treatment Effects. PLoS Medicine, 3(9), e343. 10.1371/journal.pmed.0030343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka, T., Narazaki, M., & Kishimoto, T. (2016). Immunotherapeutic implications of IL-6 blockade for cytokine storm. Immunotherapy, 8(8), 959–970. 10.2217/imt-2016-0020 [DOI] [PubMed] [Google Scholar]
- The Uses of Low-Dose Naltrexone in Clinical Practice . (2020). Natural Medicine Journal. https://www.naturalmedicinejournal.com/journal/2018-04/uses-low-dose-naltrexone-clinical-practice.
- Toljan, K., & Vrooman, B. (2018). Low-Dose Naltrexone (LDN)—Review of Therapeutic Utilization. Medical Sciences, 6(4), 82. 10.3390/medsci6040082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanommeslaeghe, K., & MacKerell, A. D. (2012). Automation of the CHARMM general force field (CGenFF) I: Bond perception and atom typing. Journal of Chemical Information and Modeling, 52(12), 3144–3154. 10.1021/ci300363c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vickers, A. P., & Jolly, A. (2006). Naltrexone and problems in pain management. BMJ (Clinical Research ed.).), 332(7534), 132–133. 10.1136/bmj.332.7534.132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walls, A. C., Park, Y.-J., Tortorici, M. A., Wall, A., McGuire, A. T., & Veesler, D. (2020). Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell, 181(2), 281–292.e6. 10.1016/j.cell.2020.02.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, T., Du, Z., Zhu, F., Cao, Z., An, Y., Gao, Y., & Jiang, B. (2020). Comorbidities and multi-organ injuries in the treatment of COVID-19. The Lancet, 395(10228), e52. 10.1016/S0140-6736(20)30558-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, X., Zhang, Y., Peng, Y., Hutchinson, M. R., Rice, K. C., Yin, H., & Watkins, L. R. (2016). Pharmacological characterization of the opioid inactive isomers (+)-naltrexone and (+)-naloxone as antagonists of toll-like receptor 4. British Journal of Pharmacology, 173(5), 856–869. 10.1111/bph.13394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, D., & Yang, X. O. (2020). TH17 responses in cytokine storm of COVID-19: An emerging target of JAK2 inhibitor Fedratinib. Journal of Microbiology, Immunology and Infection, 108(1),17-41. 10.1016/j.jmii.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, F., Zhao, S., Yu, B., Chen, Y.-M., Wang, W., Song, Z.-G., Hu, Y., Tao, Z.-W., Tian, J.-H., Pei, Y.-Y., Yuan, M.-L., Zhang, Y.-L., Dai, F.-H., Liu, Y., Wang, Q.-M., Zheng, J.-J., Xu, L., Holmes, E. C., & Zhang, Y.-Z. (2020). A new coronavirus associated with human respiratory disease in China. Nature, 579(7798), 265–269. 10.1038/s41586-020-2008-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Younger, J., Parkitny, L., & McLain, D. (2014). The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain. Clinical Rheumatology, 33(4), 451–459. 10.1007/s10067-014-2517-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaim, S., Chong, J. H., Sankaranarayanan, V., & Harky, A. (2020). COVID-19 and multiorgan response. Current Problems in Cardiology, 45(8), 100618. 10.1016/j.cpcardiol.2020.100618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zha, L. (2020). Corticosteroid treatment of patients with coronavirus disease 2019 (COVID‐19. Medical Journal of Australia, 212, 416–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, W., Zhao, Y., Zhang, F., Wang, Q., Li, T., Liu, Z., Wang, J., Qin, Y., Zhang, X., Yan, X., Zeng, X., & Zhang, S. (2020). The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): The experience of clinical immunologists from China. Clinical Immunology (Orlando, Fla.), 214, 108393. 10.1016/j.clim.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, M. (2020). Cytokine storm and immunomodulatory therapy in COVID-19: Role of chloroquine and anti-IL-6 monoclonal antibodies. International Journal of Antimicrobial Agents, 55(6),105982. 10.1016/j.ijantimicag.2020.105982 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.