Abstract
Purpose
The study was to explore whether the 3-dimensional printing guiding plate system could facilitate the modified procedure for arthroscopic treatment of nondisplaced scaphoid nonunion.
Methods
Patients, diagnosed with scaphoid nonunion without displacement, were randomly assigned into two groups. In Group A, the 3-dimensional printing guiding plate system was used for guiding fixation during the surgery. In Group B, fixation was performed with intra-operative fluoroscopy. The bone operation time was recorded during the surgery. The patients were evaluated before surgery and followed-up after six post-operative months, including motion ratio, strength ratio, Visual Analogue Scale, modified Mayo Scores, Patient Rated Wrist Evaluation scores, plain radiography and CT scan.
Results
Sixteen patients were recruited for the study. The average bone operation time in Group A was statistically shorter than that in Group B.
Conclusions
3-dimensional printing technique-assisted arthroscopic bone graft and fixation of scaphoid nonunion constitute an effective and accurate clinical treatment option.
The translational potential of this article
The concept and technique of 3D printing assisted percutaneous fixation introduced in this paper have the potential to be applied in a variety of operations requiring accurate percutaneous fixation, especially for the joint injuries.
Keywords: 3D printing, Precise treatment, Scaphoid nonunion
Introduction
Scaphoid fracture is the most common fracture in the wrist, which accounts for 70% of all carpal fractures, and scaphoid nonunion is frequently seen because the initial injury is often ignored [1]. The fracture line without dislocation is often not obvious in plain radiography at the early stage, which causes a high risk of delays in the diagnosis and treatment, and might lead to scaphoid nonunion. Scaphoid nonunion is frequently seen as a serious bone fracture complication, which remains a challenge in clinical practice [2]. Some case series of scaphoid fracture reported a nonunion rate of 11–12.3% [3,4]. The commonly used clinical option of scaphoid nonunion is open surgery of internal fixation with iliac crest bone graft, but the blood supply of scaphoid might be damaged during open surgery, which might be a factor of reducing the healing rate [5]. The development of wrist arthroscopy has transformed the treating methods of many wrist diseases from open surgery to minimally invasive surgery [6]. Recently, wrist arthroscopy bone grafting technique has been designed for partial wrist fusion with percutaneous fixation of k-wires, which could be also applied for scaphoid nonunion [7]. However, fixation of the un-united scaphoid is a quite demanding technique without the open approach. The applications of 3-dimensional (3D) printing guiding plates designed according to the bone surface have made many open surgeries more precise and reduced the surgical trauma as well [8,9]. The 3D printing guiding system was also available for minimally invasive surgery if well designed according to the skin surface, such as a previous application in acute scaphoid fracture with one central screw fixation [10]. For scaphoid nonunion, application of the 3D printing technique would be more challenging, because an additional step of removing the fibrous tissue and sclerotic bone is needed and more fixation k-wires should be added. It is challenging for the 3D printing guide to introduce all the k-wires in the right direction and prevent them from influencing each other. Thus, we designed a modified procedure of arthroscopic treatment of nondisplaced scaphoid nonunion with the assistance of 3D printing technique and conducted a study to see whether this procedure could facilitate the surgery and improve the clinical results.
Methods
Study design
The protocol was approved by the institutional review board of a local hospital.
The inclusion criteria include patients aged from 20 to 60 years old, diagnosed with scaphoid nonunion without displacement or with mini-displacement. Scaphoid nonunion was diagnosed with apparently osteosclerosis or major cyst in the scaphoid fracture line, often first found in plain radiography and then confirmed in CT scanning [11]. According to the CT reconstruction, those patients, with a displacement of the scaphoid fragments longer than one fourth of the width of scaphoid waist, were excluded from the study. All patients provided written informed consent before data were collected.
Blocked randomisation with a block size of four was used in the study to assign the patients into two groups. The patients in both groups underwent arthroscopic bone graft and internal fixation, which were performed by the same senior professor. In Group A, the 3D printing technique was used to produce a guiding plate system for the purpose of accurate fixation of three k-wires. In Group B, fixation was performed without the guiding system. In both groups, both the arthroscopy and intra-operative fluoroscopy were used to check the position of the three k-wires.
Design and preparation of the 3D guiding plate system in Group A
CT scanning of 0.625 mm thickness was used to acquire as much 3D information of the wrist as possible. Patients were scanned in wrist extension position with the support of a short splint. In this posture, the wrist was extended and ulnar-deviated, and thumb was extended, which could make the trapezium moved to the dorsal side. Thus, the trapezium could be more likely spared from the fixation axes.
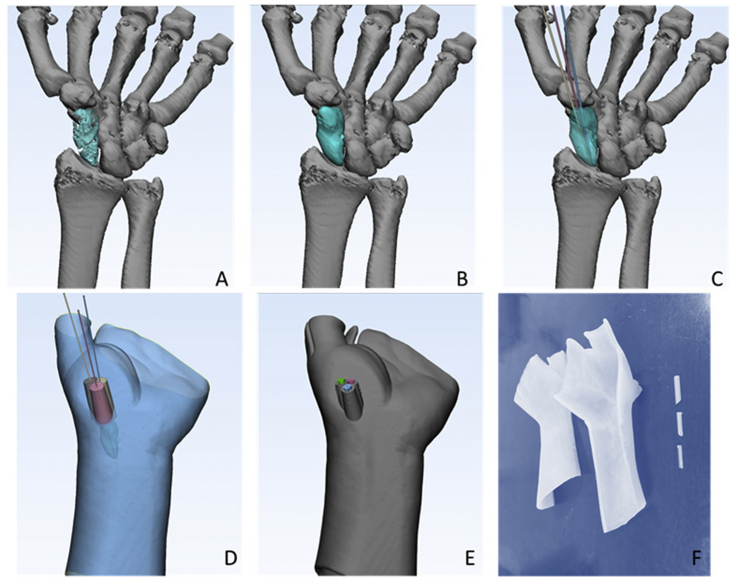
Digital Imaging and Communications in Medicine data were obtained and imported to the 3D designing software. The 3D guiding plate system was designed and prepared using the following procedure (Fig. 1).
Figure 1.
A, Bone reconstruction of the wrists showing obvious osteosclerosis and pseudarthrosis formed at the fracture line; B, signal enhancement of the scaphoid; C, location of the three fixing axes; D, three guiding tubes, with the length of 5 cm and cross-section inner diameter of 1.1 mm were designed; E, the percutaneous plate system was designed around the skin surface; F, guiding plate systems produced by the high-resolution 3D printing machine.
Both the shapes of bones and skin were reconstructed. Generally, the signal of scaphoid often showed significant osteoporosis and pseudarthrosis formed at the fracture line, which needed signal enhancement of the scaphoid in the reconstruction procedure to acquire a smooth surface. According to the location of the nonunion, three fixing axes were designed. Three guiding tubes, with the length of 5 cm and cross-section inner diameter of 1.1 mm, were designed according to these three fixing axes and then the percutaneous plate system was designed around the skin surface. The system included a volar plate, a dorsal plate and three removable tubes for the guide wire. Each patient in Group A had a specific-designed guiding plate system. A high-resolution 3D printing machine (Objet30 prime, Stratasys, MN, USA) was used to produce the guiding plate systems with a photopolymer of medical compatibility (MED610, Stratasys, MN, USA). It took about 24 h to print the guiding plate systems for each patient. The guiding plate systems were then checked by fitting the wrist of the specific patients and then underwent plasma sterilisation before the surgery. A video is attached to show how the plate system was designed (Video 1).
The following is the supplementary data related to this article:
Surgical procedure
The patients underwent general anaesthesia and lied in supine position with shoulder abduction. The tourniquet was used to temporarily stop the blood supply of the injured wrist.
In Group A, standard arthroscopy was first performed during the surgical procedure for debridement and checking the quality of the ligaments around the scaphoid, especially the radio-scapho-capitate ligament and the radio-lunate ligaments. Then, each part of the guiding plate system was set up to cover the volar and dorsal sides of the wrist. After being bundled with bandage, the arm was positioned as same as that for CT scanning. Three k-wires were slowly drilled into wrist through the guiding tubes in the plate system. The three tubes were removed and then the plate system could be taken off. Intra-operative fluoroscopy was used to confirm the position of the three k-wires.
The tips of three k-wires were retrograded to the fracture side, which allowed arthroscopic removing of the sclerotic bone. A motorised burr was used to remove the sclerotic bone at the site of pseudarthrosis. The tourniquet was deflated to see if there was new bleeding at the debrided site of scaphoid for regeneration.
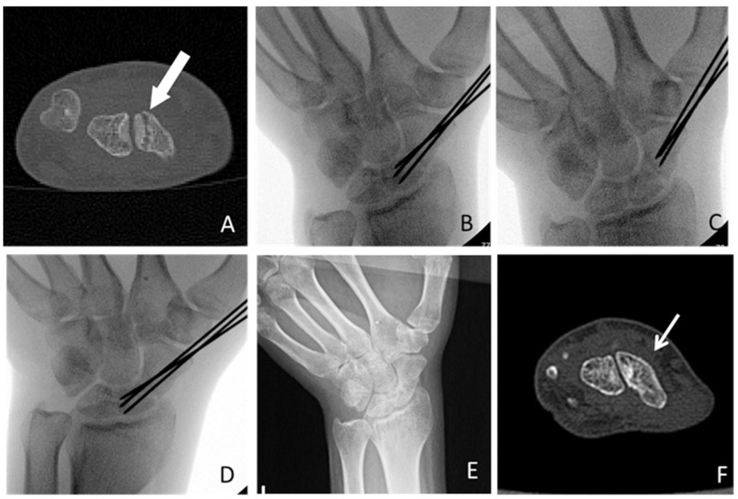
The guiding plate system was used again to wrap up the wrist and two of the three k-wires were drilled again into the proximal part of the scaphoid. Then the guiding plate system was taken off. Bone graft was harvested from the iliac bone and introduced through Scapho-Trapezio-Trapezoid (STT) portal by a trocar sheath with the camera at the mid-carpal radial (MCR) portal, which was called the Arthroscopic Bone Grafting (ABG) technique [7]. After bone grafting, the other k-wire was drilled into the proximal part of the scaphoid. Some bio-glue was injected to maintain the position of the bone graft. The three k-wires were buried beneath the skin. The main steps of intra-operative fluoroscopy, including the pre- and post-operative CT scan images, are represented in Fig. 2. A video is attached to demonstrate the surgical procedure (Video 2).
Figure 2.
A, Axial image of CT scanning showing scaphoid nonunion; B, intra-operative fluoroscopy showing the three k-wires in the right position as design; C, the tips of three k-wires were retrograded to the fracture side; D, after bone grafting, the k-wires were also drilled into the proximal part of the scaphoid; E, plain radiography at last follow-up showing scaphoid reunion; F, axial image of CT scanning at last follow-up showing scaphoid reunion.
The following is the supplementary data related to this article:
In Group B, standard arthroscopy and the ABG technique were also used. However, without a guiding plate, only intra-operative fluoroscopy was used repeatedly to check the position of the three k-wires.
Post-operative treatment
The patients wore a short arm splint for 8 weeks. Passive motion of the wrist began after the splint was removed. The three k-wires were removed after 12 weeks and then the active rehabilitation of the grip strength started.
Primary and secondary outcomes
The primary outcome is the reduction of bone operation time during the surgery, which started from drilling k-wires to the end of bone grafting. The secondary outcomes include the changes of motion ratio, strength ratio, Visual Analogue Scale, modified Mayo Scores and Patient Rated Wrist Evaluation (PRWE) scores. The patients were evaluated before the surgery as the baseline and then followed-up after six post-operative months. The evaluations were performed by a resident who was blinded about which procedure each patient was undergone because the incision was almost the same between Group A and Group B. Plain radiography was performed every three months. The CT scanning was performed after six months.
Statistical analysis
Student t test and proportion t test were used to compare respectively continuous variables and binary variables of the patients at baseline between the two groups. The mean of evaluations within each group was analysed with a paired t test. The changes of the evaluations were analysed with Student t test between the two groups. A p value of 0.05 was considered statistically significant.
Results
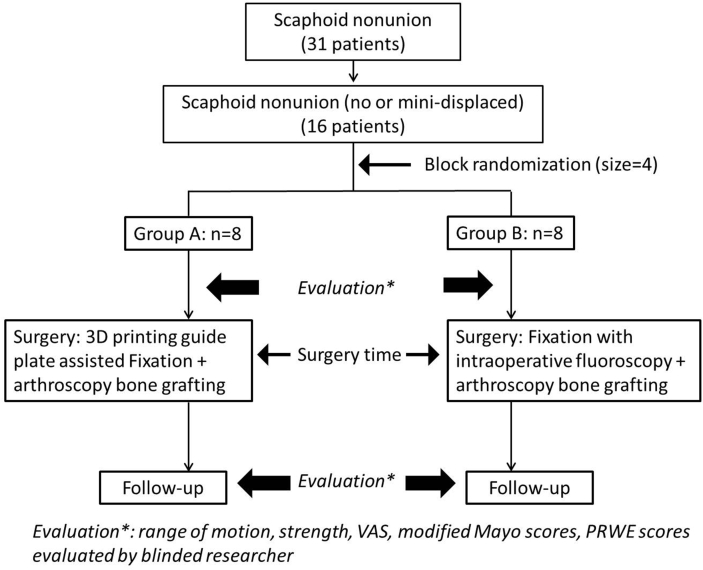
A consecutive series of 31 patients, diagnosed with scaphoid nonunion, were recruited in the clinic. Nine patients were excluded because of the existence of major displacement. Six patients were excluded because they had developed Scaphoid Nonunion Advanced Collapse (SNAC) wrists. Sixteen patients without displacement or with mini-displacement were included in this study. There were eight patients in Group A and eight patients in Group B (Fig. 3).
Figure 3.
Chart of patients flow.
In Group A, there were eight males, with an average age of 28.0 (SD 6.9) years. The scaphoid nonunion was found in six left wrists and two right wrists, with an injury-surgery duration of 5.2 (SD 6.5) years. In Group B, there were one female and seven males, with an average age of 35.0 (SD 10.0) years. The scaphoid nonunion was found in four left wrists and four right wrists, with an injury-surgery duration of 4.8 (SD 5.2) years. The characteristics of the patients at baseline are listed in Table 1.
Table 1.
Characteristics of the patients at baseline.
| Group | A (n = 8) | B (n = 8) | p value |
|---|---|---|---|
| Gender (female) | 0 (0%) | 1 (12.5%) | 0.30 |
| Age | 28.0 (SD 6.9) | 35.0 (SD 10.0) | 0.13 |
| Injured side (right) | 2 (25%) | 4 (50%) | 0.30 |
| Injury-surgery duration (year) | 5.2 (SD 6.5) | 4.8 (SD 5.2) | 0.90 |
| Injured/healthy side ratio of range of motion | |||
| Flexion-extension | 0.86 (SD 0.12) | 0.81 (SD 0.09) | 0.31 |
| Radio-ulnar deviation | 0.81 (SD 0.16) | 0.77 (SD 0.17) | 0.64 |
| Pronation-supination | 1.00 (SD 0.12) | 0.93 (SD 0.19) | 0.41 |
| Injured/healthy side ratio of strength | |||
| Grip strength | 0.77 (SD 0.18) | 0.64 (SD 0.23) | 0.24 |
| Pinch strength | 0.79 (SD 0.12) | 0.67 (SD 0.19) | 0.16 |
| Visual Analogue Scale | 5.16 (SD 2.00) | 5.90 (SD 1.76) | 0.45 |
| Modified Mayo Scores | 75.0 (SD 13.6) | 66.9 (SD 11.3) | 0.17 |
| PRWE Scores | 20.6 (SD 13.6) | 31.4 (SD 24.6) | 0.30 |
The average bone operation time was 69.4 (SD 15.3) minutes in Group A and 94.1 (SD 18.7) minutes in Group B, with statistical difference (p = 0.012 < 0.05). There is no statistical difference between Groups A and B about the changes of ROM ratios, strength ratios, or wrist function scores (Table 2). All the patients got scaphoid union within 6 months.
Table 2.
Changes of the means between groups A and B.
| Outcomes | Group A | Group B | p value |
|---|---|---|---|
| Bone operation time(minutes) | 69.4 (SD 15.3) | 94.1 (SD 18.7)a | 0.012 |
| Change of ROM ratio (injured/healthy) | |||
| Flexion-extension | −0.08 (SD 0.07) | −0.09 (SD 0.10) | 0.69 |
| Radio-ulnar deviation | −0.12 (SD 0.05) | −0.10 (SD 0.07) | 0.41 |
| Pronation-supination | −0.00 (SD 0.04) | 0.02 (SD 0.19) | 0.73 |
| Change of strength ratio (injured/healthy) | |||
| Grip strength | 0.11 (SD 0.18) | 0.15 (SD 0.16) | 0.70 |
| Pinch strength | 0.10 (SD 0.09) | 0.18 (SD 0.22) | 0.34 |
| Change of scores | |||
| Visual Analogue Scale | −4.20 (SD 2.06) | −4.17 (SD 1.47) | 0.98 |
| Modified Mayo scores | 9.4 (SD 9.8) | 5.6 (SD 12.7) | 0.52 |
| PRWE scores | −11.6 (SD 7.0) | −16.7 (SD 20.2) | 0.52 |
Statistical difference between groups.
The ROM ratios of flexion-extension and radio-ulnar deviation descended in both Groups A and B. The Visual Analogue Scale, modified Mayo Scores and Patient Rated Wrist Evaluation scores improved in both Groups A and B (Table 3).
Table 3.
Means at baseline and the last follow-up within each group.
| Outcomes | Group A |
Group B |
||
|---|---|---|---|---|
| Pre- | Post | Pre- | Post | |
| ROM ratio (injured/healthy) | ||||
| Flexion-extension | 0.86 (SD 0.12) | 0.78 (SD 0.12)a | 0.81 (SD 0.09) | 0.71 (SD 0.11)a |
| Radio-ulnar deviation | 0.81 (SD 0.16) | 0.68 (SD 0.14)a | 0.77 (SD 0.17) | 0.67 (SD 0.14)a |
| Pronation-supination | 1.00 (SD 0.12) | 1.00 (SD 0.12) | 0.93 (SD 0.19) | 0.95 (SD 0.05) |
| Strength ratio (injured/healthy) | ||||
| Grip strength | 0.77 (SD 0.18) | 0.88 (SD 0.09) | 0.64 (SD 0.23) | 0.79 (SD 0.12)a |
| Pinch strength | 0.79 (SD 0.12) | 0.89 (SD 0.07)a | 0.67 (SD 0.19) | 0.85 (SD 0.06) |
| Visual Analogue Scale | 5.16 (SD 2.00) | 0.96 (SD 0.60)a | 5.90 (SD 1.76) | 1.73 (SD 0.84)a |
| Modified Mayo scores | 75.0 (SD 13.6) | 84.4 (SD 7.8)a | 66.9 (SD 11.3) | 72.5 (SD 10.0) |
| PRWE scores | 20.6 (SD 13.6) | 9.0 (SD 7.0)a | 31.4 (SD 24.6) | 14.8 (SD 8.7) |
Statistical difference between groups.
Discussion
Comparison of characteristics of the patients at baseline indicated that the two groups are comparable. Scaphoid nonunion might be asymptomatic in a long time after fracture. In this case series, one patient had a wrist injury 20 years before, but he began to feel discomfort only recently two years before, with an asymptomatic period of eighteen years. Certainly, this kind of injuries needs to be treated to avoid developing of a SNAC wrist.
The bone operation time in Group A was significantly shorter than that in Group B, which demonstrated that the high-resolution 3D printing technique-assisted arthroscopic bone graft and fixation of scaphoid nonunion constitute an effective procedure in reducing the duration of the surgery.
It costed the 3D printing machine about 30 h for each patient to produce the 3D guiding plate system. The price of one 3D guiding plate system was about 300 US dollars, which was covered by the research fund. However, there is a reducing trend of the price of 3D printing materials. Thus, the 3D guiding plate system might be affordable for more patients in the near future.
There are many methods of fixation for the treatment of nonunion of scaphoid [[12], [13], [14]]. Removal of sclerotic bone, bone grafting and the protection of blood supply are commonly considered factors for a high reunion rate in the clinical practice. Internal fixation without bone grafting is only applicable to well-aligned scaphoid delayed unions and nonunions to achieve healing [15,16]. The reports on vascularised bone grafting using distal radial pedicle grafts vary greatly, rates ranging from 27% to 100% [[17], [18], [19]]. Traditional treatment of non-vascularised bone grafting for scaphoid nonunion can achieve union rates of 80%–90% [20,21]. In this study, all the patient achieved reunion, which might indicate that a combination of 3D printing and carpal arthroscopy makes the treatment of scaphoid nonunion more accurate and minimally invasive, which is conducive to the protection of scaphoid blood supply.
It is very important to consider how we should manage to stabilise the fracture after the debridement. During the surgical procedure of debridement, the quality of the ligaments around the scaphoid should be checked carefully, especially the radio-scapho-capitate ligament and the radio-lunate ligament. In most cases, the continuity of these stabilisers is fine. Besides, after debridement, the guiding plate system was used again to wrap up the wrist for the k-wires to be drilled again. The guiding plate system could control the direction of the k-wires again and put pressure on the wrist joint, which might be helpful to stabilise the fragment.
The indication of the 3D guiding plate system for scaphoid nonunion is no displacement or mini-displacement of the fragments, with intact ligaments around the scaphoid, which could be checked by arthroscopy. The thickness of the fat around the wrist is one of the main factors affecting accuracy of the percutaneous guide plate. Thus, obesity of the patients should be considered a relative contraindication. This kind of 3D guiding plate system is not yet available for fragment reduction. The limitation of the study might be the type of scaphoid nonunion was limited to no displacement or mini-displacement. However, according to our study, 51.6% (16/31) of the patients could be applicable for the technique. Another limitation of our study is that we did not include the degree of angulation deformity in the inclusion criteria.
In conclusion, 3D-printing assisted arthroscopic bone graft fixation of scaphoid nonunion is an effective clinical treatment option with a good union rate and wrist function recovery.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Nos. 81801941, 81525009 and 81830063), the Program of Shanghai Municipal Commission of Health and Family Planning (Grant No. 20164Y0018) and the Fudan University-SIBET Medical Engineering Joint Fund (Grant No. YG2017-012).
Conflict of interest
The authors have no conflicts of interest to disclose in relation to this article.
References
- 1.Janowski J., Coady C., Catalano L.W. Scaphoid fractures: nonunion and malunion. J Hand Surg Am. 2016;41(11):1087–1092. doi: 10.1016/j.jhsa.2016.08.019. [DOI] [PubMed] [Google Scholar]
- 2.Ding Z.C., Lin Y.K., Gan Y.K., Tang T.T. Molecular pathogenesis of fracture nonunion. J Orthop Translat. 2018;14:45–56. doi: 10.1016/j.jot.2018.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dias J.J., Brenkel I.J., Finlay D.B. Patterns of union in fractures of the waist of the scaphoid. J Bone Joint Surg. 1989;71B:307–310. doi: 10.1302/0301-620X.71B2.2925752. [DOI] [PubMed] [Google Scholar]
- 4.Geoghegan J.M., Woodruff M.J., Bhatia R., Dawson J.S., Kerslake R.W., Downing N.D. Undisplaced scaphoid waist fractures: is 4 weeks' immobilisation in a below-elbow cast sufficient if a week 4 CT scan suggests fracture union? J Hand Surg. 2009;34E:631–637. doi: 10.1177/1753193409105189. [DOI] [PubMed] [Google Scholar]
- 5.Buijze G.A., Ochtman L., Ring D. Management of scaphoid nonunion. J Hand Surg Am. 2012 May;37(5):1095–1100. doi: 10.1016/j.jhsa.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Ardouin L., Durand A., Gay A., Leroy M. Why do we use arthroscopy for distal radius fractures? Eur J Orthop Surg Traumatol. 2018;28(8):1505–1514. doi: 10.1007/s00590-018-2263-2. [DOI] [PubMed] [Google Scholar]
- 7.Ho P.C. Arthroscopic partial wrist fusion. Tech Hand Up Extrem Surg. 2008;12(4):242–265. doi: 10.1097/BTH.0b013e318190244b. [DOI] [PubMed] [Google Scholar]
- 8.Kaneyama S., Sugawara T., Sumi M. Safe and accurate midcervicalpedicle screw insertion procedure with the patient-specific screw guide template system. Spine. 2015;40(6):E341–E348. doi: 10.1097/BRS.0000000000000772. [DOI] [PubMed] [Google Scholar]
- 9.Mok S.W., Nizak R., Fu S.C., Ho K.K., Qin L., Saris D.B.F. From the printer: potential of three-dimensional printing for orthopaedic applications. J Orthop Translat. 2016;6:42–49. doi: 10.1016/j.jot.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yin H.W., Xu J., Xu W.D. 3-Dimensional printing-assisted percutaneous fixation for acute scaphoid fracture: 1-shot procedure. J Hand Surg Am. 2017;42(4):301.e1–301.e5. doi: 10.1016/j.jhsa.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 11.Lozano-Calderon S., Blazar P., Zurakowski D., Lee S.G., Ring D. Diagnosis of scaphoid fracture displacement with radiography and computed tomography. J Bone Joint Surg. 2006;88A:2695–2703. doi: 10.2106/JBJS.E.01211. [DOI] [PubMed] [Google Scholar]
- 12.Jones D.B., Jr., Burger H., Bishop A.T., Shin A.Y. Treatment of scaphoid waist nonunions with an avascular proximal pole and carpal collapse. A comparison of two vascularized bone grafts. J Bone Joint Surg. 2008;90A:2616–2625. doi: 10.2106/JBJS.G.01503. [DOI] [PubMed] [Google Scholar]
- 13.Waitayawinyu T., McCallister W.V., Katolik L.I., Schlenker J.D., Trumble T.E. Outcome after vascularized bone grafting of scaphoid nonunions with avascular necrosis. J Hand Surg. 2009;34A:387–394. doi: 10.1016/j.jhsa.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 14.Jones D.B., Jr., Moran S.L., Bishop A.T., Shin A.Y. Free-vascularized medial femoral condyle bone transfer in the treatment of scaphoid nonunions. Plast Reconstr Surg. 2010;125:1176–1184. doi: 10.1097/PRS.0b013e3181d1808c. [DOI] [PubMed] [Google Scholar]
- 15.Slade J.F., III, Geissler W.B., Gutow A.P., Merrell G.A. Percutaneous internal fixation of selected scaphoid nonunions with an arthroscopically assisted dorsal approach. J Bone Joint Surg. 2003;85A:20–32. doi: 10.2106/00004623-200300004-00003. [DOI] [PubMed] [Google Scholar]
- 16.Capo J.T., Orillaza N.S., Jr., Slade J.F., III Percutaneous management of scaphoid nonunions. Tech Hand Up Extrem Surg. 2009;13:23–29. doi: 10.1097/BTH.0b013e3181877644. [DOI] [PubMed] [Google Scholar]
- 17.Zaidemberg C., Siebert J.W., Angrigiani C. A new vascularized bone graft for scaphoid nonunion. J Hand Surg. 1991;16A:474–478. doi: 10.1016/0363-5023(91)90017-6. [DOI] [PubMed] [Google Scholar]
- 18.Steinmann S.P., Bishop A.T., Berger R.A. Use of the 1,2 intercompartmental supraretinacular artery as a vascularized pedicle bone graft for difficult scaphoid nonunion. J Hand Surg. 2002;27A:391–401. doi: 10.1053/jhsu.2002.32077. [DOI] [PubMed] [Google Scholar]
- 19.Straw R.G., Davis T.R., Dias J.J. Scaphoid nonunion: treatment with a pedicled vascularized bone graft based on the 1,2 intercompartmental supraretinacular branch of the radial artery. J Hand Surg. 2002;27B:413. doi: 10.1054/jhsb.2002.0808. [DOI] [PubMed] [Google Scholar]
- 20.Green D.P. The effect of avascular necrosis on Russe bone grafting for scaphoid nonunion. J Hand Surg. 1985;10A:597–605. doi: 10.1016/s0363-5023(85)80191-x. [DOI] [PubMed] [Google Scholar]
- 21.Barton N.J. Experience with scaphoid grafting. J Hand Surg. 1997;22B:153–160. doi: 10.1016/s0266-7681(97)80051-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.