Abstract
The relationship between mental health and receipt of social support is not well understood in low- and middle-income countries. In this paper, we focus on a cohort of older adults (40-plus) in rural South Africa to unpack associations between mental health and receipt of social support, and the extent to which marital status modifies these associations. We use baseline data from a population-based study, Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa (HAALSI), conducted between 2014 and 2015. Our results suggest that men and women who report depressive symptoms are less likely to receive social support: women are less likely to receive emotional and financial support, and men are less likely to receive physical and financial support. Both men and women who are married or partnered are more likely to receive social support than their non-married counterparts. The association between depressive symptomology and receipt of social support differs for women who are separated/divorced and for men who are widowed. Specifically, the association between having depressive symptoms and receiving physical or financial support is more positive for separated/divorced women than their married/cohabiting counterparts; for men, the association between having depressive symptoms and receiving physical support is more positive for widowed men than their married/cohabiting counterparts. Our findings speak to the complicated associations between social support, marriage and mental health in later life and the different experiences that men and women may have.
Keywords: Marriage, Sub-Saharan Africa, Health, Mental health, Depression, Social support
Highlights
-
•
We estimate links between mental health and receipt of social support among a cohort of aging adults in rural South Africa.
-
•
Having depressive symptoms is negatively associated with odds of receiving some types of social support for men and women.
-
•
Married men and women have greater odds of receiving all types of social support relative to non-married counterparts.
-
•
Depressive symptoms are more positively associated with receipt of physical support for widowed vs. married men.
-
•
Depressive symptoms more positively linked with receipt of physical or financial support for divorced vs. married women.
Introduction
Populations around the world are aging rapidly, increasing the importance of understanding the barriers to healthy aging among adults in lower- and middle-income countries (LMICs). An essential aspect of healthy aging is mental health, although this aspect of health is often overlooked. As people age, physical health and mobility limitations can lead to increased social isolation (Cornwell & Waite, 2009; Samson et al., 2000). Isolation can, in turn, increase the risk of depression while simultaneously decreasing access to informal social support (Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006; Holt-Lunstad, Smith, & Layton, 2010). This phenomenon is particularly concerning among rural populations in LMICs, where institutional support—especially mental health care—for older adults is lacking (Eaton et al., 2011; White & Sashidharan, 2018). For aging adults in these settings, limited institutional support makes access to social support from family and friends even more vital.
This paper investigates access to social support among a low-income population in rural South Africa. We use recent data from Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa (HAALSI) to understand how people who suffer from depressive symptoms fare in their receipt of social support (i.e., physical, emotional, or financial support) from within their social networks. We further investigate whether marital status modifies these associations, as marriage plays an important role in receipt of support (Ross & Mirowsky, 2002). We investigate these associations between marital status, mental health, and receipt of support separately for men and women, as there can be important gender differences in each of these factors (Kawachi & Berkman, 2001; Ross, 1995; Schone & Weinick, 1998). Our results can inform policies and interventions intended to reach individuals who lack the support they need from their social network.
Background
Setting
The population of adults on which we focus is from a cluster of rural villages in the northeast of South Africa, called Agincourt. South Africa is one of the fastest aging LMICs, with the United Nations predicting the population over age 65 to almost triple between 2020 and 2060 (United Nations, 2015). Not only is South Africa's older population increasing in size, it also faces an increasing burden of disease that includes endemic levels of HIV as well as a growing epidemic of non-communicable disease (Chang et al., 2019). Moreover, the majority of the residents of Agincourt and the entirety of our analytic sample are Black South Africans and, thus, continue to be directly affected by the legacy of apartheid (Collinson, Tollman, & Kahn, 2007).
Formal and informal social support
The South African government sponsors a formal system of support—the old age pension—which was extended to the Black population in the early 1990s. Currently, both men and women aged 60 and older are eligible to claim the pension (Ralston, Schatz, Menken, Gomez-Olive, & Tollman, 2015). Although eligibility is straight-forward, an estimated 20 to 30 percent of eligible people in Agincourt do not claim their pensions, due to barriers such as difficulty in travelling to claim it (Ralston et al., 2015).
These rural residents often create a web of financial support that combines formal support from social protection grants with informal support from family, especially, and friends (Booysen & Van der Berg, 2005; Cliggett, 2005). They tend to rely on informal networks of support for other needs, as well (Schatz & Seeley, 2015). With strong family ties and the prevalence of intergenerational households, social support is commonly available from within the household (Schatz, Madhavan, Collinson, Gomez-Olive, & Ralston, 2015). In the analyses to follow, we focus on support that comes from informal sources and is physical, emotional, or financial in nature.
Mental Health
Research suggests that, in high income countries, depression is most common among middle-aged adults and decreases at older ages (Blanchflower & Oswald, 2008; Steptoe, Deaton, & Stone, 2015), whereas in LMICs depression is most common in older populations and increases at advanced ages (Kohler, Payne, Bandawe, & Kohler, 2017). We see evidence of an increasing mental health burden among the aging population in South Africa (Jack et al., 2014). Prevalence of depressive symptoms in South Africa is lower than in the United States, but higher than in other parts of Africa (Tomlinson, Grimsrud, Stein, Williams, & Myer, 2009). In populations with high morbidity rates, like Agincourt, depression often arises as a comorbidity (Chang et al., 2019; Kohler et al., 2017). Factors such as food insecurity and low levels of education have also been found to be associated with higher rates of depression (Bishwajit, Kota, Buh, & Yaya, 2020; Tomlinson et al., 2009). In high poverty settings like Agincourt, the population is exposed to a number of factors that could increase risk for depression (Kohler et al., 2017). On the other hand, such a population may develop resilience in the face of these shocks.
Recent studies have found that 17 percent of adults aged 40 and older in Agincourt have at least three depressive symptoms, and older African women face greater risk than men (Geldsetzer et al., 2019; Kohler et al., 2017). Treatment options for mental health issues are limited in South Africa, particularly in rural areas like Agincourt (Jack et al., 2014), increasing the importance of informal support systems. If people combat the obstacles they face by creating protective social support networks, the negative effects on mental health and well-being may be tempered (Christian, Sanuade, Okyere, & Adjaye-Gbewonyo, 2020).
Marriage
South Africa has a distinctive marriage pattern compared with other countries in the region. Under apartheid, marriages and families were physically separated as a result of policies that prohibited African adults to reside in urban areas without employment (Hosegood, McGrath, & Moultrie, 2009). During this time, women entered the labor force in high numbers and female-headed households became common (Jaga, Arabandi, Bagraim, & Mdlongwa, 2018). With these changes came decreasing rates of marriage, along with increasing rates of non-marital cohabitation and marital dissolution (Budlender & Lund, 2011; Rudwick & Casale, 2011) that have persisted in the aftermath of apartheid (Budlender and Lund, 2011, Rudwick and Casale, 2011). In addition to the circulatory migration imposed by apartheid policies, the decline in marriage can also be attributed to the high cost of lobola payments that men are required to give to the wife's family prior to marriage (Rudwick & Casale, 2011). The high rate of unemployment of young men in Agincourt makes these payments difficult to achieve (Sennott, Reniers, xfmez, xeXavier, & Menken, 2016).
The HIV/AIDS epidemic has contributed to a high rate of widowhood (Hosegood et al., 2009). When marriages dissolve in this setting, it is most often the result of a spouse's death, rather than divorce (Amoateng, Richter, Makiwane, & Rama, 2004). In fact, about 30% of people in the HAALSI sample were widowed as of 2015, while 13% were separated or divorced (Jennings, Mkhwanazi, & Berkman, 2018, pp. 1–25). Remarriage is common, especially among men: In our data, among those who ever married, 41% of men and 9% of women had remarried.
Conceptual framework
The informal social support that a person receives may be responsive to their depressive symptoms, and this might differ by a person's marital status, as we discuss below. We conceptualize social support as help that one receives from within their social network (i.e., from the people with whom they interact on a regular basis), similar to the conceptualization of informal social support in other studies (Ross & Mirowsky, 2002; Schnittker, 2008). Our focus is on social support that provides physical, emotional, or financial resources.
Mental health and social support
People who experience depressive symptoms may have a greater need for social support. On one hand, their greater need for support may position them with greater odds of receiving support, either because they directly ask for it or because their friends and family perceive their need and, in turn, volunteer support. On the other hand, people who suffer from depressive symptoms may be more socially isolated, and so they may not have people in their lives from whom they feel they can request support. Furthermore, in South Africa and other LMICs, where mental health is not widely recognized as an important aspect of health (Jack et al., 2014; Kohler et al., 2017), friends and family may be less inclined to offer help to a person who struggles with mental health issues. For the same reason, a person who is depressed may be less inclined to express that they are suffering from these symptoms or that they need support.
The need for emotional support, in particular, is especially pertinent to people suffering from depressive symptoms. Emotional support can help them to feel less isolated and may mitigate their symptoms (Cramer, 2004; Ross et al., 2005). They may also have a less direct, but equally important, need for physical and financial support. Mental health limitations are often associated with physical limitations, especially among older people (Beekman et al., 1997; Beekman, Kriegsman, Deeg, & van Tilburg, 1995). Moreover, financial stress can contribute to depression (Mendes De Leon, Rapp, & Kasl, 1994), and experiencing depressive symptoms might also inhibit people's ability to financially support themselves. Hence, the need for each of these types of support (emotional, physical, and financial) may be heightened for people suffering from depressive symptoms.
The role of marital status
Based on research conducted mostly in Western settings, marriage is consistently associated with health benefits and can provide access to larger social networks (Waite & Gallagher, 2002; Zhu & Gu, 2010). One's marital status may affect whether having depressive symptoms impacts their receipt of social support. A married person has a built-in source of social support in their spouse, and may also have greater access to support through their in-laws and their spouses' friends (Cornwell, 2012; Kalmijn, 2003). Therefore, people who are married or partnered and suffer from mental health struggles may have the greatest odds of receiving social support.
Separated or divorced people are likely to have greater need for support. For example, Myroniuk (2017) found that older Malawians who have experienced a marital dissolution have worse physical and emotional health than currently married Malawians. Yet, people who have experienced a marital dissolution through divorce or separation may have limited availability of social support. A marital dissolution may result in the loss of in-laws and friends to rely on, in addition to the loss of spouse. Therefore, if a person who suffers from depressive symptoms is divorced or separated from their spouse, they may face lower odds of receiving social support than someone who is married.
Widows and widowers may have the greatest need for support, as some research has suggested that widowhood—especially among women—is associated with significant health decline (Bennett, 1997; Silverstein & Bengtson, 1994). A widowed person's social contacts may have a heightened awareness and, in turn, response to their need for social support. In fact, there is evidence from other settings that women get more support from their children following a husband's death than prior to that event (Connidis, 2001). However, there is evidence from this setting to suggest that widows may be disadvantaged in receipt of social support, as they may be blamed for their husband's death and cut off from social ties (Schatz, Madhavan, & Williams, 2011). Thus, we explore whether people who suffer from depressive symptoms are more or less likely to receive social support if they are widowed, compared with married people.
Gender differences in marriage, mental health, and social support
Gender is inextricably linked to the associations and experiences we have described here. Men tend to experience greater health advantages than women from marriage (Frech & Williams, 2007; Waite & Gallagher, 2002). Moreover, women tend to face greater risk of mental health issues than men (Kawachi & Berkman, 2001; Mirowsky, 1996). Finally, evidence suggests that women may have larger and more supportive networks than men (Antonucci & Akiyama, 1987; Carr & Bodnar-Deren, 2009), although there is evidence that South African men may have larger and more supportive friend networks than women (Amoateng et al., 2004; Jennings et al., 2018, pp. 1–25). In fact, there are particular reasons to expect gender differences in this setting, given the impact of apartheid policies on gender roles and sexual division of labor within marriages (Hosegood et al., 2009). Although we expect directions of the associations between depressive symptomology, marital status, and social support to be similar for men and women, their magnitudes may be different. For these reasons, our analyses are performed separately for men and women.
Data and methods
HAALSI is a cohort study of rural South Africans aged 40 and older at baseline. We use data from this baseline wave, collected between 2014 and 2015. The survey is population-based and aims to examine and characterize a population of older men and women in rural South Africa with respect to health, physical and cognitive function, aging, and well-being.
Participants were sampled from the existing framework of the Agincourt Health and Socio-Demographic Surveillance System (Agincourt HDSS) site in Mpumalanga province, a majority Black African area. A sample of 6281 people were randomly selected to participate in HAALSI; gender-specific sampling fractions were developed to ensure a gender-balanced cohort. Of these 6281 people, 391 had moved outside of the study site or were deceased. From the remaining 5890 eligible individuals, 5059 (86%) participated in the baseline survey. Interviews were conducted using Computer Assisted Personal Interviews (CAPI) in the local language, Shangaan. See Gómez-Olivé et al. (2018) for more detail on the study sample and design.
Measures
Dependent variables. We use measures of physical, emotional, and financial support as our dependent variables, coded from a series of survey items. Respondents were asked to name up to six adults, in order of importance, with whom they have been in communication (in person, by phone, or by internet) over the previous six months. If the respondent was married and did not name their spouse as one of the contacts then their spouse became an additional contact for them, resulting in a seventh contact. Next, respondents were asked how often they received (1) physical, (2) emotional, and (3) financial support over the previous six months. Physical support was described as “such as when you have needed help with chores around the house or at work, taking care of yourself or going from one place to another; ” emotional support as “such as when you are feeling sad or anxious or upset; ” and financial support as “such as borrowing money, receiving food, being given a job or anything else related to money or in-kind transfers.” Response options included “every day or almost every day,” “a few times per week,” “once per week,” “a few times per month,” “once per month,” “a few times in the past 6 months,” and “not at all.” We code measures of physical, emotional, or financial support as 1 if the person reported getting the respective type of support from any of their named social contacts at least a few times per month in the past six months, and 0 otherwise. If the respondent did not name any social contacts, they also received a code of 0.
Independent variables. To assess the association between depressive symptomology and social support we use the 8-item Center for Epidemiologic Studies Depression (CES-D) scale. The eight items included in our measure come from a series of survey questions that read “Much of the time in the past week, …” (1) “you felt depressed,” (2) “you put effort into everything you did” (this back-translation is slightly different from the original CES-D item), (3) “your sleep was restless,” (4) “you were happy,” (5) “you felt lonely,” (6) “you did not enjoy life,” (7) “you felt sad,” and (8) “you felt like doing nothing” (back-translation slightly different from original item). We considered a response of “yes” to be symptomatic in every case except “you felt happy,” for which we considered a response of “no” to be symptomatic. We code our independent measure as 1 if the respondent reported three or more symptoms and 0 otherwise, as done in other work using the 8-item CES-D (Glymour et al., 2012).
To investigate the modifying influence of marital status in the association between health and social support, we use a series of dummy variables to reflect marital status. These measures indicate whether the respondent (1) had never been married, (2) was currently married or living with a partner, (3) was separated/deserted or divorced, or (4) was widowed. We expect that formally married people will have similar access to social support as cohabiters, but the data do not allow us to distinguish between these two groups.
Covariates. We control for other factors that might affect receipt of social support. First, we control for the respondent's number of children, top-coded at 8. We also control for the number of times that the respondent has been married, top-coded at 3. Next, we control for the respondent's age. Age is coded into a series of five dummy variables to indicate decade of life, with the 80 or older coded as the oldest category. We also control for respondents' education, coded into three dummy variables that indicate that the respondent had (1) not completed formal education, (2) some primary or completed primary education, or (3) some secondary or higher education. Next, we control for respondents' primary employment status. These measures come from a survey item in which respondents could check as many response options as applicable to them. We coded primary employment status, reflecting that the respondent was (1) employed if they reported being employed, (2) household manager (originally meant to indicate “homemaker”, but translated to be understood as one who manages the home), if they did not report being employed but reported being a household manager (3) retired, if they did not report that they were employed or a household manager but reported being retired, or (4) not working, if they did not report being any of the previous statuses but reported that they were either unable to work, unemployed, or on leave from work.
We control for a series of five dummy variables that indicate household wealth quintiles. Households were ranked according to the scores from principal components analysis of household ownership of items such as televisions, refrigerators, livestock, and vehicles as well as housing characteristics, type of water and sanitation facilities (Filmer & Pritchett, 2001). We also control for a variable indicating that the respondent receives income from a pension based on employment, old age, or survivor benefits. We code this dummy variable as 1 if the respondent receives a pension, and 0 otherwise.
Next, we control for household characteristics. We account for the total number of people living in respondents’ household, top coded at 10. We also account for possible caregiving burden with controls for the number of household members under the age of 15, top coded at 5, and the number of household members above age 60, top coded at 3. Next, we control for a dummy measure indicating whether the respondent reported providing care to a family or household member, coded 1 if so and 0 if not.
We also control for a measure indicating the number of comorbidities that the respondent suffers from, including HIV (from blood samples), diabetes (either self-reported or confirmed in blood glucose), angina (self-reported), and/or hypertension (from blood pressure). Because many people are missing data on this comorbidity summary measure due to refusals related to HIV or inconclusive blood tests, we code missing as 0 and control for a dummy measure indicating whether the respondent is missing on comorbidities. As indicators of health behaviors, we also control for drinking and smoking behavior. This measure is coded 2 if the respondent smoked (ever) and consumed alcohol (in the last 30 days), 1 if they engaged in only one of these behaviors, and 0 if they engaged in neither behavior.
Lastly, because of evidence from this study that the timing of the interview, during the course of fieldwork, impacted interviewer-driven variability in respondents’ reporting of their social networks (Harling et al., 2018), we control for the month during which the interview was conducted.
Analytic approach
We use logistic regression to estimate the odds of depressive symptomology. We present results from logistic regression as odds ratios.
Results
Table 1 displays proportion or mean values for each of the variables used in our analyses, separately for men and women. The majority of both men and women received physical support (82% among women and 89% among men), emotional support (86% among women and 88% among men), or financial support (65% among women and 73% among men) from someone in their social network at least a few times a month in the six months preceding the interview. Slightly more women (18%) than men (15%) reported three or more depressive symptoms. Among women, nearly half (46%) are widowed, 37% are married or cohabiting, 13% are separated or divorced, and 4% never married. Among men, only 12% are widowed, 69% are married or cohabiting, 13% are separated or divorced, and about 7% never married.1
Table 1.
Descriptive statistics by sex.
| Proportion or Mean (S.D.) |
Min. | Max | ||
|---|---|---|---|---|
| Women | Men | |||
| Receipt of Social Support | ||||
| Physical | 0.82 | 0.89 | 0 | 1 |
| Emotional | 0.86 | 0.88 | 0 | 1 |
| Financial | 0.65 | 0.73 | 0 | 1 |
| Mental Health | ||||
| Depressive symptoms | 0.18 | 0.15 | 0 | 1 |
| Marital Status | ||||
| Married/cohabiting | 0.37 | 0.69 | 0 | 1 |
| Never married | 0.04 | 0.07 | 0 | 1 |
| Separated/divorced | 0.13 | 0.13 | 0 | 1 |
| Widowed | 0.46 | 0.12 | 0 | 1 |
| Controls | ||||
| Number of children | 4.27 (2.20) | 4.50 (2.49) | 0 | 8 |
| Number of times married | 1.04 (0.37) | 1.41 (0.74) | 0 | 3 |
| Age | ||||
| 40-49 | 0.19 | 0.18 | 0 | 1 |
| 50-59 | 0.29 | 0.27 | 0 | 1 |
| 60-69 | 0.25 | 0.28 | 0 | 1 |
| 70-79 | 0.16 | 0.19 | 0 | 1 |
| 80 and older | 0.11 | 0.08 | 0 | 1 |
| Education | ||||
| No formal | 0.49 | 0.40 | 0 | 1 |
| Primary | 0.33 | 0.36 | 0 | 1 |
| Secondary | 0.18 | 0.24 | 0 | 1 |
| Employment status | ||||
| Not working | 0.56 | 0.51 | 0 | 1 |
| Employed | 0.13 | 0.17 | 0 | 1 |
| Household manager | 0.13 | 0.08 | 0 | 1 |
| Retired | 0.19 | 0.23 | 0 | 1 |
| Wealth index | ||||
| Poorest | 0.20 | 0.21 | 0 | 1 |
| Poor | 0.20 | 0.19 | 0 | 1 |
| Middle | 0.20 | 0.19 | 0 | 1 |
| Less poor | 0.20 | 0.20 | 0 | 1 |
| Least poor | 0.20 | 0.21 | 0 | 1 |
| Receives income from a pension | 0.32 | 0.37 | ||
| Total number of household members | 5.24 (2.70) | 4.98 (2.86) | 1 | 10 |
| Number of permanent household members under age 15 | 1.87 (1.57) | 1.58 (1.57) | 0 | 5 |
| Number of permanent household members over age 60 | 0.71 (0.69) | 0.82 (0.81) | 0 | 3 |
| Provides care to family or household member | 0.27 | 0.16 | 0 | 1 |
| Comorbidities | 1.01 (0.65) | 0.89 (0.67) | 0 | 2 |
| Missing on comorbidities | 0.10 | 0.11 | 0 | 1 |
| Smoking and/or alcohol consumption | 0.11 (0.33) | 0.84 (0.78) | 0 | 2 |
| Interview month | 5.48 (3.02) | 5.85 (3.05) | 1 | 12 |
| N | 2604 | 2236 | ||
In Table 2 we use logistic regression to investigate the association between reporting depressive symptoms and receiving social support among women, adjusting for marital status and other relevant covariates. In Model 1, we find that having depressive symptoms does not significantly impact women's odds of receiving physical support. However, in Models 2 and 3, we find that women who have depressive symptoms are less likely to be receiving emotional or financial support than their non-depressive counterparts. Reporting depressive symptoms is associated with 25% reduced odds of emotional support and 17% reduced odds of financial support.
Table 2.
Odds ratios from logistic regression predicting receipt of social support among women.
| Model 1: Physical Support |
Model 2: Emotional Support |
Model 3: Financial Support |
||||
|---|---|---|---|---|---|---|
| Odds ratio | Z-score | Odds ratio | Z-score | Odds ratio | Z-score | |
| Mental Health | ||||||
| Depressive symptoms | 0.90 | −0.80 | 0.75+ | −1.90 | 0.83+ | −1.68 |
| Marital Status (Ref = Married/cohabiting) | ||||||
| Never married | 0.29*** | −3.68 | 0.42* | −2.22 | 0.48** | −2.65 |
| Separated/divorced | 0.54** | −3.21 | 0.39*** | −4.49 | 0.50*** | −4.68 |
| Widowed | 0.41*** | −5.76 | 0.36*** | −5.69 | 0.43*** | −7.14 |
| Controls | ||||||
| Number of children | 0.97 | −1.09 | 1.02 | 0.49 | 0.97 | −1.25 |
| Number of times married | 0.88 | −0.69 | 1.03 | 0.14 | 0.99 | −0.09 |
| Age (Ref = 40s) | ||||||
| 50-59 | 1.09 | 0.46 | 1.07 | 0.34 | 1.29+ | 1.88 |
| 60-69 | 0.66+ | −1.70 | 0.72 | −1.18 | 1.25 | 1.15 |
| 70-79 | 0.60+ | −1.91 | 0.56+ | −1.95 | 1.36 | 1.44 |
| 80 and older | 0.70 | −1.25 | 0.67 | −1.26 | 2.08** | 3.13 |
| Education (Ref = No formal) | ||||||
| Primary | 1.30* | 2.05 | 1.10 | 0.63 | 1.18 | 1.58 |
| Secondary | 1.18 | 0.86 | 0.70+ | −1.68 | 1.02 | 0.13 |
| Employment status (Ref = Not working) | ||||||
| Employed | 0.90 | −0.55 | 0.98 | −0.08 | 0.86 | −1.05 |
| Household manager | 0.40*** | −5.90 | 0.17*** | −11.09 | 0.44*** | −6.22 |
| Retired | 0.69* | −2.45 | 0.81 | −1.21 | 0.88 | −1.04 |
| Wealth index (Ref = Poorest) | ||||||
| Poor | 1.00 | −0.00 | 0.94 | −0.33 | 1.16 | 1.10 |
| Middle | 0.96 | −0.28 | 1.00 | 0.01 | 1.23 | 1.49 |
| Less poor | 0.95 | −0.28 | 0.87 | −0.74 | 0.92 | −0.60 |
| Least poor | 1.37 | 1.63 | 0.95 | −0.26 | 1.34+ | 1.91 |
| Receives income from a pension | 1.23 | 1.48 | 1.19 | 1.11 | 0.60*** | −4.41 |
| Total number of household members | 1.05 | 1.29 | 1.01 | 0.32 | 1.08* | 2.46 |
| Number of permanent household members under age 15 | 0.91 | −1.57 | 0.99 | −0.09 | 0.90* | −2.07 |
| Number of permanent household members over age 60 | 1.59*** | 3.53 | 1.32+ | 1.86 | 1.14 | 1.30 |
| Provides care to family or household member | 0.96 | −0.34 | 1.61** | 3.11 | 0.95 | −0.53 |
| Comorbidities | 0.97 | −0.33 | 1.03 | 0.26 | 0.92 | −1.24 |
| Missing on comorbidities | 0.87 | −0.80 | 0.71+ | −1.90 | 0.87 | −0.94 |
| Smoking and/or alcohol consumption | 1.30 | 1.58 | 1.76** | 2.71 | 1.15 | 1.06 |
| Interview month | 0.98 | −1.44 | 0.97 | −1.63 | 0.99 | −0.85 |
| N = 2604 | ||||||
Two-tailed tests, + p < .10, *p < .05, **P < .01, ***p < .001.
In Table 3 we investigate these same associations for men. We find that men who report suffering from depressive symptoms have significantly lower odds of receiving both physical and financial support, but not significantly different odds of receiving emotional support than men without these symptoms. Specifically, our models predict that men are 30% less likely to be receiving physical support and 46% less likely to be receiving financial support if they have depressive symptoms.
Table 3.
Odds ratios from logistic regression predicting receipt of social support among men.
| Model 1: Physical Support |
Model 2: Emotional Support |
Model 3: Financial Support |
||||
|---|---|---|---|---|---|---|
| Odds ratio | Z-score | Odds ratio | Z-score | Odds ratio | Z-score | |
| Mental Health | ||||||
| Depressive symptoms | 0.70+ | −1.86 | 1.07 | 0.35 | 0.54*** | −4.60 |
| Marital Status (Ref = Married/cohabiting) | ||||||
| Never married | 0.15*** | −5.60 | 0.30*** | −3.90 | 0.32*** | −4.68 |
| Separated/divorced | 0.15*** | −8.11 | 0.39*** | −4.32 | 0.37*** | −6.06 |
| Widowed | 0.15*** | −8.31 | 0.43*** | −3.89 | 0.27*** | −8.25 |
| Controls | ||||||
| Number of children | 1.08* | 2.13 | 1.03 | 0.82 | 1.01 | 0.32 |
| Number of times married | 1.07 | 0.54 | 1.13 | 1.03 | 0.84* | −2.19 |
| Age (Ref = 40s) | ||||||
| 50-59 | 2.01** | 3.05 | 1.17 | 0.74 | 1.18 | 1.01 |
| 60-69 | 0.94 | −0.21 | 1.05 | 0.16 | 1.72** | 2.62 |
| 70-79 | 1.12 | 0.35 | 0.85 | −0.53 | 1.94** | 2.80 |
| 80 and older | 1.13 | 0.30 | 1.23 | 0.53 | 1.99* | 2.48 |
| Education (Ref = No formal) | ||||||
| Primary | 0.82 | −1.11 | 1.06 | 0.34 | 1.08 | 0.60 |
| Secondary | 1.27 | 0.98 | 1.29 | 1.19 | 1.40* | 2.10 |
| Employment status (Ref = Not working) | ||||||
| Employed | 1.36 | 1.28 | 0.63* | −2.28 | 0.86 | −0.97 |
| Household manager | 0.85 | −0.56 | 0.12*** | −9.83 | 0.45*** | −4.43 |
| Retired | 1.08 | 0.37 | 1.04 | 0.17 | 0.96 | −0.31 |
| Wealth index (Ref = Poorest) | ||||||
| Poor | 1.02 | 0.11 | 0.94 | −0.30 | 1.22 | 1.29 |
| Middle | 1.12 | 0.48 | 1.21 | 0.85 | 1.35+ | 1.86 |
| Less poor | 0.97 | −0.13 | 0.97 | −0.14 | 1.23 | 1.27 |
| Least poor | 1.73+ | 1.85 | 0.90 | −0.43 | 1.45* | 2.13 |
| Receives income from a pension | 0.88 | −0.69 | 1.12 | 0.59 | 0.53*** | −4.79 |
| Total number of household members | 1.09 | 1.37 | 1.23*** | 3.58 | 1.09* | 2.21 |
| Number of permanent household members under age 15 | 1.01 | 0.07 | 0.81* | −2.17 | 0.88* | −2.09 |
| Number of permanent household members over age 60 | 1.70*** | 3.44 | 1.08 | 0.58 | 0.95 | −0.51 |
| Provides care to family or household member | 0.67 | −1.57 | 0.90 | −0.48 | 1.03 | 0.18 |
| Comorbidities | 0.96 | −0.32 | 1.20+ | 1.73 | 0.95 | −0.69 |
| Missing on comorbidities | 0.84 | −0.75 | 1.18 | 0.72 | 1.06 | 0.32 |
| Smoking and/or alcohol consumption | 1.14 | 1.31 | 1.07 | 0.76 | 1.12+ | 1.68 |
| Interview month | 1.00 | −0.06 | 1.02 | 0.88 | 0.99 | −0.40 |
| N = 2236 | ||||||
Two-tailed tests, + p < .10, *p < .05, **p < .01, ***p < .001.
To test whether the associations we find are limited to either younger or older respondents in our sample, we tested interactions between depressive symptoms and a variable indicating that the respondent was aged 65 or older (not shown). We found no significant differences in the associations between depressive symptoms and receipt of any type of social support for those aged 65 or older versus younger than 65, among men or women.
Table 2, Table 3 reveal significant associations between marital status and social support. As expected, both women and men who are married (the reference group) are more likely to receive support across the board than any of their non-married counterparts. In Table 4, Table 5 we investigate the role of marital status in modifying the association between depressive symptoms and social support for women and men, respectively. In Table 4 we find that, among women, being separated/divorced significantly modifies the association between having depressive symptoms and receipt of physical or financial support relative to being married/cohabiting (Models 1 and 3). We do not find interactions to be significantly associated with receipt of emotional support among women (Model 2).
Table 4.
Odds ratios from logistic regression predicting receipt of social support among women, interactions with marital status.
| Model 1: Physical Support |
Model 2: Emotional Support |
Model 3: Financial Support |
||||
|---|---|---|---|---|---|---|
| Odds ratio | Z-score | Odds ratio | Z-score | Odds ratio | Z-score | |
| Interactions | ||||||
| Separated/divorced * Depressive symptoms | 2.61+ | 1.76 | 1.13 | 0.22 | 2.23* | 2.09 |
| Widowed * Depressive symptoms | 1.04 | 0.12 | 0.66 | −1.02 | 0.95 | −0.20 |
| Mental Health | ||||||
| Depressive symptoms | 0.79 | −0.82 | 0.97 | −0.07 | 0.77 | −1.26 |
| Marital Status (Ref = Married/cohabiting) | ||||||
| Never married | 0.29*** | −3.65 | 0.43* | −2.17 | 0.49** | −2.62 |
| Separated/divorced | 0.47*** | −3.69 | 0.37*** | −4.36 | 0.44*** | −5.16 |
| Widowed | 0.41*** | −5.42 | 0.39*** | −5.04 | 0.44*** | −6.60 |
| N = 2604 | ||||||
Table 5.
Odds ratios from logistic regression predicting receipt of social support among men, interactions with marital status.
| Model 1: Physical Support |
Model 2: Emotional Support |
Model 3: Financial Support |
||||
|---|---|---|---|---|---|---|
| Odds ratio | Z-score | Odds ratio | Z-score | Odds ratio | Z-score | |
| Interactions | ||||||
| Separated/divorced * Depressive symptoms | 1.33 | 0.64 | 0.84 | −0.36 | 1.42 | 1.00 |
| Widowed * Depressive symptoms | 2.13+ | 1.68 | 0.80 | −0.47 | 1.09 | 0.25 |
| Mental Health | ||||||
| Depressive symptoms | 0.51* | −2.31 | 1.18 | 0.60 | 0.50*** | −4.21 |
| Marital Status (Ref = Married/cohabiting) | ||||||
| Never married | 0.15*** | −5.62 | 0.30*** | −3.91 | 0.32*** | −4.68 |
| Separated/divorced | 0.14*** | −7.75 | 0.40*** | −3.96 | 0.35*** | −6.00 |
| Widowed | 0.13*** | −8.28 | 0.45*** | −3.39 | 0.27*** | −7.52 |
| N = 2236 | ||||||
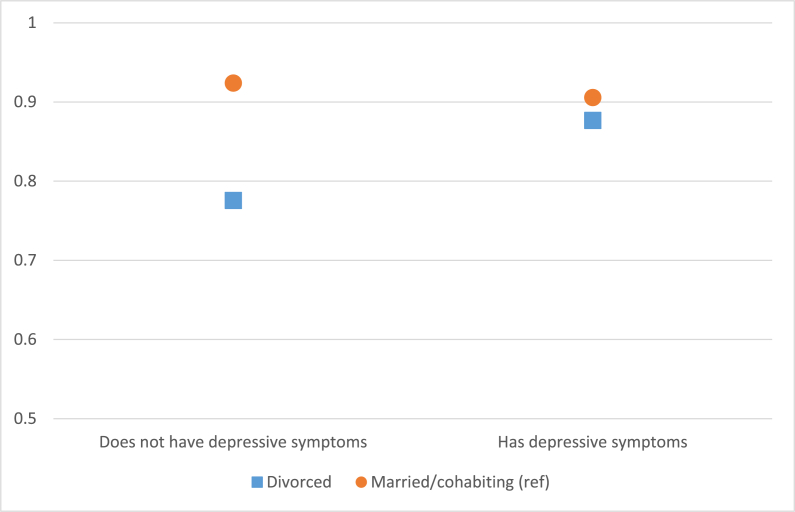
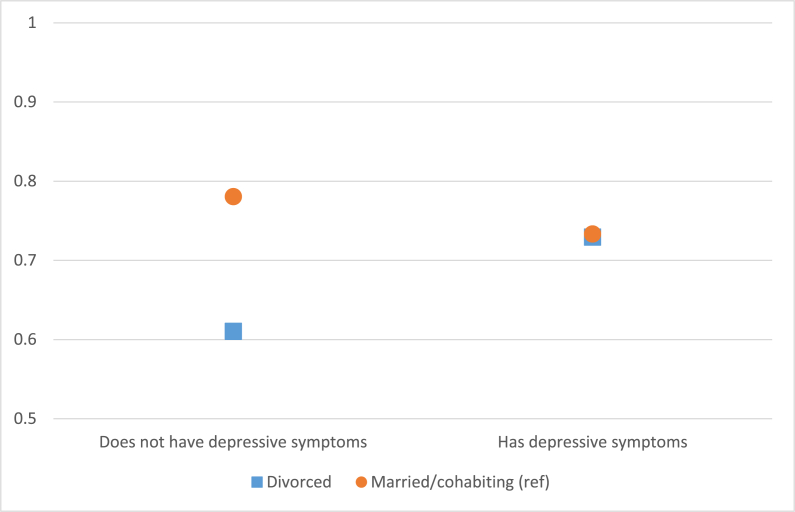
Fig. 1, Fig. 2 illustrate these interactions with plots of the predicted probabilities associated with the odds of receiving physical and financial support, respectively. Fig. 1 shows that the association between having depressive symptoms and receiving physical support is more positive for separated/divorced women than for the reference category of married/cohabiting women, but there is little difference in receipt of physical support for women with depressive symptoms of either marital status. In Fig. 2, we find that a similar pattern holds for women's receipt of financial support.
Fig. 1.
Predicted probabilities of receipt of physical support from interaction between being separated/divorced and having depressive symptoms among women.
Fig. 2.
Predicted probabilities of receipt of financial support from interaction between being separated/divorced and having depressive symptoms among women.
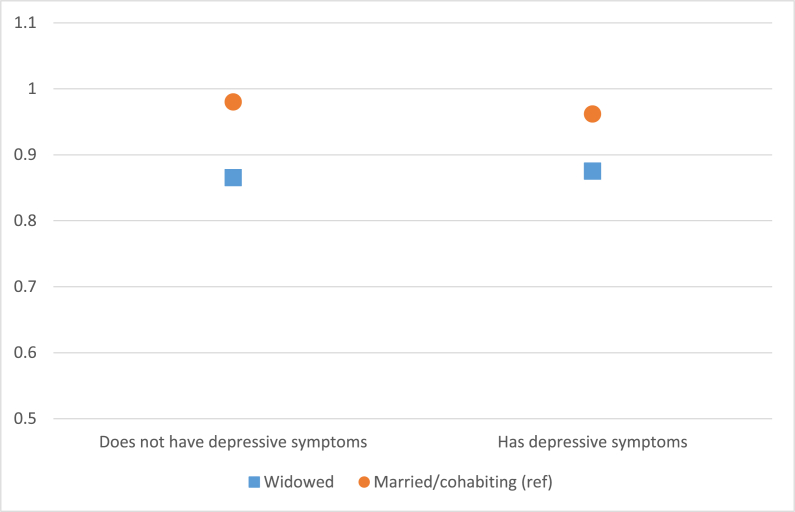
In Table 5, we investigate the modifying role of marital status in the association between depressive symptoms and social support for men. We find no significant differences between marital status and depressive symptoms in men's odds of receiving emotional or financial support, but we find evidence of a significant association in the interaction between widowhood and depressive symptoms on receipt of physical support. Fig. 3 illustrates this interaction, which mirrors the pattern for separated/divorced women: Men who are widowed experience a more positive association between depressive symptoms and receipt of physical support than men who are married.2
Fig. 3.
Predicted probabilities of receipt of physical support from interaction between widowhood and having depressive symptoms among men.
Discussion
Demographic shifts coupled with economic and social changes in LMICs have raised questions about who is likely to receive social support in advanced age. We use some of the highest quality data in the region on social networks and mental health to investigate the predictors of receiving social support among adults aged 40 years and older in rural South Africa. We find an important gendered narrative between depressive symptoms, marital status, and social support, highlighting key contextual challenges that impact older adults’ wellbeing in LMICs.
Our analysis illuminates possible gaps in meeting the needs of men and women suffering from poor mental health in this setting. Similar to other evidence from South Africa, we find that women are more likely to report depressive symptoms than men (Peltzer & Phaswana-Mafuya, 2013). Furthermore, we find that the association between depressive symptoms and receipt of social support tends to be negative. This is in line with other studies, largely from high income countries, that suggest that depression leads to isolation and decreased access to social support (Cacioppo et al., 2006; Holt-Lunstad et al., 2010). Women with depressive symptoms face significantly lower odds of receiving emotional or financial support than women without these symptoms, while men with these symptoms face significantly lower odds of receiving physical and financial support.
Given that emotional needs would seem to be the most connected to depression, we expected to find strong associations between having depressive symptoms and receiving emotional support. We found evidence for this among women but not among men in our sample. It may be that, given the strong patriarchal norms of the community, masculinity limits men's ability to ask for or be offered emotional support. Additionally, mental health issues may be overlooked or stigmatized among this population, and especially among men, which can further inhibit this ability. These mechanisms may help to explain the lack of significance in the association between depressive symptoms and receipt of emotional support among men but not women.
Research stemming almost entirely from high income countries consistently suggests that marriage brings health benefits, especially for men (Waite & Gallagher, 2002; Zhu & Gu, 2010) and it is often theorized that this benefit comes from access to social networks and support (Cornwell, 2012; Kalmijn, 2003). Research on this topic in LMICs tends to focus mainly on the impact of widowhood on health (Bennett, 2005; Lin, Brown, Wright, & Hammersmith, 2019) or combines divorce and widowhood into one category of ‘marital dissolution’ (Myroniuk, 2017). We separate categories of divorce and widowhood for a more nuanced understanding of the relationship between marriage, support and mental health. Our results suggest that being never married, separated/divorced, or widowed is associated with lower odds of receiving any type of support, relative to being married/cohabiting, for both men and women. Moreover, these findings prompt us to re-think the expectation that marital dissolution is met with greater social support, and the evidence that widows, in particular, garner more social support compared with those currently married (Connidis, 2001).
Our test of whether marital status modifies associations between depressive symptoms and receipt of social support revealed that divorce matters for women, whereas widowhood matters for men. For both men and women in these respective statuses of marital dissolution, when compared with married counterparts, having depressive symptoms was associated with greater odds of receiving support. These findings suggest that women's informal social networks are more responsive to their needs if they experience a marital dissolution due to marital breakdown, while men's networks may be more responsive to marital dissolutions that result from spousal death.
Women may be especially at risk of economic loss in the case of a divorce (Holden & Smock, 1991), and their friends and family may therefore step in with financial support to mitigate this. Women often have more diverse and robust social networks to draw from during stressful events (Antonucci and Akiyama, 1987, Carr and Bodnar-Deren, 2009), and this may explain why we see a modifying effect of separation/divorce for women but not men. This is an important nuance in understanding the relationship between marriage and social support in this setting, and future studies could shed light on the mechanisms operating.
We found limited evidence that widowhood modifies the association between depressive symptoms and receipt of support, with the exception of men's receipt of physical support. Although unexpected, these results are in line with evidence suggesting that the depression brought on by the distressing event of a spousal death cannot be mitigated by social support (Stroebe, Stroebe, Abakoumkin, & Schut, 1996). Women, in particular, may suffer strained social ties after their husbands' death, as research in this setting has revealed that women are sometimes blamed for their husband's death (Schatz et al., 2011). Men who experience the death of their spouse, on the other hand, appear to garner physical support in response to depressive symptoms. This is suggestive of greater recognition and response, from within their social networks, to widow men's physical needs that result from mental health struggles.
In interpreting our results, it is important to keep in mind a few limitations. First, the relationship between mental health and social support is almost certainly bi-directional: People who have more depressive symptoms face greater need for support from their friends and family, and people who have more social support may have fewer depressive symptoms. Because our data are cross-sectional, we cannot determine the direction of association. We have treated social support as the dependent measure, with the assumption that any significant associations we pick up are more likely to indicate that social support reacts to health than vice versa. Second, healthier people may be selected into stable marriages (Lamb, Lee, & DeMaris, 2003; Mastekaasa, 1992), and their marital status, itself, may exacerbate mental health issues (Mastekaasa, 1992). Third, we do not have complete information on past marital dissolutions, and whether they resulted from divorce or widowhood. We control for a respondent's total number of marriages, but future research could benefit from a closer look at the impact of lifetime marital trajectories. Finally, our cross-sectional data may underestimate the magnitude of the influence of depressive symptomology on receiving support in this population (Schwarzbach, Luppa, Forstmeier, König, & Riedel-Heller, 2014). Future research should utilize subsequent waves of the HAALSI data to help unpack these associations.
Conclusion
Population aging in LMICs, including South Africa, will only heighten the growing mental health burden in these countries. Understanding the protective factors of core social institutions such as social support and marriage is a key component to understanding and addressing this health crisis. In rural South Africa, gaps in informal social support might best be filled by formal systems of support, such as health and social services, that could complement the existing state-sponsored elderly pension program with support that is emotional and/or physical in nature.
Author statement
Elyse A. Jennings: Conceptualization, Methodology, Data curation, Analysis, Writing - original draft, Writing - editing and revisions; Margaret Ralston: Conceptualization, Methodology, Writing - original draft, review, and editing; Enid Schatz: Conceptualization, Contextualizing, Writing - review and editing.
Statement of ethical approval
HAALSI was ethically approved by review committees at the University of the Witwatersrand Human Research Ethics Committee, the Harvard T.H. Chan School of Public Health Office of Human Research Administration (HCS OHRA) and the Mpumalanga Provincial Research and Ethics Committee.
Acknowledgements
The HAALSI study was funded by NIA of the NIH (P01 AG041710). HAALSI is nested within the Agincourt Health and Socio-Demographic Surveillance System, with funding from Wellcome Trust (058893/Z/99/A; 069683/Z/02/Z; 085477/Z/08/Z; 085477/B/08/Z), University of the Witwatersrand, and Medical Research Council, South Africa.
Footnotes
Each gender difference reported in this paragraph is significant at p < .05, except for receipt of emotional support, which is significant at p < .10, and separated/divorced status, which does not reach statistical significance at p < .10.
We also tested, in models not shown, the odds of receiving social support from a presumptive child. These outcome measures were coded similarly to those shown, but indicating that the support received was from a relative between 18 and 38 years younger than the respondent (limited information on the respondent's relationship to named contacts made this approximation the best proxy for children's support). These analyses revealed no significant association between depressive symptoms and receipt of any type of support from presumptive children, nor significant differences by marital status. Hence, we do not find evidence that children, in particular, respond to parental depressive symptoms with increased (or decreased) support in physical, emotional, or financial form.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100666.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Amoateng A.Y., Richter L., Makiwane M., Rama S. 2004. Describing the structure and needs of families in South Africa: Towards the development of a national policy framework for families. [Google Scholar]
- Antonucci T.C., Akiyama H. An examination of sex differences in social support among older men and women. Sex Roles. 1987;17(11):737–749. doi: 10.1007/bf00287685. [DOI] [Google Scholar]
- Beekman A.T.F., Kriegsman D.M.W., Deeg D.J.H., van Tilburg W. The association of physical health and depressive symptoms in the older population: Age and sex differences. Social Psychiatry and Psychiatric Epidemiology. 1995;30(1):32–38. doi: 10.1007/bf00784432. [DOI] [PubMed] [Google Scholar]
- Beekman A.T.F., Penninx B.W.J.H., Deeg D.J.H., Ormel J., Braam A.W., van Tilburg W. Depression and physical health in later life: Results from the longitudinal aging study Amsterdam (LASA) Journal of Affective Disorders. 1997;46(3):219–231. doi: 10.1016/S0165-0327(97)00145-6. [DOI] [PubMed] [Google Scholar]
- Bennett K.M. Widowhood in elderly women: The medium- and long-term effects on mental and physical health. Mortality. 1997;2(2):137–148. doi: 10.1080/713685857. [DOI] [Google Scholar]
- Bennett K.M. Psychological wellbeing in later life: The longitudinal effects of marriage, widowhood and marital status change. International Journal of Geriatric Psychiatry. 2005;20(3):280–284. doi: 10.1002/gps.1280. [DOI] [PubMed] [Google Scholar]
- Bishwajit G., Kota K., Buh A., Yaya S. Self-reported food insecurity and depression among the older population in South Africa. Psychiatry. 2020;2(1):34–43. [Google Scholar]
- Blanchflower D.G., Oswald A.J. Is well-being U-shaped over the life cycle? Social Science & Medicine. 2008;66(8):1733–1749. doi: 10.1016/j.socscimed.2008.01.030. [DOI] [PubMed] [Google Scholar]
- Booysen F., Van der Berg S. The role of social grants in mitigating the socio-economic impact of HIV/AIDS in two free state communities. South African Journal of Economics. 2005;73(s1):545–563. doi: 10.1111/j.1813-6982.2005.00038.x. [DOI] [Google Scholar]
- Budlender D., Lund F. South Africa: A legacy of family disruption. Development and Change. 2011;42(4):925–946. doi: 10.1111/j.1467-7660.2011.01715.x. [DOI] [PubMed] [Google Scholar]
- Cacioppo J.T., Hughes M.E., Waite L.J., Hawkley L.C., Thisted R.A. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychology and Aging. 2006;21(1):140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Carr D., Bodnar-Deren S. Gender, aging and widowhood. In: Uhlenberg P., editor. International handbook of population aging. Springer Netherlands; Dordrecht: 2009. pp. 705–728. [Google Scholar]
- Chang A.Y., Gómez-Olivé F.X., Payne C., Rohr J.K., Manne-Goehler J., Wade A.N.…Salomon J.A. Chronic multimorbidity among older adults in rural South Africa. BMJ Global Health. 2019;4(4) doi: 10.1136/bmjgh-2018-001386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian A.K., Sanuade O.A., Okyere M.A., Adjaye-Gbewonyo K. Social capital is associated with improved subjective well-being of older adults with chronic non-communicable disease in six low- and middle-income countries. Globalization and Health. 2020;16(1):2. doi: 10.1186/s12992-019-0538-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cliggett L. Cornell University Press; Ithaca, NY: 2005. Grains from grass: Aging, gender and famine in rural Africa. [Google Scholar]
- Collinson M.A., Tollman S.M., Kahn K. Migration, settlement change and health in post-apartheid South Africa: Triangulating health and demographic surveillance with national census data 1. Scandinavian Journal of Public Health. 2007;35(69_suppl):77–84. doi: 10.1080/14034950701356401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connidis I. SAGE Publications; Thousand Oaks, CA: 2001. Family ties and aging. [Google Scholar]
- Cornwell B. Spousal network overlap as a basis for spousal support. Journal of Marriage and Family. 2012;74(2):229–238. doi: 10.1111/j.1741-3737.2012.00959.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell E.Y., Waite L.J. Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior. 2009;50(1):31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer D. Emotional support, conflict, depression, and relationship satisfaction in a romantic partner AU - cramer, Duncan. Journal of Psychology. 2004;138(6):532–542. doi: 10.3200/JRLP.138.6.532-542. [DOI] [PubMed] [Google Scholar]
- Eaton J., McCay L., Semrau M., Chatterjee S., Baingana F., Araya R. Scale up of services for mental health in low-income and middle-income countries. The Lancet. 2011;378(9802):1592–1603. doi: 10.1016/S0140-6736(11)60891-X. [DOI] [PubMed] [Google Scholar]
- Filmer D., Pritchett L.H. Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states Of India*. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Frech A., Williams K. Depression and the psychological benefits of entering marriage. Journal of Health and Social Behavior. 2007;48(2):149–163. doi: 10.1177/002214650704800204. [DOI] [PubMed] [Google Scholar]
- Geldsetzer P., Vaikath M., Wagner R., Rohr J.K., Montana L., Gómez-Olivé F.X.…Berkman L.F. Depressive symptoms and their relation to age and chronic diseases among middle-aged and older adults in rural South Africa. Journal of Gerontology: Series A. 2019 doi: 10.1093/gerona/gly145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glymour M.M., Yen J.J., Kosheleva A., Moon J.R., Capistrant B.D., Patton K.K. Elevated depressive symptoms and incident stroke in Hispanic, African-American, and White older Americans. Journal of Behavioral Medicine. 2012;35(2):211–220. doi: 10.1007/s10865-011-9356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Olivé F.X., Montana L., Wagner R.G., Kabudula C.W., Rohr J.K., Kahn K.…Berkman L. Cohort profile: Health and ageing in Africa: A longitudinal study of an INDEPTH community in South Africa (HAALSI) International Journal of Epidemiology. 2018;47(3):689–690j. doi: 10.1093/ije/dyx247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harling G., Perkins J.M., Gómez-Olivé F.X., Morris K., Wagner R.G., Montana L.…Berkman L. Interviewer-driven variability in social network reporting: Results from health and aging in Africa: A longitudinal study of an INDEPTH community (HAALSI) in South Africa. Field Methods. 2018;30(2):140–154. doi: 10.1177/1525822X18769498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden K.C., Smock P.J. The economic costs of marital dissolution: Why do women bear a disproportionate cost? Annual Review of Sociology. 1991;17(1):51–78. doi: 10.1146/annurev.so.17.080191.000411. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: A meta-analytic review. PLoS Medicine. 2010;7(7) doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosegood V., McGrath N., Moultrie T. Dispensing with marriage: Marital and partnership trends in rural KwaZulu-Natal, South Africa 2000-2006. Demographic Research. 2009;20:279–312. doi: 10.4054/DemRes.2009.20.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack H., Wagner R.G., Petersen I., Thom R., Newton C.R., Stein A. Closing the mental health treatment gap in South Africa: A review of costs and cost-effectiveness. Global Health Action. 2014;7:1–11. doi: 10.3402/gha.v7.23431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaga A., Arabandi B., Bagraim J., Mdlongwa S. Doing the ‘gender dance’: Black women professionals negotiating gender, race, work and family in post-apartheid South Africa. Community, Work & Family. 2018;21(4):429–444. doi: 10.1080/13668803.2017.1311840. [DOI] [Google Scholar]
- Jennings E.A., Mkhwanazi N., Berkman L. Ageing and Society; 2018. Receipt of emotional support among rural South African adults. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmijn M. Shared friendship networks and the life course: An analysis of survey data on married and cohabiting couples. Social Networks. 2003;25(3):231–249. doi: 10.1016/S0378-8733(03)00010-8. [DOI] [Google Scholar]
- Kawachi I., Berkman L.F. Social ties and mental health. Journal of Urban Health. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohler I.V., Payne C.F., Bandawe C., Kohler H.-P. The demography of mental health among mature adults in a low-income, high-HIV-prevalence context. Demography. 2017;54(4):1529–1558. doi: 10.1007/s13524-017-0596-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb K.A., Lee G.R., DeMaris A. Union formation and depression: Selection and relationship effects. Journal of Marriage and Family. 2003;65(4):953–962. doi: 10.1111/j.1741-3737.2003.00953.x. [DOI] [Google Scholar]
- Lin I.F., Brown S.L., Wright M.R., Hammersmith A.M. Depressive symptoms following later-life marital dissolution and subsequent repartnering. Journal of Health and Social Behavior. 2019;60(2):153–168. doi: 10.1177/0022146519839683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastekaasa A. Marriage and psychological well-being: Some evidence on selection into marriage. Journal of Marriage and Family. 1992;54(4):901–911. [Google Scholar]
- Mendes De Leon C.F., Rapp S.S., Kasl S.V. Financial strain and symptoms of depression in a community sample of elderly men and women:A longitudinal study. Journal of Aging and Health. 1994;6(4):448–468. doi: 10.1177/089826439400600402. [DOI] [Google Scholar]
- Mirowsky J. Age and the gender gap in depression. Journal of Health and Social Behavior. 1996;37(4):362–380. doi: 10.2307/2137263. [DOI] [PubMed] [Google Scholar]
- Myroniuk T.W. Marital dissolutions and the health of older individuals in a rural African context. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2017;72(4):656–664. doi: 10.1093/geronb/gbw077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltzer K., Phaswana-Mafuya N. Depression and associated factors in older adults in South Africa. Global Health Action. 2013;6 doi: 10.3402/gha.v6i0.18871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ralston M., Schatz E., Menken J., Gomez-Olive F.X., Tollman S. Who benefits-or does not--from South Africa's old age pension? Evidence from characteristics of rural pensioners and non-pensioners. International Journal of Environmental Research and Public Health. 2015;13(1):85. doi: 10.3390/ijerph13010085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross C.E. Reconceptualizing marital status as a continuum of social attachment. Journal of Marriage and Family. 1995;57(1):129–140. doi: 10.2307/353822. [DOI] [Google Scholar]
- Ross C.E., Mirowsky J. Family relationships, social support and subjective life expectancy. Journal of Health and Social Behavior. 2002;43(4):469–489. doi: 10.2307/3090238. [DOI] [PubMed] [Google Scholar]
- Ross R., Zeller R., Srisaeng P., Yimmee S., Somchid S., Sawatphanit W. Depression, stress, emotional support, and self-esteem among baccalaureate nursing students in Thailand. International Journal of Nursing Education Scholarship. 2005;2 doi: 10.2202/1548-923x.1165. [DOI] [PubMed] [Google Scholar]
- Rudwick S., Casale D. Is marriage a dying institution in South Africa? Exploring changes in marriage in the context of ilobolo payments AU - posel, Dorrit. Agenda. 2011;25(1):102–111. doi: 10.1080/10130950.2011.575589. [DOI] [Google Scholar]
- Samson M.M., Meeuwsen I.B., Crowe A., Dessens J.A., Duursma S.A., Verhaar H.J. Relationships between physical performance measures, age, height and body weight in healthy adults. Age and Ageing. 2000;29(3):235–242. doi: 10.1093/ageing/29.3.235. [DOI] [PubMed] [Google Scholar]
- Schatz E., Madhavan S., Collinson M., Gomez-Olive F.X., Ralston M. Dependent or productive? A new approach to understanding the social positioning of older South Africans through living Arrangements. Research on Aging. 2015;37(6):581–605. doi: 10.1177/0164027514545976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz E., Madhavan S., Williams J. Female-headed households contending with HIV/AIDS-related hardship in rural South Africa. Health & Place. 2011;17:598–605. doi: 10.1016/j.healthplace.2010.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz E., Seeley J. Gender, ageing and carework in East and Southern Africa: A review. Global Public Health. 2015;10(10):1185–1200. doi: 10.1080/17441692.2015.1035664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittker . 2008. Happiness and success: Genes, families, and the psychological effects of socioeconomic position and social support. [DOI] [PubMed] [Google Scholar]
- Schone B.S., Weinick R.M. Health-related behaviors and the benefits of marriage for elderly persons. The Gerontologist. 1998;38(5):618–627. doi: 10.1093/geront/38.5.618. [DOI] [PubMed] [Google Scholar]
- Schwarzbach M., Luppa M., Forstmeier S., König H.-H., Riedel‐Heller S.G. Social relations and depression in late life—a systematic review. International Journal of Geriatric Psychiatry. 2014;29(1):1–21. doi: 10.1002/gps.3971. [DOI] [PubMed] [Google Scholar]
- Sennott C., Reniers G., xf mez O., xe Xavier F., Menken J. Premarital births and union formation in rural South Africa. International Perspectives on Sexual and Reproductive Health. 2016;42(4):187–196. doi: 10.1363/42e2716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein M., Bengtson V.L. Does intergenerational social support influence the psychological well-being of older parents? The contingencies of declining health and widowhood. Social Science & Medicine. 1994;38(7):943–957. doi: 10.1016/0277-9536(94)90427-8. [DOI] [PubMed] [Google Scholar]
- Steptoe A., Deaton A., Stone A.A. Subjective wellbeing, health, and ageing. The Lancet. 2015;385(9968):640–648. doi: 10.1016/S0140-6736(13)61489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe W., Stroebe M., Abakoumkin G., Schut H. The role of loneliness and social support in adjustment to loss: A test of attachment versus stress theory. Journal of Personality and Social Psychology. 1996;70(6):1241–1249. doi: 10.1037/0022-3514.70.6.1241. [DOI] [PubMed] [Google Scholar]
- Tomlinson M., Grimsrud A.T., Stein D.J., Williams D.R., Myer L. The epidemiology of major depression in South Africa: Results from the South African Stress and Health study. South African Medical Journal. 2009;99(5):368–373. [PMC free article] [PubMed] [Google Scholar]
- United Nations . Vol. I. Comprehensice Tables; Retrieved from New York: 2015. (World population prospects: The 2015 revision). ST/ESA/SER.A/313. [Google Scholar]
- Waite L., Gallagher M. Crown/Archetype; 2002. The case for marriage: Why married people are happier, healthier and better off financially. [Google Scholar]
- White R.G., Sashidharan S.P. Towards a more nuanced global mental health. British Journal of Psychiatry. 2018;204(6):415–417. doi: 10.1192/bjp.bp.113.139204. [DOI] [PubMed] [Google Scholar]
- Zhu H., Gu D. The protective effect of marriage on health and survival: Does it persist at oldest-old ages? Journal of Population Ageing. 2010;3(3):161–182. doi: 10.1007/s12062-011-9034-8. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.