ABSTRACT
A large measles epidemic has been ongoing in Romania and many European countries, since 2016. We report case-based surveillance data for all patients (n = 1371) with laboratory-confirmed and epidemiologically-confirmed measles hospitalized in a major infectious diseases hospital in Bucharest Romania during the first three years of the current measles epidemic (July 2016–July 2019).
More than half of the patients (57.6%) had ages below 5 years; 6% (n = 82) had preexisting comorbidities. Only 1.5% of the patients had been fully vaccinated, 5.9% had received only one vaccine dose, while 92.8% had not been vaccinated at all against measles. The rate of measles-related complications was 93.4%; complications occurred more frequently among patients who were not eligible for vaccination due to young age or underlying diseases, and among children, who developed pneumonia and enterocolitis more frequently than adults. The median hospital length-of-stay was 6 days. Eight cases (0.6%) required intensive care and mechanical ventilation, and three deaths (0.2%) were recorded.
Measles disproportionately affects patient groups who are not eligible for vaccination. During the current epidemic in Romania, 98.5% of the patients hospitalized for measles had not been vaccinated and among these, 75.7% would have been eligible for vaccination. For the remaining pool of unvaccinated children, supplementary immunization activities are urgently needed.
KEYWORDS: Measles, vaccination, vaccine-preventable disease, measles epidemic
Introduction
Measles is an infectious disease, but it is also an important public health issue. Airborne transmission allows it to easily spread through susceptible populations, and the only effective measure for preventing the disease is vaccination. Given its high reproductive number, high vaccine coverage rates are needed to prevent ongoing transmission, specifically, rates above 95%, ideally within the range of 96–99% [1].
Measles can also be a good candidate for elimination or eradication, since it fulfills all the essential biological principles for global eradication: it causes acute infection, the virus does not persist for a long time in the environment, humans are its only reservoir, and effective and safe vaccines exist and can interrupt transmission [2]. The World Health Organization (WHO)’s Global Measles and Rubella Strategic Plan set the year 2015 as the target for measles elimination in the European Region [3]. However, here we are, almost five years later, and Europe is facing the largest measles epidemic reported during the past years, with multiple countries reporting high numbers of cases, both in countries where measles was still endemic, and in countries where measles had been eliminated.
While coverage of measles-containing vaccine (MCV) in Romania was consistently above 95% for both recommended doses until 2009, a sharp decrease in coverage was associated first with the 2011–2013 measles epidemic, and then a further decrease to 85.8% for MCV1 and 67% for MCV2 in 2015 prompted the current epidemic, which started in 2016 and is still ongoing [4–7].
Measles-related complications represent some of the main reasons for hospitalization, but not enough data is available on the extent of these complications, or on their impact on the severity of the infection.
We aimed to characterize the cases of measles hospitalized in a major infectious diseases hospital in Bucharest during the current measles epidemic, in order to ensure optimal future preparedness and outbreak response in a country still endemic for measles, and also to inform public health policies on how to better address the gaps in reaching WHO’s measles elimination goals in Romania.
Patients and methods
The current study analyzes case-based surveillance data for all patients with measles admitted to the National Institute for Infectious Diseases “Prof. Dr. Matei Balș”, during the first three years of the current measles epidemic (July 2016 – July 2019). The institute is the national reference center for the diagnosis and management of infectious diseases. It is located in Bucharest Romania and covers the Bucharest-Ilfov area, along with the surrounding counties from South-Eastern Romania, but it is also the main referral center for complicated cases from hospitals throughout the country.
For each measles case, data was prospectively entered into the epidemiological notification report forms and the patients’ files as part of the hospital’s measles surveillance. The notification forms were based on the national surveillance methodology, and included all the EU and WHO recommended minimum data elements for case-based data [8]. The following variables were processed for the purpose of this study: demographic data, clinical picture at onset, time span from onset to hospital admission, duration of hospital stay, course and outcome of disease, occurrence and type of complications, presence of comorbidities, vaccination history, existence of contraindication to vaccination, use of healthcare resources, and case classification according to the case definition [5,8,9]. Among complications, we looked specifically at all-cause and bacterial pneumonia, thrombocytopenia, enterocolitis (diarrhea), cytolysis, acute encephalitis, otitis media, bacterial sepsis and acute respiratory failure (defined as SpO2 < 90% on room air).
The following laboratory criterion was used for confirming cases according to the ECDC definition: “measles virus specific antibody response characteristic for acute infection in serum” [9], by using the following kits in the hospital’s laboratory to test blood samples from possible measles cases: Masern Virus/Measles/Rougeole IgM and Masern Virus/Measles/Rougeole IgG, Institute Virion\Serion, Würzburg, Germany. In case of equivocal results, and for patients with severe disease or death, retesting was performed in the reference laboratory at the National Institute for Medico-Military Research Cantacuzino.
Use of the data for publication was approved by the Institutional Review Board and by the Bioethics Committee of the National Institute for Infectious Diseases “Prof. Dr. Matei Balș”, Bucharest, Romania. A waiver for informed consent was granted by the Bioethics Committee for the purpose of this observational study.
The statistical analysis was performed using IBM SPSS Statistics for Windows, version 20 (IBM Corp., Armonk, NY, USA). For continuous variables with non-parametric distribution we report the median and interquartile range (IQR), and for categorical variables we report the frequency and percentage, along with the results of the Chi square test and odds ratios (OR) and 95% confidence intervals (95%CI) for risk calculation. Multiple regression analysis was used to assess the impact of measles-related complications on the duration of hospital admission, and the role of specific risk factors in the occurrence of severe outcome of measles infection, defined as a composite of: prolonged hospital stay (upper quartile), need for mechanical ventilation, or death. Two-tailed p values <0.05 were considered statistically significant.
Results
Patient population
During the study timespan, a total number of 1468 patients were admitted to our hospital with measles, of which 1289 (87.8%) were laboratory confirmed (confirmed cases), 82 (5.6%) were epidemiologically confirmed (probable cases) and 97 (6.6%) were clinical cases (possible cases). In the current article, we present data for the laboratory-confirmed and epidemiologically-confirmed cases (n = 1371).
Overall, 51.6% (n = 708) of patients were male and 56.7% (n = 777) had acquired the infection in an urban area. Approximately half (51.1%, n = 700) of the patients came from Bucharest/Ilfov, and the other half came mostly from 23 counties in South-Eastern Romania – Figure 1.
Figure 1.
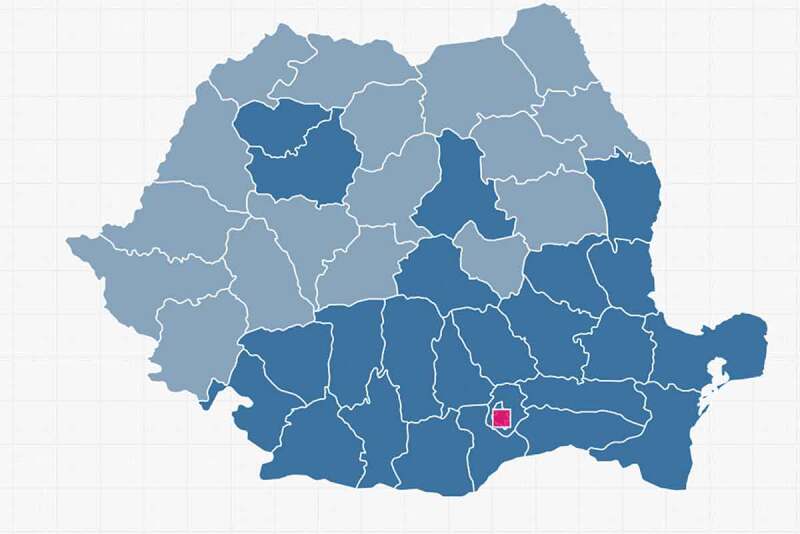
Geographic distribution of measles cases hospitalized in the National Institute for Infectious Diseases “Prof. Dr. Matei Balș” during the first three years of the current (2016 – ongoing) epidemic. Counties of origin of patients are marked in dark blue.
The median age was 3 years old (IQR: 1–10 years, range: 0–63 years). More than half of the patients (57.6%) had ages below 5 years old (Table 1). Females had significantly higher ages at onset (median 4 years, IQR: 1–14 yeas) compared to males (median 3 years, IQR: 0–8 years), p < 0.001, U = 205,767, r = −0.1.
Table 1.
Distribution of confirmed and probable measles cases by age group and immunization status in the first three years of the current (2016 – ongoing) epidemic.
| Core age group | Number of cases | Percentage of cases | Cumulative percentage of cases | Two doses of MCV | One dose of MCV | Zero doses of MCV | Unknown vaccination status |
|---|---|---|---|---|---|---|---|
| 0–8 months | 238 | 17.4 | 17.4 | 0 | 0 | 238 | 0 |
| 9–11 months | 100 | 7.3 | 24.7 | 0 | 2 | 95 | 3 |
| 1–4 years | 452 | 33.0 | 57.6 | 1 | 34 | 392 | 25 |
| 5–9 years | 211 | 15.4 | 73.0 | 3 | 18 | 164 | 26 |
| 10–14 years | 107 | 7.8 | 80.8 | 5 | 9 | 72 | 21 |
| 15–19 years | 50 | 3.6 | 84.5 | 1 | 1 | 30 | 18 |
| 20–24 years | 27 | 2.0 | 86.4 | 1 | 0 | 19 | 7 |
| 25–29 years | 53 | 3.9 | 90.3 | 5 | 3 | 26 | 19 |
| 30–34 years | 48 | 3.5 | 93.8 | 0 | 1 | 28 | 19 |
| 35–39 years | 48 | 3.5 | 97.3 | 0 | 2 | 26 | 20 |
| >40 years | 37 | 2.7 | 100.0 | 2 | 1 | 19 | 15 |
| Total | 1371 | N/A | N/A | 18 | 71 | 1109 | 173 |
MCV – measles-containing vaccine.
Only 6% (n = 82) of the cases had preexisting comorbid diseases; among these cases, most (n = 34) had one underlying condition, 20 patients had two underlying conditions, and the rest (n = 24, missing data for 4 patients) had ≥3 comorbidities, with a maximum number of 11 comorbidities in one case. The preexisting comorbid diseases were classified as neurological disease in 20 cases (24.4% of those with comorbidities and 1.5% of the whole patient group), immune deficit in 25 cases (30.5%/1.8%), chronic liver disease in 12 cases (14.6%/0.9%), congenital malformations in 16 cases (19.5%/1.2%), and other comorbidities in 33 cases (40.2%/2.4%).
Monthly hospitalized case distribution
Hospital admissions for cases from the current measles epidemic started in late 2016, with the number of hospitalized cases slowly building up in 2017, with a first peak in the winter of 2017 (November-December 2017), a second, higher, peak in March-April 2018, and continued transmission throughout the summer of 2018 (with cases reported up to August 2018). Transmission continued in 2019 (late winter, spring and summer – data current through July 2019), albeit at a lower rate – Figure 2.
Figure 2.
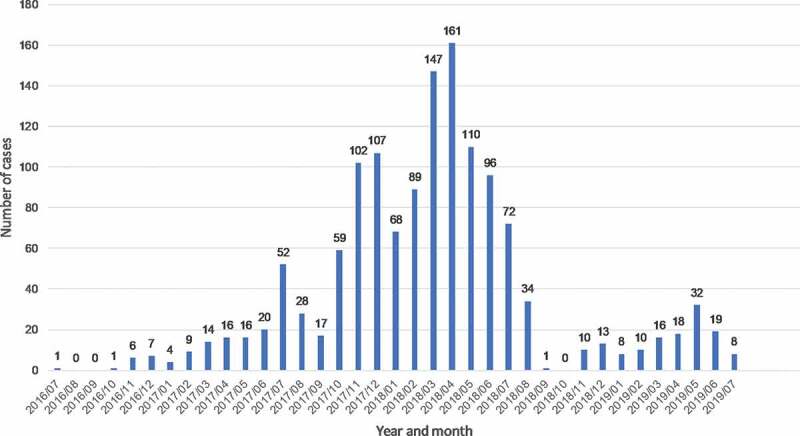
Monthly distribution of hospitalized measles cases during the first three years of the current (2016 – ongoing) epidemic in the National Institute for Infectious Diseases “Prof. Dr. Matei Balș”.
Immunization status
Information on vaccine status was available for 87.2% of patients (n = 1195): among these, 18 patients (1.5%) had been vaccinated with two doses of MCV, 71 (5.9%) had received only one previous dose of MCV, and the vast majority of patients (n = 1109, 92.8%) had not been vaccinated with MCV at all. Among the latter group (patients with zero previous doses of MCV), 840 (75.7%) would have been eligible for vaccination, 3 cases (0.3%) had an underlying condition that associated immune impairment, and 266 cases (24.0%) had ages below the threshold for vaccination, which was defined for the purpose of this analysis as 12 months old up until December 2016 (which was at that time the standard age for receiving the first dose of MCV in Romania through the general practitioner network), and 9 months old after December 2016, when a supplementary MCV dose was introduced in the national immunization regimen, in order to contain the ongoing measles epidemic. The numbers of cases by age group and immunization status are presented in Table 1.
Clinical picture and healthcare resource use
Clinically, all patients had a rash and fever, 96.9% (n = 1328) had either one of the upper respiratory tract symptoms (93.3%, n = 1279 cough, 84.8%, n = 1162 coryza), and 73.7% (n = 1011) had conjunctivitis. All cases met the clinical case definition of fever plus rash plus cough, coryza or conjunctivitis, while 73.1% of the cases (n = 1002) had the complete clinical picture, with fever plus rash plus cough or coryza plus conjunctivitis.
Most cases were admitted to the hospital on the day when the rash appeared (28.3%, n = 388), or on the next day following rash onset (27.8%, n = 381). A total of 15.7% of patients (n = 213) were admitted to the hospital during the prodromal phase of the disease (1–4 days prior to rash onset), while 26.3% of patients (n = 358) were admitted to the hospital ≥2 days after rash onset, for measles complications. In 0.4% of cases (n = 4) rash occurred in patients who had already been hospitalized for a different reason, for ≥10 days (nosocomial measles cases); none of these four patients had been vaccinated. Among these nosocomial cases, pneumonia was a frequent complication (in three of the cases), but no deaths were recorded. For 0.7% of cases (n = 10) there was missing information regarding the time from rash onset to hospital admission.
Four percent of patients (n = 55) had been transferred to our institute from a different hospital, for the management of measles-related complications. The median duration of hospitalization was 6 days (IQR: 5–8 days).
Measles-related complications
The overall rate of measles-related complications was extremely high, with 93.4% (n = 1280) of patients presenting at least one complication, as follows: 81.3% (n = 1114) all-cause pneumonia, 44.4% (n = 609) enterocolitis, 25.3% (n = 347) thrombocytopenia, 19.0% (n = 260) cytolysis, 15.5% (n = 213) acute respiratory failure, 12.2% (n = 167) bacterial pneumonia, 4.4% (n = 61) otitis media, 0.6% (n = 8) bacterial sepsis, and 0.4% (n = 5) acute encephalitis. The number of complications per patient ranged from 0 to 5, with most patients presenting, in decreasing order of frequency, 2 (n = 583, 42.5%), 1 (n = 378, 27.6%) and 3 (n = 260, 19.0%) complications. Eight cases (0.6%) required transfer to a different hospital for intensive care and mechanical ventilation, and three deaths (0.2%) were recorded, all in children: one 11-month old and two one-year-olds. Among the cases who died, two had no preexisting comorbid disease, and one case had a cumulus of comorbidities: hypochromic microcytic anemia, grade 1/2 protein calorie malnutrition, hyperthyroidism, and concomitant enteroviral infection. All three cases had severe measles complicated with bronchopneumonia and acute respiratory distress requiring mechanical ventilation, and one of the cases also presented sepsis with multisystem organ failure.
Nine of the adult patients were pregnant at the time when they developed measles. Of these, 7 developed at least one complication (pneumonia n = 5, thrombocytopenia n = 3, acute respiratory failure n = 2, cytolysis n = 1); the odds of developing these complications were not significantly different from those of non-pregnant female adults (all p > 0.05). Two of these cases had adverse pregnancy outcomes or events (spontaneous abortion at 16 weeks of gestation and vaginal bleeding at 22 weeks of gestation, respectively). For the other cases, no pregnancy-related complication was recorded during their measles episode, but pregnancy outcome data was not available following discharge from our institution.
The occurrence of any type of complication significantly prolonged the duration of hospitalization from a median (IQR) of 5.5 (3–7) days in the absence of complications to 7 (5–8) days (p < 0.001, U = 49,846, r = −0.1). Multiple regression identified the following significant predictors of prolonged hospitalization: any complication (B = 1.2, 95%CI: 4.8–6.1, p = 0.008), enterocolitis (B = 0.5, 95%CI: 0.2–0.9, p = 0.006), and acute respiratory failure (B = 1.6, 95%CI: 1.1–2.1, p < 0.001), while pneumonia (B = 0.1, 95%CI: −0.5–0.7, p = 0.783), thrombocytopenia (B = −0.3, 95%CI: −0.7–0.1, p = 0.174), cytolysis (B = −0.4, 95%CI: −0.9–0.04, p = 0.070) and acute encephalitis (B = 2.8, 95%CI: −0.3–5.8, p = 0.079) were not associated with a significant impact (F(7, 1449) = 12.091, p < 0.001, R2 = 0.06).
Overall, 457 patients (33.3%) presented the composite severity outcome, with multiple regression identifying the following significant predictors of severity (F(14, 1340) = 10.273, p < 0.001): time from onset of rash to hospital admission (B = −0.037, 95 CI: −0.048–0.027, p < 0.001), preexisting immune impairment (B = 0.231, 95%CI: 0.048–0.413, p = 0.013), and the occurrence of complications such as otitis media (B = 0.162, 95%CI: 0.043–0.281, p = 0.008) and bacterial pneumonia (B = 0.272, 95%CI: 0.195–0.350, p < 0.001), while other factors such as age, gender, preexisting neurological disease, and specific complications such as all-cause pneumonia, thrombocytopenia, enterocolitis, cytolysis, acute encephalitis, and bacterial sepsis did not significantly influence the model (all p > 0.05).
The overall rate of complications was comparable between patients with and without chronic conditions (90.2% vs. 93.6%, p = 0.245), but certain complications were more frequent in patients with underlying conditions, as follows: thrombocytopenia (36.6% vs. 24.6%, OR = 1.8, 95%CI: 1.1–2.8, p = 0.018), cytolysis (33.3% vs. 18.1%, OR = 2.3, 95%CI: 1.4–3.7, p = 0.002), and acute respiratory failure (25.6% vs. 15.0%, OR = 2.0, 95%CI: 1.2–3.2, p = 0.017).
Prematurity was associated with a higher risk of bacterial pneumonia (OR = 22.0, 95%CI:2.3–212.5, p < 0.001) and acute respiratory failure (OR = 16.4, 95%CI:1.7–158.7, p = 0.013), Patients with preexisting neurological disease had higher odds of developing certain measles-related complications, specifically bacterial pneumonia (45% vs. 11.7%, OR = 6.2, 95%CI: 2.5–15.1, p < 0.001), bacterial sepsis (10% vs. 0.4%, OR = 24.9, 95%CI:4.7–131.8, p = 0.005), cytolysis (42.1% vs. 18.7%, OR = 3.2, 95%CI: 1.3–8.0, p = 0.017), and acute respiratory failure (50% vs. 15.1%, OR = 5.6, 95%CI:2.3–13.7, p < 0.001). Patients with preexisting immune deficit had higher odds of developing thrombocytopenia (50% vs. 24.9%, OR = 3.0, 95%CI: 1.4–6.6, p = 0.006), and so did patients with preexisting liver disease (69.2% vs. 24.9%, OR = 6.8, 95%CI:2.1–22.2, p = 0.001). Patients who had congenital malformations had higher odds of developing bacterial pneumonia (41.2% vs. 11.8%, OR = 5.2, 95%CI: 2.0–13.9, p = 0.002) and acute respiratory failure (41.2% vs. 15.3%, OR = 3.9, 95%CI:1.5–10.3, p = 010).
Complications were also more frequent among patients who were not eligible for vaccination either due to age or due to medical contraindication (96.2% vs. 92.8%, OR = 2.0, 95%CI: 1.1–3.9, p = 0.039). Specifically, three of the recorded complications were more frequent in this category of patients: pneumonia (88.7% vs. 79.5%, OR = 2.0, 95%CI: 1.4–3.0, p < 0.001), enterocolitis (60.5% vs. 40.7%, OR = 2.2, 95%CI: 1.7–2.9, p < 0.001), and acute respiratory failure (29.7% vs. 12.2%, OR = 3.0, 95%CI: 2.2–4.2, p < 0.001).
When comparing the rate of complications in children (<18 years) versus adults (18 years and older), children displayed a higher rate of developing any measles-related complication (96.1% vs. 80.2%, OR = 1.2, 95%CI: 1.1–1.3, p < 0.001). The following complications were more frequent in children: pneumonia (88.0% vs. 48.3%, OR = 1.8, 95%CI: 1.6–2.1, p < 0.001), enterocolitis (51.6% vs. 9.6%, OR = 5.4, 95%CI: 3.6–8.1, p < 0.001) and the following were more frequent in adults: thrombocytopenia (48.7% vs. 20.6%, OR = 3.7, 95%CI: 2.7.2–4.9, p < 0.001), cytolysis (36.8% vs. 15.4%, OR = 3.2, 95%CI: 2.3–4.4, p < 0.001), whereas for acute encephalitis data were insufficient to allow a comparison, and for acute respiratory failure the rate was similar in the two groups (13.0% in adults vs. 16.1%, p = 0.274).
When looking specifically at children with ages below 1 year, we found that they had a higher risk of developing any measles-related complication (96.1% vs. 92.6%, OR = 2.0, 95%CI:1.1–3.6, p = 0.029), and specifically all-cause pneumonia (88.3% vs. 79.1%, OR = 2.0, 95%CI:1.4–2.9, p < 0.001), bacterial pneumonia (18.6% vs. 10.2%, OR = 2.0, 95%CI:1.4–2.9, p < 0.001), enterocolitis (58.1% vs. 40.1%, OR = 2.1, 95%CI:1.6–2.7, p < 0.001), and acute respiratory failure (27.5% vs. 11.7%, OR = 2.9, 95%CI:2.1–3.9, p < 0.001).
Discussion
We have reported the characteristics of measles cases admitted to a major infectious diseases hospital in Romania in the three-year time span from the beginning of the current epidemic. More than half of the patients had ages below 5 years old, but all age groups were affected to a certain extent, including adults. Since the beginning of the current epidemic, measles has lost its seasonality, circulating all year round, with high numbers of cases even during summertime in 2017.
Almost all cases (98.5% of those for whom immunization status was available) had not been vaccinated at all or had only received one dose of MCV. Among patients who had not received any dose of MCV, 75.9% would have been eligible for vaccination, suggesting that they had either opted-out of vaccination or missed the various opportunities for receiving the state-mandated vaccine.
Refusal of MCV has a threefold impact. First, measles can associate important complications, over 90% of the patients hospitalized in our institute having complicated disease, and among these, over 15% being life-threatening complications – such as acute respiratory failure. Furthermore, while the rate of complications was unsurprisingly extremely high (90.2%) in patients with underlying chronic conditions, complications also occurred in 93.6% of otherwise healthy patients, and there is no way to predict who among this latter category will go on to develop complications.
Second, contrary to popular belief that “childhood illnesses are milder during childhood”, this may not be particularly true for measles, where our study has shown that children were actually at a 1.2-fold higher risk of developing any measles-related complication compared to adults, and they specifically had 1.8-fold higher odds of developing pneumonia and 5.4-fold higher odds of developing enterocolitis.
Third, our study has shown that vaccination is more than just a personal choice. When it comes to highly contagious diseases such as measles, one’s decision to refuse or defer vaccination also has an important public health impact, leaving those at the highest risk of severe disease (i.e., those not eligible for vaccination) exposed to a potentially serious infection. In our study severe disease was more frequent among patients not otherwise eligible for vaccination; they presented 2-fold higher odds of developing any complication, pneumonia, or enterocolitis, and 3-fold higher odds of acute respiratory failure.
On a national level, 17,846 cases have been reported from the beginning of the current epidemic until the end of July 2019 [10]. Among these, 64 deaths were recorded, all occurring in patients who had not been vaccinated (n = 63) or had only received one dose (n = 1), and 24 of which occurring in patients who had no underlying chronic disease [5,10,11]. The main circulating genotype during the 2016–ongoing epidemic was B3, different from the endemic genotype D4 involved in the previous measles outbreaks in Romania [5].
The number of measles cases reported on a national level peaked from January to August 2017 [12]. However, the first consistent peak in hospitalized cases in our study occurred in November-December 2017, and it was followed by a second, higher, peak in March-April 2018, our data being consistent with the reported intense circulation of genotype B3 in Romania during that time span of the epidemic [5].
A good vaccine coverage for MCV is essential in preventing a return to the pre-vaccine era, when measles was still responsible for high numbers of cases and high mortality. The target for obtaining elimination is coverage >95%. When coverage drops below this threshold, the risk of measles outbreaks and/or epidemics exponentially increases, with a recent study from Italy showing that a drop in vaccine coverage below 90% associated a two-fold increase in the number of hospitalized measles cases [13].
In Romania, coverage of MCV in 2015 (the year preceding the current epidemic), and in 2016 and 2017 (throughout the current epidemic) was 85.8%, 87.1% and 87% for MCV1 and 67%, 74.5%, 74.7% for MCV2, respectively [4,14,15]. Shortly after the beginning of the current epidemic, supplementary immunization activities (SIA) were initiated in order to decrease the fraction of susceptible population, as an improved vaccine uptake was evidently the only effective measure that could be taken to contain the epidemic [16,17]. Furthermore, in December 2016, health authorities in Romania also introduced a supplementary dose of MCV in infants, at the age of 9 months. SIAs initially included children with ages below 15 years old, living in areas of ongoing measles outbreaks, in early 2016, and were then extended to include children throughout the country, either unvaccinated children with ages 9 months to 9 years old or partially vaccinated children with ages 5 to 9 years old. However, despite a good initial uptake of SIA, by October 2017 only 31.2% of those eligible for SIA had been vaccinated, with the main reasons for deferral of vaccination through SIA being: not presenting to the general practitioner for SIA (26.4%), children not found at home for SIA (17%), vaccine refusal (14%) and contraindication to vaccination (11.5%), as reported by the Romanian National Center for Communicable Diseases Surveillance and Control [18]. Data current through February 2019 showed that vaccine coverage was 81.7% for MCV1 at 18 months old [19] and still extremely low, at 60%, for MCV2 at 5 years old [20]. Vaccine refusal was significantly more frequent in urban areas compared to rural areas [20], and specifically refusal of MCV was more frequent compared to other vaccines [19], suggesting that this might be connected to the spread of anecdotal “junk science” in the media, which is an ongoing issue that still needs to be addressed by proactive involvement of health experts in the media. Furthermore, continued surveillance of measles is essential for informing public health decisions [21], for redirecting health efforts and deploying intensive SIA into areas with measles outbreaks or with low vaccine coverage.
In our study, we have analyzed the rate of measles-related complications. When comparing our data with a study that looked at a limited number of participants in the USA (n = 33), we found lower rates of bacterial pneumonia (12.2% in our study compared to 30% reported by Hester et al.) and otitis media (4.4% compared to 42%), but a longer duration of hospital stay (a median of 6 days compared to a median of 3.7 days reported by Hester et al.) [22]. When comparing our data with the concurrent 2017 measles outbreak in Belgium (n = 125), the patients from our study had lower rates of cytolysis (19.0% compared to 46%), bacterial pneumonia (12.2% vs. 16%) and acute encephalitis (0.4% vs. 3%), a similar rate of otitis media (4.4% vs. 4%), and a higher rate of enterocolitis (44.4% vs. 30%), while the duration of hospital stay was comparable (6 days vs. 5 days) [23].
As expected for any observational study, the present study has certain limitations. The collected data was based on the epidemiological notification report forms, filled out by the hospital’s physicians, and cross-checked with patients’ files to ensure completeness. Acertain degree of bias or inter-observer differences cannot be ruled out. Furthermore, vaccination status could not be ascertained for all patients based on the available medical records and therefore 176 cases (12.8%) had to be discarded from the immunization status analysis. And finally, since we have analyzed the cases of measles that have been hospitalized in our institute, the results specifically reflect the study population – hospitalized measles cases – and may not be generalizable to the entire population.
The study also has a set of strengths, specifically that it is the first report from Romania of hospitalized measles cases during the current epidemic, the most extensive measles epidemic in Romania during the past decade. Having used ECDC’s and WHO’s case definition, recommended data analysis and report plans for the measles mortality reduction phase [8,21], our data could be used for comparison with that from other countries involved in the current epidemic. In addition, our study has also looked at measles-related complications in depth, and has highlighted certain patient categories that might have higher odds of developing complications.
In conclusion, measles is more than an infectious disease, it is a matter of public health, which disproportionately affects those who are not eligible for vaccination. During the current epidemic, 98.5% of the patients hospitalized for measles had not been vaccinated and among these, 75.7% would have been eligible for vaccination. For the remaining pool of unvaccinated children, supplementary immunization activities are urgently needed and should be coupled with medical information campaigns to properly address all potential hypothetical concerns of parents, in order to increase vaccine uptake among eligible children, contain the current epidemic and prevent future outbreaks.
Acknowledgments
The authors would like to thank all the hospital’s staff, doctors and nurses for their involvement in the management of measles cases during this epidemic, all those who have contributed to the epidemiological notification report forms, and all the residents who were involved in database entry and management: Alina Mihaela Căzănaru (Clinical Emergency Hospital „Sf.Ioan”, Bucharest, Romania), Andreea Cristina Badea (City Hospital Stei, Bihor, Romania), Elena Teodora Stoian (Pneumophthysiology Hospital Leordeni, Argeș, Romania), Andreea Silvia Ioaneș (City Hospital „Sf.Spiridon” Mioveni, Argeș, Romania), Bianca Georgiana Milcu (Carol Davila University of Medicine and Pharmacy Bucharest, National Center for Surveillance and Control of Communicable Diseases, Bucharest, Romania), Alina-Andreea Tănase (University Emergency Hospital, Bucharest, Romania), Alexandru Stanca (City Hospital, Zimnicea, Teleorman), Nicolae Rizea (University Emergency Hospital, Bucharest, Romania), Bianca Chipaila (Brăila Emergency Hospital, Brăila, Romania).
Funding Statement
No funding was received for this study.
Author contributions
All authors had equal contributions.
Disclosure statement
The authors declare that they have no conflict of interest.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author [OS] upon reasonable request.
References
- [1].Plans-Rubio P. Evaluation of the establishment of herd immunity in the population by means of serological surveys and vaccination coverage. Hum Vaccin Immunother. 2012;8(2):184–8, 18444 [pii]. [DOI] [PubMed] [Google Scholar]
- [2].Dowdle WR. The principles of disease elimination and eradication. Bull World Health Organ. 1998;76(Suppl 2):22–25. [PMC free article] [PubMed] [Google Scholar]
- [3].WHO . Global measles and rubella strategic plan: 2012-2020. Geneva, Switzerland: World Health Organization; 2012. [Google Scholar]
- [4].Centrul Național de Supraveghere și Control al Bolilor Transmisibile . Analiza evoluției bolilor transmisibile aflate în supraveghere. Raport pentru anul 2015. 2016. [cited 2019 September02]. Available from: http://cnscbt.ro/index.php/rapoarte-anuale/549-analiza-evolutiei-bolilor-transmisibile-aflate-in-supraveghere-raport-pentru-anul-2015/file
- [5].Lazar M, Stanescu A, Penedos AR, et al. Characterisation of measles after the introduction of the combined measles-mumps-rubella (MMR) vaccine in 2004 with focus on the laboratory data, 2016 to 2019 outbreak, Romania. Euro Surveill. 2019;24(29). DOI: 10.2807/1560-7917.ES.2019.24.29.1900041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Dascalu S. Measles epidemics in Romania: lessons for public health and future policy. Front Public Health. 2019;7:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Luminos M, Săndulescu O. Measles in perspective – lessons learned from the ongoing outbreak in Romania. J Contemp Clin Pract. 2017;4(2):46. [Google Scholar]
- [8].World Health Organization . WHO-recommended surveillance standard of measles. [cited 2019 August14]. Available from: https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/active/measles_standards/en/
- [9].Commission implementing decision (EU) 2018/945 of 22 June 2018 on the communicable diseases and related special health issues to be covered by epidemiological surveillance as well as relevant case definitions OJ.L 170(6.7.2018):p. 30; 2018.
- [10].Centrul Național de Supraveghere și Control al Bolilor Transmisibile . Situația rujeolei în România la data de 26.07.2019; 2019. [cited 2019 July31]. Available from: http://cnscbt.ro/index.php/informari-saptamanale/rujeola-1/1223-situatia-rujeolei-in-romania-la-data-de-26-07-2019/file
- [11].Centrul Național de Supraveghere și Control al Bolilor Transmisibile . Situația deceselor datorate rujeolei, România 2016-2019; 2019. [cited 2019 September01]. Available from: http://cnscbt.ro/index.php/informari-saptamanale/rujeola-1/1071-situatia-deceselor-datorate-rujeolei-romania-2016-2019/file
- [12].Centrul Național de Supraveghere și Control al Bolilor Transmisibile . Situația rujeolei în România la data de 14.12.2018; 2018. [cited 2019 July31]. Available from: https://www.cnscbt.ro/index.php/informari-saptamanale/rujeola-1/1035-situatia-rujeolei-in-romania-la-data-de-14-12-2018/file
- [13].Fiasca F, Necozione S, Fabiani L, et al. Measles-related hospitalizations in Italy, 2004-2016: the importance of high vaccination coverage. Ann Glob Health. 2019;85(1):40 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Centrul Național de Supraveghere și Control al Bolilor Transmisibile . Analiza evoluției bolilor transmisibile aflate în supraveghere. Raport pentru anul 2016. 2017. [cited 2019 September02]. Available from: http://www.cnscbt.ro/index.php/rapoarte-anuale/779-analiza-evolutiei-bolilor-transmisibile-aflate-in-supraveghere-raport-pentru-anul-2016/file
- [15].Centrul Național de Supraveghere și Control al Bolilor Transmisibile . Analiza evoluției bolilor transmisibile aflate în supraveghere. Raport pentru anul 2017. 2018. [cited 2019 September02]. Available from: http://www.cnscbt.ro/index.php/rapoarte-anuale/1003-analiza-evolutiei-bolilor-transmisibile-aflate-in-supraveghere-raport-pentru-anul-2017/file
- [16].World Health Organization . Measles, 1st dose (MCV1). Immunization coverage estimates. 2017. [cited 2017 August29]. Available from: http://apps.who.int/gho/data/view.main.81100?lang=en
- [17].Săndulescu O. Measles – worldwide burden of a vaccine-preventable disease. Rev Aeronaut Med Psychol. 2017;21(3,80):14–18. [Google Scholar]
- [18].Centrul Național de Supraveghere și Control al Bolilor Transmisibile . Situația rujeolei în România la data de 17.11.2017. 2017. [cited 2019 September01]. Available from: http://cnscbt.ro/index.php/informari-saptamanale/rujeola-1/799-situatia-rujeolei-in-romania-la-data-de-17-11-2017/file
- [19].Centrul Național de Supraveghere și Control al Bolilor Transmisibile . Analiza rezultatelor estimării acoperirii vaccinale la vârsta de 18 luni pentru copiii născuți în luna iulie, 2017. 2019. [cited 2019 September02]. Available from: http://cnscbt.ro/index.php/analiza-date-supraveghere/evaluarea-acoperirii-vaccinale/1200-analiza-rezultatelor-estimarii-acoperirii-vaccinale-cu-dt-si-cu-2-doze-rro-1/file
- [20].Centrul Național de Supraveghere și Control al Bolilor Transmisibile . Analiza rezultatelor estimării acoperirii vaccinale cu 2 doze RRO la vârsta de 5 ani, și cu dT la vârsta de 14 ani. 2019. [cited 2019 August31]. Available from: http://cnscbt.ro/index.php/analiza-date-supraveghere/evaluarea-acoperirii-vaccinale/1200-analiza-rezultatelor-estimarii-acoperirii-vaccinale-cu-dt-si-cu-2-doze-rro-1/file
- [21].Ruhanya V, Moyo SR. Measles laboratory-based surveillance in Zimbabwe during 2004-2009. GERMS. 2012;2(2):36–42 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hester G, Nickel A, LeBlanc J, et al. Measles hospitalizations at a United States children’s hospital 2011-2017. Pediatr Infect Dis J. 2019;38(6):547–552. 00006454-201906000-00001 [pii]. [DOI] [PubMed] [Google Scholar]
- [23].Cornelissen L, Grammens T, Leenen S, et al. High number of hospitalisations and non-classical presentations: lessons learned from a measles outbreak in 2017, Belgium. Epidemiol Infect. 2020;148:e35 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author [OS] upon reasonable request.


