Abstract
Entry receptor for SARS-CoV-2 is expressed in nasal epithelial cells, and nasal delivery pathway can be a key feature of transmission. Here, a possibility of interaction of SARS-CoV-2 with air pollution particulate matter (PM) was considered. It was shown in our recent studies that water-suspended plastic and wood smoke aerosol PM and carbon-containing nanoparticles from burning organics can interact with the plasma membrane of brain nerve terminals presumably due to their lipid components. COVID-19 patients have neurological symptoms, viral particles were found in the brain, SARS-CoV-2 enters the cells via fusion of lipid viral envelope with the plasma membranes of infected cells, and so viral envelop can contain lipid components of the host neuronal membranes. Therefore, interaction of SARS-CoV-2 envelope with PM is possible in water surrounding. After drying, PM can serve as a carrier for transmission of SARS-CoV-2 immobilized at their surface. Moreover, PM and SARS-CoV-2 per se can enter human organism during nasal inhalation, and they both use the same nose-to-brain delivery pathways moving along axons directly to the brain, influencing the nervous system and exocytosis/endocytosis in nerve cells. Thus, PM can aggravate neurological symptoms of SARS-CoV-2 and vice versa, due to their identical nose-to-brain delivery mechanism and possible interference of neuronal effects. In addition, different types of PM because of their ability to interact with the plasma membranes of nerve cells can facilitate unspecific SARS-CoV-2 entrance to the cells, and can influence envelope features of SARS-CoV-2. Detailed studies are required to analyze interaction of SARS-CoV-2 with PM.
Keywords: COVID -19, SARS-CoV-2, Coronavirus, Virus transmission, Viral envelope, Lipid membrane, Air pollution particulate matter, Smoke aerosol, Brain, Nerve terminals, Trans-synaptic transfer
Introduction
The coronavirus disease 2019 (COVID-19) is provoked by one of the highly pathogenic human coronaviruses (CoVs), severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (World Health Organization 2020a, b). Virions of coronaviruses measure ~ 120 nm in diameter (The Editors of Encyclopaedia Britannica 2020). Assembled intracellular SARS-CoV-2 virions were between 70 and 90 nm inside of Vero cells (Kim et al. 2020).
COVID-19 has rapid transmission rates (Behla et al. 2020). Literature data regarding ways of SARS-CoV-2 transmission are contradictory and still debated. Transmission of SARS-CoV-2 via aerosol droplets naturally produced by human is plausible, since the virus can remain viable and infectious in aerosols for hours, and beside that SARS-CoV-2 is viable on surfaces up to days (Doremalen et al. 2020). Entry receptor for SARS-CoV-2, angiotensin-converting enzyme 2 (ACE2) (Behla et al. 2020), and entry-associated protease TMPRSS2 are greatly expressed in nasal goblet and ciliated cells, and so nasal carriage was suggested to be a key feature of transmission (Sungnak et al. 2020). Alternatively, SARS-CoV-2-containing aerosol droplets can land on surfaces and people by touching these contaminated surfaces become infected (World Health Organization 2020a, b). SARS-CoV was detected in wastewater, but a low stability in the environment was suggested, and also CoVs and in particular SARS-CoV-2 were identified in the fecal of infected patients, and so a possibility of waterborne transmission needs to be analyzed (La Rosa et al. 2020).
CoVs are large enveloped non-segmented positive-sense RNA viruses (Li et al. 2020). Viral envelopes consist of proteins and lipid components, and enveloped viruses require the fusion of their lipid envelope with the host cell membrane to entry the infected cells (Millet and Whittaker 2018). CoVs display a large degree of plasticity regarding the entry pathways that can occur at the plasma membrane and through the endocytic pathway (Millet and Whittaker 2018). Protein components of SARS-CoV-2 envelope are in the focus of current research, in particular spike glycoprotein (S), which belongs to class I fusion protein, and is responsible for both binding to the receptor on the host cell and the fusion of host and viral membranes (Belouzard et al. 2012).
In this study, we have suggested that lipid constituents of the viral envelope can be very important for unspecific interaction of viral particles with different surfaces, including air pollution particulate matter (PM). It should be emphasized that this interaction capability can be inherent mainly to enveloped viruses. Recently, it was confirmed that air pollution PM can travel across border for a long distance and inhalation with fine and ultrafine PM (the aerodynamic diameter is less than 2.5 μm and 0.1 μm, respectively) is associated with many diseases, including neurological ones (Landrigan et al. 2018).
Based on our recent studies on interaction of different types of nano- and micro-sized particles, including water-suspended fine and ultrafine smoke aerosol PM, with the plasma membrane of brain nerve terminals, presumably their lipid components (Borysov et al. 2020; Shelestov et al. 2020; Borisova 2019), we supposed that air pollution PM can interact in water surrounding with envelope of SARS-CoV-2 composed of viral proteins and membrane fragments of infected nerve cells. Arguments in favor of this suggestion were analyzed.
Presentation of the concerns
Possibility of interaction of air pollution PM with envelope of SARS-CoV-2 and its uncontrolled transmission
Patients with COVID-19 have respiratory distress and neurologic signs. A growing body of evidences demonstrates that neurotropism is a common feature of CoVs, and transfection of SARS-CoV-2 is accompanied with neurological symptoms, and SARS-CoV-2 invades the central nervous system inducing neurological diseases (Li et al. 2020). In both patients and experimental animals, the CoV infection has been found in different brain regions (Netland et al. 2008; Li et al. 2016, 2020), and in transgenic for ACE2 mice, the brain was a main target organ for infection (Netland et al. 2008). Detailed analysis of neurologic manifestation of patients with COVID-19 in Wuhan, China, was performed (Mao et al. 2020). In this study, manifestations of the central nervous system, i.e., dizziness, headache, impaired consciousness (which includes the change of consciousness level (somnolence, stupor, coma), and content (confusion and delirium)), acute cerebrovascular disease, ataxia, and seizure, and also manifestations of the peripheral nervous system, i.e., taste, smell, vision impairment, and nerve pain, as well as skeletal muscular injury were examined. It was shown that 36.4% of COVID-19 patients had neurologic symptoms, which were more common in severe infected patients (45.5%) (Mao et al. 2020). In the mice infected with low inoculum doses of MERS-CoV, virus particles were identified in the brain only (not in the lung) (Li et al. 2016; Li et al. 2020). It is urgent to understand whether SARS-CoV-2 can provoke neuronal injury leading to the acute respiratory distress (Li et al. 2020).
In our earlier studies, a capability of fine/ultrafine water-suspended plastic and wood smoke PM and different types of micro- and nano-sized particles to interact with the plasma membrane of brain nerve terminals, and so to disturb a plasma membrane integrity and key synaptic characteristics, was shown (Borysov et al. 2020; Shelestov et al. 2020). It was revealed that water-suspended plastic and wood smoke PM depolarized the plasma membrane (Borysov et al. 2020; Shelestov et al. 2020), and carbon nano-sized particles from burning organics (the main components of air pollution PM), as well as maghemite nanoparticles affected the membrane integrity, thereby increasing leakage of excitatory and inhibitory neurotransmitters, glutamate, and GABA, respectively, and enhancing their ambient levels in nerve terminal preparations (Borisova et al. 2015; Borisova et al. 2016; Borisova et al. 2017; Borisova 2018, 2019). In particular, maghemite nanoparticles (0.75 mg/ml) did so by 36%, and carbon nano-sized particles (1.0 mg/ml) by 47% (Borisova 2019). Whereas, natural aluminosilicate particles (Pozdnyakova et al. 2017) did not alter significantly the integrity of the plasma membrane of nerve terminals. Therefore, different types of air pollution PM demonstrated various efficacies to interact with and affect the integrity of the cellular plasma membranes. Interaction of above particles and nerve terminals occurred mainly due to their lipid components that were confirmed by parallel experiments using the artificial planar lipid membrane (Borisova 2019).
CoVs have envelopes composed of viral proteins and membrane fragments of infected cells. As the central nervous system, and in particular, synaptic transmission are targeted by SARS-CoV-2 (Li et al. 2020), its envelope can contain lipid components of the host neuronal membranes. Taking into account that definite types of air pollution PM can interact with the plasma membrane of nerve cells (Borysov et al. 2020; Shelestov et al. 2020; Borisova et al. 2015; Borisova et al. 2017; Borisova 2018, 2019), it can be suggested that SARS-CoV-2 due to presence of neuronal membrane fragments in their envelopes can also interact with PM in water surrounding in a similar way. Air pollution PM and SARS-CoV-2 can form complex in water surrounding, where PM after drying can serve as a carrier for both short- and long-distance transportation of the virus, including outdoor and indoor one. Therefore, a possibility of unspecific interaction of SARS-CoV-2 envelope with air pollution PM and so its transmission and transfection being immobilized at the PM surface were considered. Different envelope compositions and size of viruses can influence their capability and efficiency to form complex with PM. Despite the fact that PM concentrations in the air were decreased due to reduced anthropogenic activity during quarantine, residual PM can be enough to perform carrier service for SARS-CoV-2; moreover, exact virus infection doses are still not identified.
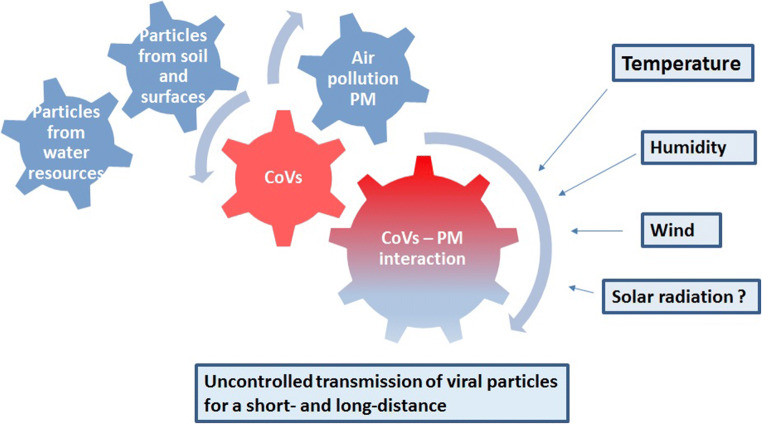
There are non-numerous literature data that can be considered in support of this suggestion. The effect of fine dust concentrations in the air in the Republic of Korea (2016–2017) on the incidence of viral respiratory infections caused by the human coronavirus, respiratory syncytial virus, human metapneumovirus, adenovirus, rhinovirus, human bocavirus, human parainfluenza virus, and influenza virus was investigated. It was concluded that when the weekly average concentration of fine dust increased, the incidence of infections by the human coronavirus, human metapneumovirus, adenovirus, human bocavirus, human parainfluenza virus, and influenza also increased (Cheon et al. 2019). In the USA, the majority of the positive cases of highly pathogenic avian influenza (HPAI) H5N2 might have received airborne virus carried by fine air pollution PM, and these results provide insights into the risk of airborne transmission of HPAI virus via fine dust particles (Zhao et al. 2019). In Beijing, China, association between daily PM2.5 (PM with size lesser than 2.5 μm) and influenza-like illness ILI risk was investigated using a generalized additive model. A strong positive relationship between PM2.5 and ILI risk at the flu season was established, but the effect of PM2.5 differed across age groups (Feng et al. 2016). Simply moving around in buildings was considered a significant source of human exposure to PM, potentially contaminated with Sin Nombre virus (SNV), during spring and summer seasons (Richardson et al. 2013). In 2003, investigation of SARS-CoV-1 victims revealed that patients were twice to die in regions where air pollution was high rather than low, and even in moderately polluted regions, the risk of dying was 84% higher (Niranjan 2020). Kabir et al. (2020) underlined that besides air pollution, several environmental factors, e.g., temperature and humidity, can influence the COVID-19 transmission pattern (Kabir et al. 2020). SARS-CoV’s transmissibility is comparable with that of influenza virus, the occurrence of which markedly elevates with high relative humidity and low temperatures (Park et al. 2020; Kabir et al. 2020). Also, further studies are needed to test solar ultraviolet radiation sensitivity of environmental SARS-CoV-2 (Seyer and Sanlidag 2020) (Fig.1).
Fig. 1.
Interaction of air pollution PM with CoVs and uncontrolled transmission
Air pollution PM can module SARS-CoV-2 viability and its interaction with the cells
The question arose whether or not immobilization at the surface of different types of air pollution PM can influence SARS-CoV-2 viability. Literature data showed that SARS-CoV-2 was more stable on plastic and stainless steel surfaces, and viable virus was detected up to 72 h after application to these surfaces (Doremalen et al. 2020). In this context, it can be suggested that immobilization of SARS-CoV-2 at the surface of definite types of air pollution PM can potentially favor virus viability.
SARS-CoVs, and in particular SARS-CoV-2, recognize ACE2 as a host binding receptor for viral S protein (Sungnak et al. 2020). It can be hypothesized that definite types of air pollution PM can facilitate SARS-CoV-2 entrance to the cells, when the virus acts as a component of PM complex. Plastic and wood smoke aerosol PM, and especially their carbon components, can be of special attention because they considerably disturb the properties and integrity of the cellular plasma membrane (Borysov et al. 2020; Shelestov et al. 2020). Acting as a complex with this PM, SARS-CoV-2 can cross the cellular plasma membranes and reach the cytoplasm avoiding specific ACE2-dependent mechanism of viral transmission. Vice versa, this PM per se due to ability to interact with cellular membranes can influence SARS-CoV-2 envelope properties. Therefore, potential increase/decrease in viral viability during interaction with different types of air pollution PM was suggested, where PM immobilizing virus can be a carrier for its transmission through the cellular membranes.
Air pollution PM can enhance neurological symptoms and influence trans-synaptic transfer of SARS-CoV-2
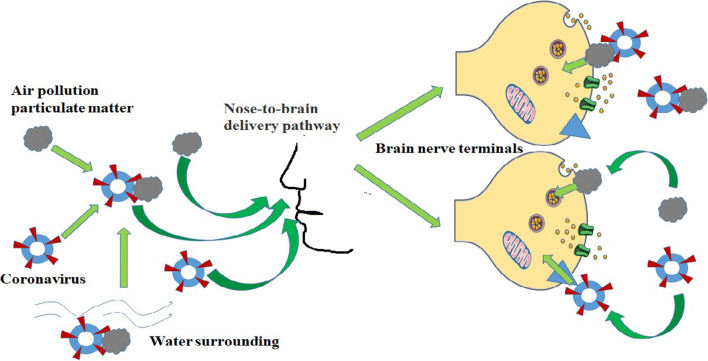
On one hand, during nasal inhalation, air pollution PM reaches olfactory caves and moves along axon of olfactory nerves directly to the brain avoiding the blood-brain barrier (Oberdörster et al. 2005). On the other hand, CoV-induced neurological symptoms may have resulted from movement of viral particles through axons that consequently targets synaptic neurotransmission (Li et al. 2020). Using transgenic mice, it has been shown that SARS-CoV and MERS-CoV administrated intranasally can rapidly spread transneuronally from the olfactory bulb to connected brain areas causing neuronal loss (Netland et al. 2008; Li et al. 2016; Li et al. 2020). In this context, nose-to-brain delivery is a common pathway of air pollution PM and CoVs (Fig. 2).
Fig. 2.
Interference of the nose-to-brain delivery pathways of air pollution PM and SARS-CoV-2 and their effects in brain nerve terminals
Increasing evidence shows that CoVs may first invade peripheral nerve terminals and then gain access to the central nervous system via a synapse-connected route (Li et al. 2020). Also, some CoVs are able to spread via a synapse-connected route to the medullary cardiorespiratory center from the mechanoreceptors and chemoreceptors in the lung and lower respiratory airways (Netland et al. 2008; Li et al. 2020). Ultrastructural studies have demonstrated that transfer of HEV 67N between neurons occurred via the clathrin-mediated endocytic/exocytic pathway (Li et al. 2013). The trans-synaptic transfer has been well documented for CoVs and avian bronchitis virus (Li et al. 2020). Inside the cells, SARS-CoV-2 was observed in a wide range of intracellular organelles, especially in vesicles (Kim et al. 2020). SARS-CoV-2 release does not require cell lysis, and thus the virus might exploit existing secretory pathways (Sungnak et al. 2020). It has been suggested that animal death may have resulted from dysfunction and/or death of infected neurons, which are an extremely susceptible target for SARS-CoV (Netland et al. 2008).
It was demonstrated in our recent studies that water-suspended smoke PM influenced exocytosis in nerve terminals. In particular, plastic smoke PM (Borysov et al. 2020) and carbon-containing nanoparticles from burning organics (Borisova et al. 2015; Borisova et al. 2017) decreased an exocytic release of neurotransmitters glutamate and GABA from brain nerve terminals. Presumably, nano-sized smoke PM and carbon-containing nanoparticles can enter synaptic vesicles in nerve terminals, thereby impairing neurotransmitter storage and exocytic release. It can be speculated that when the synaptic machinery does not receive required neurotransmitters from the exocytic release, it can provoke more intensive stimulation of release episodes via different regulatory mechanisms, thereby aggravating synaptic transmission damage.
Air pollution PM influencing exocytosis in nerve terminals can in turn change transfer of CoVs between neurons. In case of synaptic neurotransmission modulation, they can act independently and/or as a complex SARS-CoV-2-PM (Fig. 2). It should be noted that viral particles are larger than synaptic vesicles, which are approximately 40 nm in diameter. It is more plausible that SARS-CoV-2-PM may have disturbed synaptic vesicle recycling during exo-/endocytosis. Facilitation of membrane activity of the viral particles can be expected when they act as a complex with definite types of PM (for instance, nano-sized plastic and wood smoke PM, which have already possessed these properties) that in turn may have more pronounced effects on exocytosis and vesicle recycling.
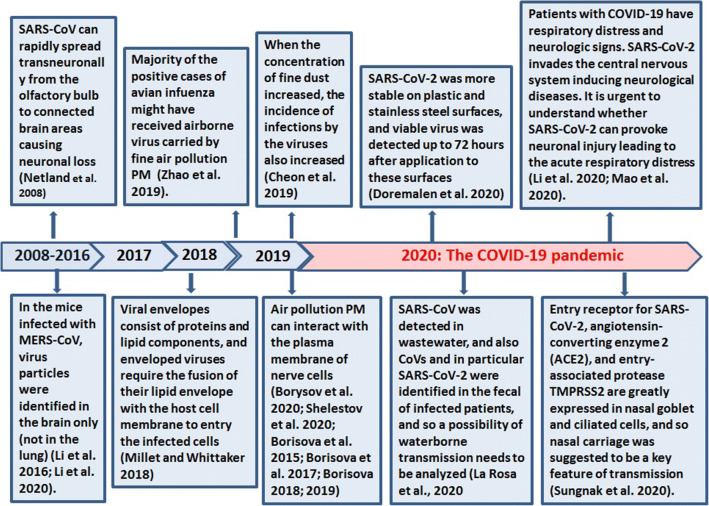
Therefore, air pollution PM and CoVs have the same nose-to-brain delivery pathways and target synaptic transmission, and so their neurological effects can interfere and aggravate each other and can be additive or even synergetic (Fig. 2). A chronologic timeline diagram of important research milestones is presented in Fig. 3.
Fig. 3.
Important milestones: a chronologic timeline diagram
Conclusions
In summary, a possibility of SARS-CoV-2 envelope to interact in water surrounding with air pollution PM, which in turn becomes a carrier for short- and long-distance virus transmission, including outdoor and indoor one, was suggested. Besides that, definite types of PM can facilitate SARS-CoV-2 transportation across the cellular plasma membranes and can influence viability of SARS-CoV-2 immobilized at their surface. PM and CoVs per se can enter human organism during nasal inhalation, and they both use the same nose-to-brain delivery pathways, and exocytosis for trans-synaptic transfer that can favor interference of their neurological effects. Detailed studies are required to confirm or decline above suggestions regarding air pollution PM and SARS-CoV-2 interaction.
Authors’ Contributions
Tatiana Borisova and Serhiy Komisanenko − conceptualization of study. Tatiana Borisova developed the design of the manuscript and prepared draft manuscript and figures. Tatiana Borisova and Serhiy Komisarenko designed the final manuscript structure, reviewed the scientific literature, and supervised the final version of the manuscript. The authors read and approved the final manuscript.
Funding
This work was supported by the grant of National Research Foundation of Ukraine # 2020.02/0147; PI: Prof. T. Borisova.
Data availability
Not applicable.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Behla T, Kaur I, Bungau S, Kumar A, Uddin MS, Kumar C, Palf G, Sahil, Shrivastava K, Zengin G, Arora S. The dual impact of ACE2 in COVID-19 and ironical actions in geriatrics and pediatrics with possible therapeutic solutions. Life Sci. 2020;257(15):118075. doi: 10.1016/j.lfs.2020.118075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belouzard S, Millet JK, Licitra BN, Whittaker GR. Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses. 2012;4(6):1011–1033. doi: 10.3390/v4061011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borisova T. Nervous system injury in response to contact with environmental, engineered and planetary micro- and nano-sized particles. Front Physiol. 2018;9:728. doi: 10.3389/fphys.2018.00728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borisova T (2019) Express assessment of neurotoxicity of particles of planetary and interstellar dust. npj Microgravity 5(2). 10.1038/s41526-019-0062-7 [DOI] [PMC free article] [PubMed]
- Borisova T, Nazarova A, Dekaliuk M, Krisanova N, Pozdnyakova N, Borysov A, Sivko R, Demchenko AP. Neuromodulatory properties of fluorescent carbon dots: effect on exocytotic release, uptake and ambient level of glutamate and GABA in brain nerve terminals. Int J Biochem Cell Biol. 2015;59:203–215. doi: 10.1016/j.biocel.2014.11.016. [DOI] [PubMed] [Google Scholar]
- Borisova T, Borysov A, Pastukhov A, Krisanova N. Dynamic gradient of glutamate across the membrane: glutamate/aspartate-induced changes in the ambient level of L-[14C]glutamate and D-[3H]aspartate in rat brain nerve terminals. Cell Mol Neurobiol. 2016;36(8):1229–1240. doi: 10.1007/s10571-015-0321-4. [DOI] [PubMed] [Google Scholar]
- Borisova T, Dekaliuk M, Pozdnyakova N, Pastukhov A, Dudarenko M, Borysov A, Vari SG, Demchenko AP. Harmful impact on presynaptic glutamate and GABA transport by carbon dots synthesized from sulfur-containing carbohydrate precursor. Environ Sci Pollut Res. 2017;24(21):17688–17700. doi: 10.1007/s11356-017-9414-6. [DOI] [PubMed] [Google Scholar]
- Borysov A, Tarasenko A, Krisanova N, Pozdnyakova N, Pastukhov A, Dudarenko M, Paliienko K, Borisova T. Plastic smoke aerosol: nano-sized particle distribution, absorption/fluorescent properties, dysregulation of oxidative processes and synaptic transmission in rat brain nerve terminals. Environ Pollut. 2020;263(Part A):114502. doi: 10.1016/j.envpol.2020.114502. [DOI] [PubMed] [Google Scholar]
- Cheon JM, Yang YJ, Yoon YS, Lee ES, et al. Influence of fine particulate dust particulate matter 10 on respiratory virus infection in the Republic of Korea. Korean J Fam Pract. 2019;9(5):454–459. doi: 10.21215/kjfp.2019.9.5.454. [DOI] [Google Scholar]
- Doremalen N, Bushmaker T, Morris DH et al (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med:NEJMc2004973. 10.1056/NEJMc2004973 [DOI] [PMC free article] [PubMed]
- Feng C, Li J, Sun W, Zhang Y, Wang Q. Impact of ambient fine particulate matter (PM2.5) exposure on the risk of influenza-like-illness: a time-series analysis in Beijing, China. Environ Health. 2016;15:17. doi: 10.1186/s12940-016-0115-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabir MT, Uddin MS, Hossain MF, Abdulhakim JA, Alam MA, Ashraf GM, Bungau SG, Bin-Jumah MN, Abdel-Daim MM, Aleya L. nCOVID-19 pandemic: from molecular pathogenesis to potential investigational therapeutics. Front Cell Dev Biol. 2020;8:616. doi: 10.3389/fcell.2020.00616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JM, Chung YS, Jo HJ, Lee NJ, et al. Identification of coronavirus isolated from a patient in Korea with COVID-19. Osong Public Health Res Perspect. 2020;11(1):3–7. doi: 10.24171/j.phrp.2020.11.1.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Rosa G, Bonadonna L, Lucentini L, Kenmoe S, Suffredini E. Coronavirus in water environments: occurrence, persistence and concentration methods - A scoping review. Water Res. 2020;179:115899. doi: 10.1016/j.watres.2020.115899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrigan PJ, Fuller R, Acosta NJR, Adeyi O, Arnold R, Basu N, et al. The Lancet Commission on pollution and health. Lancet. 2018;391:462–512. doi: 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- Li YC, Bai WZ, Hirano N, Hayashida T, Taniguchi T, Sugita Y, Tohyama K, Hashikawa T. Neurotropic virus tracing suggests a membranous-coating-mediated mechanism for transsynaptic communication. J Comp Neurol. 2013;521:203–212. doi: 10.1002/cne.23171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li K, Wohlford-Lenane C, Perlman S, Zhao J, Jewell AK, Reznikov LR, Gibson-Corley KN, Meyerholz DK, McCray PB., Jr Middle East respiratory syndrome coronavirus causes multiple organ damage and lethal disease in mice transgenic for human dipeptidyl peptidase 4. J Infect Dis. 2016;213:712–722. doi: 10.1093/infdis/jiv499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li YC, Bai WZ, Hashikawa T (2020) The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 10.1002/jmv.25728 [DOI] [PMC free article] [PubMed]
- Mao L, Wang M, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Li Y, Jin H, Hu B (2020) Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. MedRxiv. 10.1101/2020.02.22.20026500
- Millet JK, Whittaker GR. Physiological and molecular triggers for SARS-CoV membrane fusion and entry into host cells. Virology. 2018;517:3–8. doi: 10.1016/j.virol.2017.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82:7264–7275. doi: 10.1128/JVI.00737-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niranjan A (2020) Coronavirus: air pollution might raise risk of fatality 2020 Environment, EcoWatch, Environmental News for a Healthier Planet and Life https://www.ecowatch.com/coronavirus-air-pollution-fatality-2645656760.html. Accessed 7 Apr 2020
- Oberdörster G, Oberdörster E, Oberdörster J. Nanotoxicology: an emerging discipline evolving from studies of ultrafine particles. Environ Health Perspect. 2005;113:823–839. doi: 10.1289/ehp.7339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park JE, Son WS, Ryu Y, Choi SB, Kwon O, Ahn I. Effects of temperature, humidity, and diurnal temperature range on influenza incidence in a temperate region. Influenza Other Respir Viruses. 2020;14:11–18. doi: 10.1111/irv.12682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pozdnyakova N, Pastukhov A, Dudarenko M, Borysov A, Krisanova N, Nazarova A, Borisova T. Enrichment of inorganic Martian dust simulant with carbon component can provoke neurotoxicity. Microgravity Sci Technol. 2017;29:133–144. doi: 10.1007/s12217-016-9533-6. [DOI] [Google Scholar]
- Richardson KS, Kuenzi A, Douglass RJ, Hart J, Carver S. Human exposure to particulate matter potentially contaminated with sin nombre virus. Ecohealth. 2013;10(2):159–165. doi: 10.1007/s10393-013-0830-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seyer A, Sanlidag T. Solar ultraviolet radiation sensitivity of SARS-CoV-2. Lancet Microbe. 2020;1:e8–e9. doi: 10.1016/S2666-5247(20)30013-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelestov A, Kolotii A, Borisova T, Turos O, Milinevsky G, Gomilko I, Bulanay T, Fedorov O, Shumilo L, Pidgorodetska L, Kolos L, Borysov A, Pozdnyakova N, Chunikhin A, Dudarenko M, Petrosian A, Danylevsky V, Miatselskaya N, Choliy V. Essential variables for air quality estimation. Int J Digit Earth. 2020;13(2):278–298. doi: 10.1080/17538947.2019.1620881. [DOI] [Google Scholar]
- Sungnak W, Huang N, Bécavin C, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26:681–687. doi: 10.1038/s41591-020-0868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Editors of Encyclopaedia Britannica (2020). Coronavirus. Chicago, Illinois, U.S: Encyclopaedia Britannica, inc
- World Health Organization (2020a) Naming the coronavirus disease (COVID-19) and the virus that causes it. https://www.who.int/emergencies/diseases/ novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease- (covid-2019)-and-the-virus-that-causes-it (2020)
- World Health Organization (2020b) Coronavirus disease 2019 (COVID-19) Situation Report – 66 https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200326-sitrep-66-covid-19.pdf. Accessed 26 Mar 2020
- Zhao Y, Richardson B, Takle E, Chai L, Schmitt D, Win H. Airborne transmission may have played a role in the spread of 2015 highly pathogenic avian influenza outbreaks in the United States. Sci Rep. 2019;9:11755. doi: 10.1038/s41598-019-47788-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.