Figure 4.
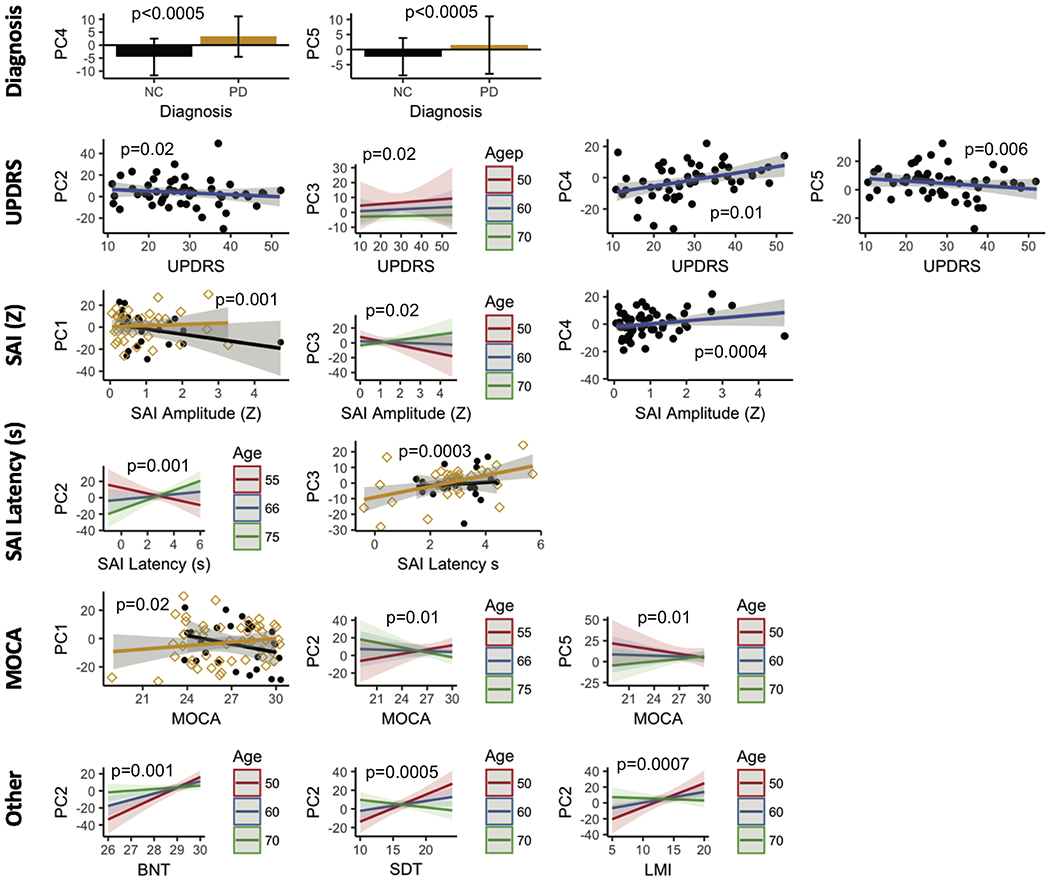
The PCs in the OFF condition were tested for association with diagnosis, MDS-UPDRS, SAI measures, and cognitive performance while adjusting for age and gender. PC 4 and PC 5 contributed to the PDRP network in the OFF state. PC 4 significantly (p<0.0005) discriminated controls form PD participants in the OFF condition. PC 5 was strongly associated with age (p=0.003). Lower PC 2 and PC 5 scores were associated with high MDS-UPDRs scores (PC 2, p= 0.02; PC5, p = 0.006). PC 4 showed the opposite trend (p =0.01 ). While high PC 3 scores were associated with high UPDRS scores, they decreased with age (p = 0.02 ). Higher PC 1 scores were associated with low SAI amplitude only in PD participants (p = 0.001). This relationship was observed for all participants for PC 3 but decreased with age (p = 0.02). Higher PC4 scores were associated with higher SAI amplitude (p = 0.0004). Lower PC 2 scores were associated with SAI latency, with this relationship reversing with increasing age (p = 0.0001). Lower PC 3 scores were associated with shorter latency times on SAI in controls only (p = 0.003 ). PC 1 showed opposite correlations with MOCA scores (p = 0.03). Higher PC 2 scores were associated with higher MOCA scores, but this relationship reversed with age(p = 0.01). The exact opposite behavior was observed with PC 5 (p = 0.01). BNT, SDT, and LMI scores were all positively correlated with PC 2. This correlation reduced or even reversed with age in all tests. (p-value; BNT = 0.001, SDT <0.0005, LMI = 0.0007).
