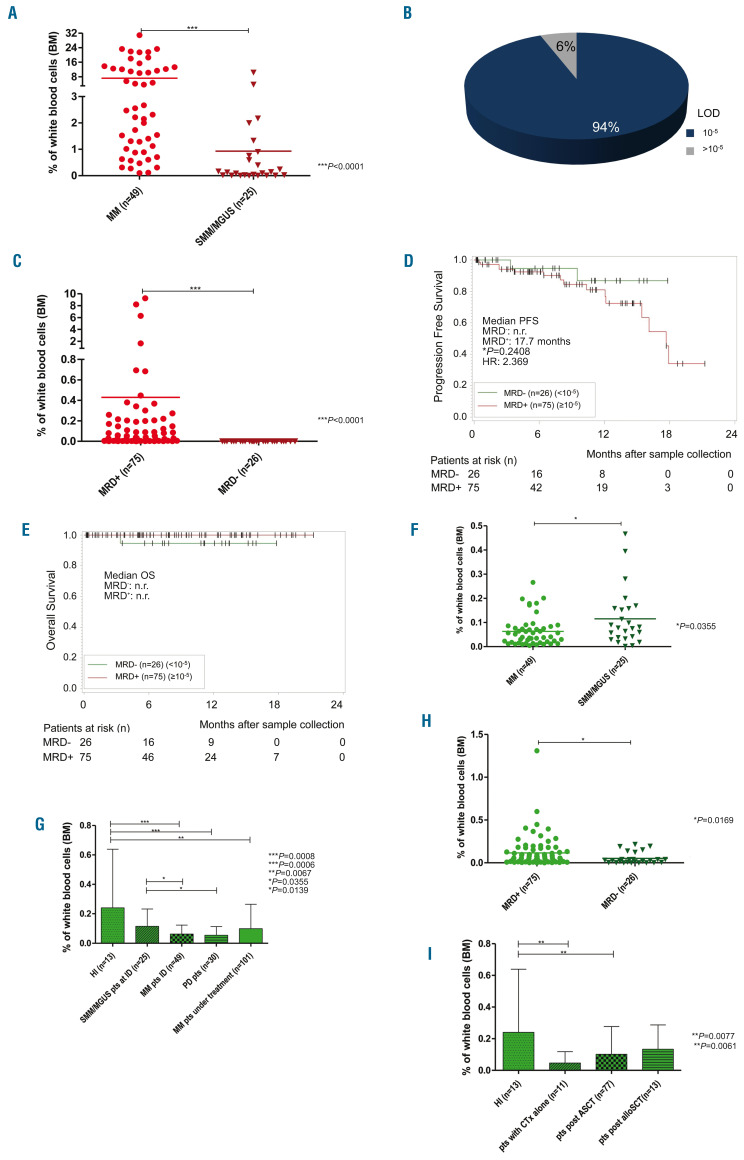
Figure 2.
The level of aberrant and normal plasma cells in bone marrow samples and the influence of minimal residual disease detection on the outcome of patients. (A) Patients’ samples at initial diagnosis were divided into two groups: those from patients with multiple myeloma (MM) in need of treatment and those from patients with smoldering multiple myeloma (SMM)/monoclonal gammopathy of undetermined significance (MGUS) not in need of treatment. As expected, the percentage of aberrant plasma cells (aPC) was significantly higher (***P<0.0001) in MM samples (n=49) than in SMM/MGUS samples (n=25). (B) In 94% of all minimal residual disease (MRD) samples (n=101) the limit of detection and a sensitivity of 10-5 could be reached. (C) Patients’ samples after treatment were divided into two groups: MRD+ (≥10-5) and MRD– (<10-5). The percentages of aPC in MRD+ samples (n=75) were, expectedly, significantly higher (***P<0.0001) than those in MRD– samples (n=26). (D) Post-therapy bone marrow samples were divided into MRD+ (≥0.001% aPC among total nucleated cells) and MRD– (<0.001% aPC among total nucleated cells) to estimate progression-free survival. The estimated median progression-free survival, determined using the Kaplan-Meier method, was 17.7 months for MRD+ patients (n=75) and not reached for MRD– patients (n=26) (P=0.2408). The hazard ratio was 2.369 (95% confidence interval: 0.54-10.50). (E) Overall survival was determined for the MRD– (n=26) and MRD+ (n=75) cohort. A big difference could not be observed because only one event was censored. [(F) Patients’ samples at initial diagnosis were divided into those from patients with MM in need of treatment and those from patients with SMM/MGUS not in need of treatment. Interestingly, the percentages of normal plasma cells (nPC) were significantly higher (*P=0.0355) in SMM/MGUS patients than in MM patients. (G) Comparing nPC in healthy individuals (HI) and MM patients at different stages of the disease, the percentages of nPC in HI (n=13) were significantly higher (***P=0.0008) than those from MM patients at initial diagnosis (n=49), with progressive disease (n=30) (***P=0.0006) or under treatment (n=101) (**P=0.0067). Patients at initial diagnosis of SMM/MGUS (n=25) had significantly higher percentages of nPC compared to MM patients at initial diagnosis (*P=0.0355) or during progressive disease (*P=0.0139). No significant differences were observed between SMM/MGUS patients and HI or patients under treatment or among MM patients at initial diagnosis, during progression and under treatment. (H) Patients’ samples after treatment were divided into MRD+ (≥0.001% aPC among total nucleated cells) and MRD– (<0.001% aPC among total nucleated cells). The percentages of nPC were significantly higher (*P=0.0169) in MRD+ samples than in MRD– samples. (I) Comparing nPC numbers in HI and patients treated with different modalities, the percentages of nPC were significantly higher in HI (n=13) than in patients after treatment with standard chemotherapy (n=11) (**P=0.0077) or after autologous stem cell transplantation (n=77) (**P=0.0061). No significant differences were observed between nPC numbers in HI and patients after allogeneic stem cell transplantation (n=13) or among the groups treated with the different modalities. The graphs show the mean (A, C, F, H) or mean ± standard deviation (G, I), Mann-Whitney U-test (A, C, F-I), and Kaplan-Meier method (D, E). BM: bone marrow; LOD: limit of detection; PFS: progression-free survival; n.r.: not reached; HR: hazard ratio; n: number; OS: overall survival; pts: patients; ID: initial diagnosis; PD: progressive disease; CTx: standard chemotherapy; ASCT: autologous stem cell transplantation; alloSCT: allogeneic stem cell transplantation.]