Abstract
Background
In conflict settings, data to guide humanitarian and development responses are often scarce. Although geospatial analyses have been used to estimate health-care access in many countries, such techniques have not been widely applied to inform real-time operations in protracted health emergencies. Doing so could provide a more robust approach for identifying and prioritising populations in need, targeting assistance, and assessing impact. We aimed to use geospatial analyses to overcome such data gaps in Yemen, the site of one of the world's worst ongoing humanitarian crises.
Methods
We derived geospatial coordinates, functionality, and service availability data for Yemen health facilities from the Health Resources and Services Availability Monitoring System assessment done by WHO and the Yemen Ministry of Public Health and Population. We modelled population spatial distribution using high-resolution satellite imagery, UN population estimates, and census data. A road network grid was built from OpenStreetMap and satellite data and modified using UN Yemen Logistics Cluster data and other datasets to account for lines of conflict and road accessibility. Using this information, we created a geospatial network model to deduce the travel time of Yemeni people to their nearest health-care facilities.
Findings
In 2018, we estimated that nearly 8·8 million (30·6%) of the total estimated Yemeni population of 28·7 million people lived more than 30-min travel time from the nearest fully or partially functional public primary health-care facility, and more than 12·1 million (42·4%) Yemeni people lived more than 1 h from the nearest fully or partially functional public hospital, assuming access to motorised transport. We found that access varied widely by district and type of health service, with almost 40% of the population living more than 2 h from comprehensive emergency obstetric and surgical care. We identified and ranked districts according to the number of people living beyond acceptable travel times to facilities and services. We found substantial variability in access and that many front-line districts were among those with the poorest access.
Interpretation
These findings provide the most comprehensive estimates of geographical access to health care in Yemen since the outbreak of the current conflict, and they provide proof of concept for how geospatial techniques can be used to address data gaps and rigorously inform health programming. Such information is of crucial importance for humanitarian and development organisations seeking to improve effectiveness and accountability.
Funding
Global Financing Facility for Women, Children, and Adolescents Trust Fund; Development and Data Science grant; and the Yemen Emergency Health and Nutrition Project, a partnership between the World Bank, UNICEF, and WHO.
Introduction
Since 2015, Yemen has faced one of the world's most devastating armed conflicts. More than 100 000 people have been killed, 3·6 million internally displaced, and nearly 80% of the country's almost 30 million people requires humanitarian assistance.1, 2 In 2018, the conflict in Yemen was named the world's worst humanitarian crisis, with nearly half of the country's population on the brink of famine and hundreds of thousands affected by cholera.3, 4 The ongoing conflict has severely affected the country's health-care system: barely half of public health facilities are fully functional; salaries for health-care workers went unpaid from October, 2016, to early 2019; and essential medications and equipment are in short supply or absent.5
As humanitarian and development agencies seek to support health-care delivery in Yemen, timely and reliable data on the health system and access to care are essential, but hard to obtain. The most recent Yemen Demographic and Health Survey, the gold standard for public health information in most low-income and middle-income countries, was done in 2013, well before the escalation of conflict.6 No comprehensive national or district level estimates of health-care access or household surveys have been completed since 2013. The dynamic nature of the conflict—shifting front lines, new offensives, ongoing displacement, and changing disease burdens—has complicated efforts to prioritise and target assistance.
Research in context.
Evidence before this study
Timely and accurate data are crucial for guiding humanitarian and development assistance in protracted conflict settings, yet such data are often lacking. The conflict in Yemen, now in its 6th year, has severely impacted the country's health system, but data on access to health care remain scarce. No national, governorate, or regional-level estimates exist to quantify the number of people with poor access to health facilities or specific services, or to determine the locations where the largest number of people have inadequate access. Although geospatial analytics have been used to estimate access to care and inform policy making in many countries, these techniques have not been widely applied in conflict settings to inform humanitarian and development responses. We searched PubMed, Google Scholar, and grey literature in the Humanitarian Data Exchange repository for articles in English related to the use of geospatial analyses in humanitarian health emergencies and conflict settings between Jan 1, 2006, and Dec 1, 2019. We used the search terms “geospatial”, “health”, “healthcare”, “humanitarian”, “development”, AND “armed conflict”, as well as the names of specific countries classified as fragile or conflict-affected by the World Bank since 2006. We also searched more broadly for examples of geospatial analyses used for health policy and planning from non-conflict settings focusing on the measurement of access to care. Articles unrelated to the health sector were excluded.
Added value of this study
We developed a novel geospatial model to estimate access to health care in Yemen that calculates travel times to public health-care facilities and health services from any point in the country. To do so, we compiled a geospatial database of hospitals and primary care facilities containing geocoordinates, functionality, and service availability data. Using UN population estimates, satellite data, and census figures, we developed up-to-date, high-resolution population spatial distribution maps for Yemen. We built a digital road network map using satellite imagery that incorporated road closures and lines of conflict to account for the impact of conflict on population movements. Based on these inputs, a novel geospatial analytical model yielded estimates of walk and drive times to: functional hospitals and primary care facilities; and specific health services. We found, and quantified the degree to which, a large proportion of the population of Yemen faces challenges with geographical access to care. We found that access varied widely by type of service and district, and we ranked districts in terms of poorest access to care by headcount and percentage.
Implications of all the available evidence
To our knowledge, these findings provide the first comprehensive estimates of access to health care in Yemen since the current conflict began. They provide national and district level estimates of access to functional health facilities and key health services. Moreover, they provide proof of concept for how operational data and geospatial techniques can be combined to address data needs and answer key questions around access in these settings. We argue that the use of geospatial techniques offers a data-driven, methodologically rigorous approach for planning and targeting assistance that could have profound implications for humanitarian and development responses.
These challenges are not unique to Yemen. Recent responses to humanitarian emergencies have been characterised by data shortcomings that limit efforts to target programming and assess effectiveness.7, 8, 9 In many protracted conflicts, baseline health system data are lacking, public health information systems are weak, and data that are collected are of low quality, fragmented, and inconsistent.7, 8 Additionally, data collection has become more difficult owing to administrative and movement restrictions, violence against data collectors, and other such limitations.10
Addressing these data challenges is essential to improving the effectiveness and accountability of international assistance. One potential approach, largely unrealised in protracted health emergencies, involves using geospatial analytics to identify populations in need and improve targeting of health services and resources. Over the past decade, geospatial analyses have become increasingly commonplace in policy planning for resource allocation in many low-income and middle-income countries, as well as high-income countries.11, 12 Several key inputs are required for these analyses: geocoordinates of health facilities; comprehensive road network maps; and high-resolution population spatial distribution data. Using this approach, health authorities have identified where geographical access to health care is poor, thereby enabling more equitable and efficient allocation of resources.11
Such techniques, in theory, could be used to strengthen responses to humanitarian health emergencies and protracted conflicts. In practice, however, geospatial analytics have made little progress in these contexts. Necessary data on facility functionality, service availability, population location, and road networks are often unknown, incomplete, or outdated. Moreover, to the extent that humanitarians have applied geospatial techniques in health responses, the focus has largely been on thematic mapping, that is, making maps showing basic geocoded information or simple relationships.13 Some progress has been made using geospatial techniques to track population movements after natural disasters (eg, Nepal in 2015), model infectious disease outbreaks, and estimate mortality in conflict-affected settings.14, 15 However, beyond these applications, geospatial analytics remain under-utilised in the humanitarian health sector, particularly for generating data to guide real-time decision making around service delivery and health system planning.13
In this Article, we aim to provide proof of concept for how geospatial analytics, coupled with operational data on facility functionality, service availability, road accessibility, and lines of conflict, can be used to address data gaps amid an active armed conflict such as that in Yemen. We produce national and district level estimates of access to care and propose that these outputs could substantially inform the targeting and effectiveness of assistance, as well as strengthen efforts to support the resilience of affected health systems.
Methods
Assembling a geolocated inventory of health facility locations
We derived latitude and longitude coordinates for public primary health-care facilities and hospitals from the 2018 Health Resources and Services Availability Monitoring System (HeRAMS). This assessment was done by WHO and the Yemen Ministry of Public Health and Population (appendix p 3) and contains data on facility location, functionality, and service availability, including antenatal care, illness in children younger than 5 years, malnutrition, emergency obstetric care, and surgery, all of which are services relevant to the Yemen Minimum Service Package for Health.16 Facility locations were verified when possible by cross checking them against third-party monitoring data collected by the Yemen Emergency Health and Nutrition Project, implemented by WHO, UNICEF, and the World Bank. Discrepancies between HeRAMS and third-party data were reviewed and reconciled.
Population data
To model updated population distribution, we implemented widely adopted geospatial modelling approaches developed by WorldPop (appendix p 4).17 Previous WorldPop population mapping in Yemen involved the integration of the 2004 census data with urban extents defined by Moderate Resolution Imaging Spectroradiometer (MODIS) satellite imagery and 2010 district-level population estimates,18 matching similar mapping elsewhere.19, 20 Because major population movements and growth have occurred in Yemen since 2010, these existing datasets were outdated and required substantial revision.
Estimates of 2018 district populations from the UN Office for the Coordination of Humanitarian Affairs (OCHA) were the basis for the new mapping. The modelling process focused on disaggregating these estimates to a spatial resolution of 100 m by 100 m. UN OCHA national and district boundaries were obtained from the Humanitarian Data Exchange.21 The locations of 112 974 villages and settlements enumerated and mapped in the 2004 census were obtained, with the population count of each village or settlement matched to an associated point location. Additionally, the footprints of major cities and towns were obtained from two global satellite-derived datasets: the Global Human Settlement Layer (GHSL), derived from 2014 Landsat imagery; and the Global Urban Footprint (GUF), derived from 2012 synthetic-aperture radar imagery.22
GHSL uses more recent imagery and captures urban growth more effectively, whereas GUF uses more detailed imagery and different mapping algorithms, identifying smaller settlements more precisely. Therefore, the two datasets were combined to make a joint settlement footprint dataset aligned to the WorldPop master grid. Because the GHSL-GUF combined dataset only captured cities, towns, and large villages, it missed a substantial proportion of small villages important for mapping rural populations. To rectify this, the 2004 census dataset was integrated to capture these smaller settlements. The 2004 village and settlement totals per district were rescaled to match the 2018 estimates to provide new per-village estimates.
Estimates were generated for the total population of Yemen at a 100 m spatial resolution. Population centres aggregated to 1 km by 1 km cells were used as the starting points for all journeys. We transformed the aggregated product to a vector layer of points, with each point representing the centroid of a 1 km2 grid cell. These points were subsequently used as origins in network analyses and consisted of more than 500 000 points.
Road network data
After conducting a baseline review of the Yemen road network in OpenStreetMap, additional roads were digitised and disconnected roads were joined to the main network to create a network that could be queried for travel times between points. We added missing paved roads and connected large settlements to the main network based on satellite imagery from DigitalGlobe imagery, as provided to the OpenStreetMap project. Raw data was obtained from Geofabrik,23 retaining street-type or way-type objects with a highway tag, signalling that they were roads. This raw inventory was refined by removing all road objects not tagged with one of several acceptable road types, then cleaning road geometries to remove interstitial nodes and non-intersections, using a process modified from the Python package OSMnx.24 Finally, we split road sections into 2 km sections to improve network snapping fidelity. The final road network is shown in the appendix (p 5).
Elevation data
We used elevation data gathered by NASA's Shuttle Radar Topography Mission25 to determine the elevation of each tile in the WorldPop population layer previously described. Elevation estimates were then used to modify walk time estimates to and from the main network.
Network analysis
In our basic model, each journey had three segments: a walk from the origin point to the nearest node on the network; a driving portion along the road system; and a walk from the nearest node to the final destination. The two walking segments assume straight-line movement from point to point, with walk speed adjusted for elevation changes according to Tobler's hiking function, with a maximum off-road walk speed set at 4 km/h, based on estimates by in-country partners. Driving portions assume that the traveller always moves at the speed limit while on the road network.
We modelled all possible journeys to health-care facilities individually along our network graph and calculated weighted shortest-path journeys. All processing steps were executed in Python (version 3.6). We used the lesser of the travel time calculated using this method (walk plus drive plus walk) and the direct straight-line walking time from origin to destination. This adjustment becomes relevant in areas where road network coverage is sparse and the distance to the nearest network node is large. We repeated this calculation for each origin point to all potential destinations (health facilities); from this set we take the minimum as the minimum access time to service for that origin.
Multiple access time thresholds were modelled: less than 30 min, less than 60 min, less than 120 min, and less than 240 min. These thresholds were based upon published guidelines for hospital and primary care planning and discussions with Yemen ground partners.26, 27
Modifications to incorporate conflict dynamics
Given the fragility of the Yemen conflict, we incorporated several novel dynamic variables into the model to reflect the impact of conflict on access to health-care services. The variables included road closures, lines of conflict, and mode of transportation.
The UN Logistics Cluster routinely collects information on road closures and restrictions due to conflict. We used the January 2019 dataset (to reflect year-end 2018) by intersecting their road network with our own and modifying travel speeds. Closed roads in the UN model resulted in a reduction in travel speeds by 100% in our model (road impassable); restricted roads reduced travel speeds by 50%. Information on lines of conflict was obtained from ground partners, reflecting the state of conflict between December, 2018, and January, 2019. We assumed these lines to be impassable by civilians and incorporated this assumption into the model by preventing hypothetical journeys from crossing such lines at any point. These lines effectively split Yemen into five contiguous areas in the model, such that each acts as its own self-contained network. To estimate accessibility when there is no access to a vehicle, we assigned a flat walking speed of 6 km/h along roads and hold all other assumptions constant (off-road walking speed remained the same at 4 km/h).
No personal health information was collected. Ethics committee approval was not necessary.
Role of funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
We identified 275 hospitals and 4767 primary health-care facilities, for a total of 5042 health facilities in Yemen in 2018. Of the hospitals, 149 (54%) were fully functional and 98 (36%) were partially functional; of the primary health-care facilities, 2416 (51%) were fully functional and 1651 (35%) were partially functional. We verified geocoordinates for 3806 (88%) of the 4314 functional or partially functional hospital and primary health-care facilities, based on HERAMS data triangulated against third-party monitoring data. The gross locations of these facilities are illustrated in the appendix (p 3).
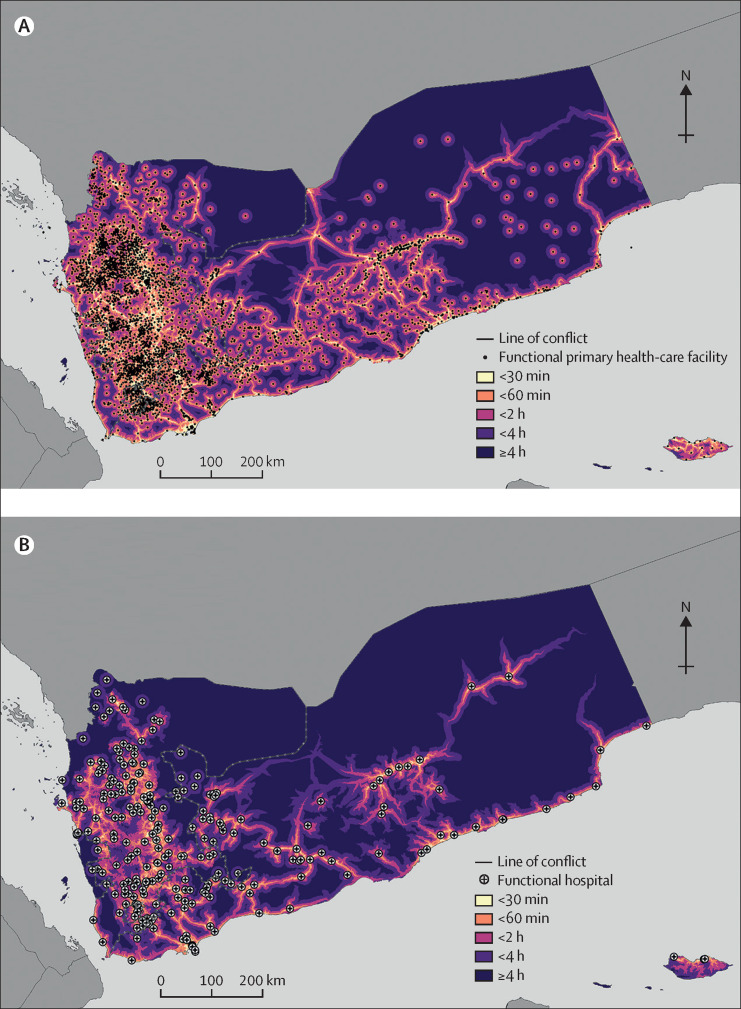
We produced national-level estimates of access to health-care facilities by calculating travel times to the nearest partially or fully functional primary-care facility or hospital from any point in Yemen, assuming access to motorised transport. For primary-care facilities, of a total estimated population of 28 670 616, we estimated that 19 899 047 (69·4%) people lived within 30 min of the nearest partially or fully functional primary health-care facility; 26 056 626 (90·9%) people lived within 60 min of a facility; and 28 224 303 (98·4%) people lived within 120 min of a facility (table 1 ; figure 1A ). For hospitals, we estimated that 10 717 094 (37·4%) people of the population lived within 30 min of a partially or fully functioning hospital; 16 525 186 (57·6%) people lived within 60 min of a hospital; and 23 087 916 (80·5%) people lived within 120 min of a hospital (table 1; figure 1B).
Table 1.
Population living within specified travel time of health facilities assuming motorised transport
|
Nearest primary health-care facility |
Nearest hospital |
|||||
|---|---|---|---|---|---|---|
| Headcount | Proportion of country population, % | District mean, % (SD) | Headcount | Proportion of country population, % | District mean, % (SD) | |
| <30 min | 19 899 047 | 69·4% | 62·3% (23·7) | 10 717 094 | 37·4% | 26·2% (31·1) |
| <60 min | 26 056 626 | 90·9% | 85·6% (18·5) | 16 525 186 | 57·6% | 45·6% (34·2) |
| <120 min | 28 224 303 | 98·4% | 95·2% (12·2) | 23 087 916 | 80·5% | 68·8% (34·2) |
Figure 1.
Travel time to the nearest functional or partially functional public primary health-care facility (A) and hospital (B), 2018
At the district level, we found that access to functional health facilities varied widely among districts, in both percentage and absolute terms. Across Yemen's 333 districts, we found that the proportion of the population in each district living less than 30 min from a primary health-care facility ranged from 0% to 100%, with a mean of 62·3% (SD 23·7; IQR 47·3–79·2); the proportion living less than 1 h away from a hospital ranged from 0% to 100%, with a mean of 45·6% (SD 34·2; IQR 15·4–77·1).
We ranked districts according to the absolute number of individuals with poor access according to defined threshold times to health care (appendix p 8). Thresholds were defined as 1 h for primary care and 2 h for hospital care, reflecting WHO standards and consultations regarding acceptable travel times in Yemen.18 Headcount maps by district, with districts shaded in terms of the absolute number of people living beyond these thresholds, are provided in the appendix (pp 6, 7). The districts with the greatest number of people living beyond these thresholds are shown in the appendix (p 8). We found that in 29 districts, more than 20 000 people lived further than 1 h from a primary health-care facility; and in six districts, more than 50 000 people lived further than 1 h. At the hospital level, we found that in 93 districts, more than 20 000 people lived further than 2 h from the nearest hospital; in 24 districts, more than 50 000 people lived further than 2 h; and in five districts, more than 100 000 people lived further than 2 h.
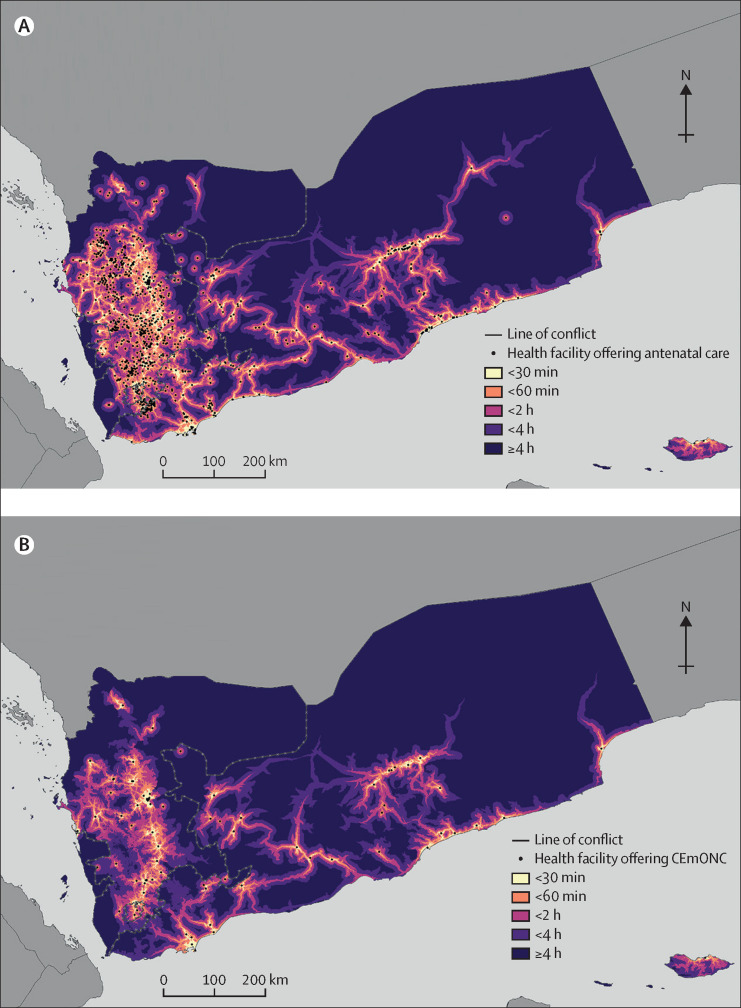
We next modelled geographical access to key health services. We found poor access overall for many services, with substantial variability by service type (table 2 ; figure 2 ). Access was highest for immunisations and malnutrition services, with 17 914 659 and 17 923 044 individuals (62·5% of the population for both categories) living within a 30-min travel to these services, followed by care of children younger than 5 years (15 416 499 people; 53·8% of the population) and antenatal care (13 028 648 people; 45·4%). By contrast, only 9 833 012 (34·3%) people could access basic emergency obstetric care, 8 078 568 (29·2%) people could access emergency obstetric care, and 7 916 210 (27·6%) people could access emergency surgery within 30-min travel time. Roughly a third of the population lived more than 1 h away from antenatal care, and nearly half lived more than 1 h away from basic emergency obstetric care. Only 17 867 326 (62·3%) and 17 641 386 (61·5%) Yemenis lived within 2-h travel time of comprehensive emergency obstetric care or surgery services. Service accessibility also varied widely among districts; in the bottom quartile of districts, for example, less than a third of the population lived within 2 h of basic emergency obstetric care, whereas in the top quartile, more than 95% of the population did. This district-level variation was seen across all service types.
Table 2.
National and district level estimates of access to specific health services
|
Within 30-min travel time |
Within 60-min travel time |
Within 120-min travel time |
||||
|---|---|---|---|---|---|---|
| Headcount and proportion of country population, % | District mean, % (SD) | Headcount and proportion of country population, % | District mean, % (SD) | Headcount and proportion of country population, % | District mean, % (SD) | |
| Antenatal care | 13 028 648; 45·4% | 32·3% (32·1) | 19 481 946; 68·0% | 53·1% (35·8) | 24 560 013; 85·7% | 72·8% (35·1) |
| Treatment of illnesses in children younger than 5 years | 15 416 499; 53·8% | 42·3% (31·7) | 22 080 371; 77·0% | 66·1% (31·8) | 26 380 278; 92·0% | 83·8% (26·6) |
| Malnutrition treatment | 17 923 044; 62·5% | 51·6% (29·3) | 24 492 014; 85·4% | 85·6% (28·6) | 27 346 004; 95·4% | 95·3% (23·1) |
| Immunisations | 17 914 659; 62·5% | 53·0% (28·2) | 24 402 008; 85·1% | 76·3% (27·2) | 27 438 633; 95·7% | 89·7% (21·7) |
| Basic emergency obstetric care | 9 833 012; 34·3% | 22·7% (31·7) | 15 224 443; 53·1% | 40·4% (35·7) | 21 734 649; 75·8% | 63·9% (37·1) |
| Comprehensive emergency obstetric and neonatal care | 8 358 690; 29·2% | 16·8% (31·6) | 11 983 950; 41·8% | 27·9% (36·5) | 17 867 326; 62·3% | 48·6% (40·3) |
| Emergency surgery | 7 916 210; 27·6% | 15·6% (31·3) | 11 510 094; 40·1% | 26·0% (36·0) | 17 641 386; 61·5% | 46·8 (40·3) |
Figure 2.
Travel time to the nearest health facility offering antenatal care (A) and comprehensive emergency obstetric and neonatal care (B)
CEmONC=comprehensive emergency obstetric and neonatal care.
Finally, we reran the analysis assuming no access to motorised transport (appendix p 9), given that exit survey data from WHO and UNICEF supported facilities in Yemen indicate that many patients are accessing facilities by foot. In this iteration, travel times to care increased and access decreased substantially. Assuming travel on foot only, only 55% of the population lived within 30 min of a primary health-care facility (vs 97% who lived within 120-min travel time). At the hospital level, only 17% of the population lived within a 30-min walk to a hospital (with 52% within 120 min).
Discussion
Using a novel geospatial analysis, we report the first population-level estimates of access to health care in Yemen since the outbreak of the current conflict. We compiled geocoordinates of health facilities and obtained satellite imagery, UN operational and third-party monitoring data, and other datasets to generate updated road network maps and high-resolution spatial population distribution estimates. To our knowledge, these estimates are the first to reflect key infrastructure and demographic changes (eg, internal displacement) since the conflict. These inputs were analysed using geospatial network analytics to produce estimates of access to primary health-care facilities, hospitals, and key health services. These estimates identified the location and magnitude of populations with limited access to health care to a much greater degree of spatial resolution than previously available.
We found, and quantified the degree to which, a large proportion of the population of Yemen faces challenges with accessing care. In 2018, nearly 8·8 million people (30·6% of Yemenis) were estimated to live more than a 30-min travel time from the nearest partially or fully functional public primary health-care facility, and approximately 12·1 million people (42·4% of Yemenis) lived more than 1 h from the nearest partially or fully functional public hospital. Access varied widely by district, which we ranked in terms of access deprivation. Of the districts with the largest number of people with poor geographical access to care, the majority are front-line districts, reflecting access challenges faced by civilians living close to armed conflict.
We found that access varied widely by type of health service, underscoring the reality that access to a functional health facility does not guarantee access to a specific service. Access was particularly poor for resource-intensive, hospital-based services, with slightly less than 40% of the population living more than a 2-h drive from comprehensive emergency obstetric care and surgical care, as well as for certain essential outpatient services, such as antenatal care. For patients who lack access to motorised transport, we found that their access is poorer still: assuming walking only, roughly 45% of Yemenis live more than a 30-min walk to the nearest functional primary health-care facility, and 68% live more than a 60-min walk to the nearest functional hospital.
Operationally, these findings could be immediately useful to humanitarian and development responses within the country. First, although the Yemen humanitarian health cluster has identified 74 hard-to-reach districts based on reported barriers,26 the geospatial approach presented here, which analyses access from the population perspective, provides a much higher degree of spatial resolution of the size and locations of populations in need. Second, given that many organisations are earnestly investing in outreach programming to reach remote populations, these findings could immediately inform targeting decisions (eg, where to send community health workers or mobile teams). Third, because geospatial analytical models are adaptable, this analysis could be routinely updated to reflect changing ground conditions, for example, incorporating new data on road accessibility from the UN logistics cluster, service availability from field teams, and seasonality data. Fourth, these findings can help planners to respond more effectively to changing disease burdens. Findings from this work are already being used to model how COVID-19 might affect access to basic health-care services. Likewise, given that malnutrition and cholera have been major challenges in Yemen, understanding the geospatial relationship between disease outbreaks and accessibility to care could greatly inform efforts to locate disease-specific resources where they are needed most.
This approach is also highly relevant for organisations working in other conflict settings around the world. As previously discussed, although geospatial analyses are becoming increasingly commonplace in stable contexts, they remain underutilised in the humanitarian health space apart from basic thematic mapping, infectious disease modelling, and a handful of other research applications.13 If operationalised further, these tools could greatly inform resource allocation decisions that are too often based upon fragmented and incomplete data, with ramifications that affect millions.7, 8 With access to data becoming harder, the need for innovative evidence generation is real.10 The approach described here presents a novel means of combining ground-level operational data with geospatial techniques to address key data gaps and provides proof of concept for how such an approach can provide more comprehensive, timely analytics in conflict settings.
Finally, this type of analysis holds promise for strengthening monitoring and evaluation. In recent years, humanitarian and development organisations have faced growing calls to move beyond documenting inputs, such as numbers of kits or vaccines delivered, and focus more on measuring health outcomes and impact.28, 29 In the health sector, this would entail finding more rigorous ways to measure access, coverage, quality, affordability, and health outcomes associated with interventions. Such calculations often require accurate estimates of the population in need within a defined area (catchment zones, districts, governorates, etc). This geospatial approach provides one method for doing so. Moreover, this analysis could be repeated with serial datasets (eg, a 2020 version of HeRAMS is currently underway in Yemen) to measure changes in access over time and serve as a reference point for health system rebuilding.
We acknowledge several limitations with this work, as well as opportunities for more strongly incorporating geospatial analytics into humanitarian and development interventions. First, we recognise that determining who needs assistance, and where assistance is needed, is not simply a matter of geographical access. Epidemiological considerations are crucial, particularly in conflicts where disease outbreaks, injuries, and other health burdens can concentrate in specific areas.30 Organisations working in these contexts must take epidemiological trends into account, and future geospatial work should seek to incorporate geocoded epidemiological data, such as estimates of disease incidence and transmission trends. This approach would help identify not only areas with large populations who lack access to care, but also those affected by or at risk of specific disease burdens (population in need).
Second, we acknowledge that geographical access represents only one dimension of access and might overestimate true access. Populations living near a functional facility often face substantial utilisation barriers, such as lack of transportation, discrimination, security concerns, poor quality of care, and affordability. We modelled one of these barriers (lack of transportation) and found a sharp drop in access. However, each of these factors can affect care-seeking and should be further assessed to understand not only theoretical access, but actual utilisation. To that end, WHO, UNICEF, and the World Bank have invested in strengthening utilisation data collection in Yemen and are working to analyse the access–utilisation relationship.
Third, we acknowledge limitations with the completeness and quality of some data, as well its reproducibility in other contexts. HeRAMS does not cover private sector facilities and might exclude temporary facilities and outreach activities, which can play a key part in improving access for remote populations. Future work should capture contributions from these modalities. Although GPS coordinates were obtained for nearly 90% of public health facilities in Yemen, facilities for which coordinates were not available were excluded, and some coordinates from HeRAMS were identified as incorrect, which required further investigation and verification using third-party monitors when possible. Moreover, HeRAMS is not available in all conflict-affected countries; however, there is growing interest in standardising these tools in such settings. The road network map, which includes more than 145 000 digitised segments, is extensive, but not every road was digitised, meaning that access might be underestimated in some areas. Finally, conflict is, by its nature, dynamic. The analysis presented here is a snapshot in time that should be updated as new data become available.
We also acknowledge the sensitivity around geocoded health data. Over the past decade, attacks on health-care workers and health facilities in conflict zones have proliferated.31 These attacks represent a violation of International Humanitarian Law, and despite efforts to curb them, they continue. We caution that geocoded data, particularly for health facilities, must be treated with utmost sensitivity, and that organisations involved in collecting data must be extremely thoughtful and deliberate about how such data are stored, shared, and used.
As protracted conflicts proliferate, there is growing need for accurate, timely data to guide humanitarian and development responses. In recent years, calls to strengthen public health information systems and improve data collection have increased. Such efforts are vital, but better data collection needs to be paired with more rigorous analytical approaches to improve accountability among organisations and populations at large. As the Yemen conflict continues, vulnerability in what was already one of the poorest countries in the world is growing. Understanding where assistance is needed, and assuring accountability to those in need, is more pressing than ever.
For the Global Human Settlement Layer see https://ghsl.jrc.ec.europa.eu/
For the DigitalGlobe see https://www.digitalglobe.com/
For the OpenStreetMap see https://www.openstreetmap.org/
For the WorldPop see https://www.worldpop.org/
For HeRAMS please see https://herams.org/
Acknowledgments
Acknowledgments
The authors alone are responsible for the views expressed in this Article and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated. This work was supported by: the Global Financing Facility for Women, Children, and Adolescents Trust Fund; a Decision and Delivery Science Support for Improved Universal Health Coverage grant, supported by a collaboration between the World Bank and Bill & Melinda Gates Foundation; and the Yemen Emergency Health and Nutrition Project, a partnership between the World Bank, UNICEF, and WHO. We thank Fouzia Shafique, former Chief of Health and Nutrition, UNICEF-Yemen; Altaf Musani, WHO Representative in Yemen; and Ernest Massiah, former World Bank Practice Manager, Health, Nutrition, and Population for the Middle East and North Africa Region, for their valuable support, insights, and contributions to this work. We would also like to acknowledge Manal Al-Hajji, geospatial analyst, for her contributions to the digitisation of the Yemeni road network.
Contributors
KG, CF, and MA were responsible for the study concept and design. KG, KO, MD, KH, NQ, LL-B, and KA-S collected and analysed the data. CF, AT, and KG were responsible for the geospatial analysis. All authors contributed to the manuscript writing and editing.
Declaration of interests
KG, CF, MA, NQ, LL-B, KA-S, KO, MD, and KH have worked on the bank-financed Yemen Emergency Health and Nutrition Project, a collaboration between the World Bank, WHO, and UNICEF that has supported the Yemen health system since 2017. AT declares no competing interests.
Supplementary Material
References
- 1.Armed Conflict Location & Event Data Project Press release: over 100,000 reported killed in Yemen war. 2019. https://www.acleddata.com/2019/10/31/press-release-over-100000-reported-killed-in-yemen-war/
- 2.International Organization for Migration IOM Yemen 2019 operational overview. 2019. https://reliefweb.int/report/yemen/iom-yemen-2019-operational-overview
- 3.UNHCR Yemen on the brink of famine. 2018. https://www.unrefugees.org/news/yemen-on-the-brink-of-famine/
- 4.Voice of America UN: Yemen has world's ‘worst humanitarian crisis’. https://learningenglish.voanews.com/a/un-officials-say-yemen-has-world-s-worst-humanitarian-crisis-/4847402.html
- 5.Devi S. Devastation in Yemen ongoing. Lancet. 2018;392:14–20. doi: 10.1016/S0140-6736(18)31607-6. [DOI] [PubMed] [Google Scholar]
- 6.Demographic and Health Survey Program Yemen Survey summary. https://dhsprogram.com/what-we-do/survey/survey-display-358.cfm
- 7.Checchi F, Warsame A, Treacy-Wong V, Polonsky J, van Ommeren M, Prudhon C. Public health information in crisis-affected populations: a review of methods and their use for advocacy and action. Lancet. 2017;390:2297–2313. doi: 10.1016/S0140-6736(17)30702-X. [DOI] [PubMed] [Google Scholar]
- 8.Samarasakera U, Horton R. Improving evidence for health in humanitarian crises. Lancet. 2017;390:18–24. doi: 10.1016/S0140-6736(17)31353-3. [DOI] [PubMed] [Google Scholar]
- 9.Diggle E, Welsch W, Sullivan R. The role of public health information in assistance to populations living in opposition and contested areas of Syria, 2012–2014. Confl Health. 2017;11:33. doi: 10.1186/s13031-017-0134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maxwell D, Hailey P, Spainhour B, Kim JJ. Feinstein International Center, Tufts University; Boston: 2019. Constrains and complexities of Information analysis in humanitarian emergencies: evidence from Yemen. [Google Scholar]
- 11.Juran S, Broer PN, Klug SJ. Geospatial mapping of access to timely essential surgery in sub-Saharan Africa. BMJ Glob Health. 2018;3 doi: 10.1136/bmjgh-2018-000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wagner Z, Heft-Neal S, Bhutta ZA, Black RE, Burke M, Bendavid E. Armed conflict and child mortality in Africa: a geospatial analysis. Lancet. 2018;392:857–865. doi: 10.1016/S0140-6736(18)31437-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenough PG, Nelson EL. Beyond mapping: a case for geospatial analytics in humanitarian health. Confl Health. 2019;13:50. doi: 10.1186/s13031-019-0234-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilson R, Zu Erbach-Schoenberg E, Albert M. Rapid and near real-time assessments of population displacement using mobile phone data following disasters: the 2015 Nepal earthquake. PLoS Curr. 2016;8 doi: 10.1371/currents.dis.d073fbece328e4c39087bc086d694b5c. ecurrents.dis.d073fbece328e4c39087bc086d694b5c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galway L, Bell N, Sae AS. A two-stage cluster sampling method using gridded population data, a GIS, and Google Earth (TM) imagery in a population-based mortality survey in Iraq. Int J Health Geogr. 2012;11:12. doi: 10.1186/1476-072X-11-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO The Minimum Service Package – a lifeline for the vulnerable in remote areas. Available at: http://www.emro.who.int/yem/yemen-news/the-minimum-service-package-a-lifeline-for-the-vulnerable-in-remote-areas.html
- 17.Tatem AJ. WorldPop, open data for spatial demography. Sci Data. 2017;4 doi: 10.1038/sdata.2017.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stevens FR, Gaughan AE, Linard C, Tatem AJ. Disaggregating census data for population mapping using random forests with remotely-sensed and ancillary data. PLoS One. 2015;10 doi: 10.1371/journal.pone.0107042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Linard C, Alegana VA, Noor AM, Snow RW, Tatem AJ. A high resolution spatial population database of Somalia for disease risk mapping. Int J Health Geogr. 2010;9:45. doi: 10.1186/1476-072X-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lloyd CT, Sorichetta A, Tatem AJ. High resolution global gridded data for use in population studies. Sci Data. 2017;4 doi: 10.1038/sdata.2017.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Humanitarian Data Exchange Yemen – administrative boundaries. https://data.humdata.org/dataset/yemen-admin-boundaries
- 22.DLR Earth Observation Center Global urban foortprint. https://www.dlr.de/eoc/en/desktopdefault.aspx/tabid-9628/16557_read-40454/
- 23.Geofabrik Our download server. 2020. https://www.geofabrik.de/data/download.html
- 24.Boeing G. OSMnx: new methods for acquiring, constructing, analyzing, and visualizing complex street networks. Computers Environment and Urban Systems. 2017;65:126–139. [Google Scholar]
- 25.Jet Propulsion Laboratory: California Institute of Technology U.S. releases enhanced shuttle land elevation data. https://www2.jpl.nasa.gov/srtm/
- 26.Meara JG, Leather AJ, Hagander L. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 27.WHO Yemen: health cluster bulletin. 2019. https://reliefweb.int/report/yemen/yemen-health-cluster-bulletin-may-2019
- 28.Akseer N, Salehi AS, Hossain SM. Achieving maternal and child health gains in Afghanistan: a Countdown to 2015 country case study. Lancet Glob Health. 2016;4:e395–e413. doi: 10.1016/S2214-109X(16)30002-X. [DOI] [PubMed] [Google Scholar]
- 29.Spiegel PB. The humanitarian system is not just broke, but broken: recommendations for future humanitarian action. Lancet. 2017 doi: 10.1016/S0140-6736(17)31278-3. published online June 8. [DOI] [PubMed] [Google Scholar]
- 30.Norris A, Hachey K, Curtis A, Bourdeaux M. Crippling violence: conflict and incident polio in Afghanistan. PLoS One. 2016;11 doi: 10.1371/journal.pone.0149074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.WHO . World Health Organization; Geneva: 2019. Attacks on health care initiative 2019–2022. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.