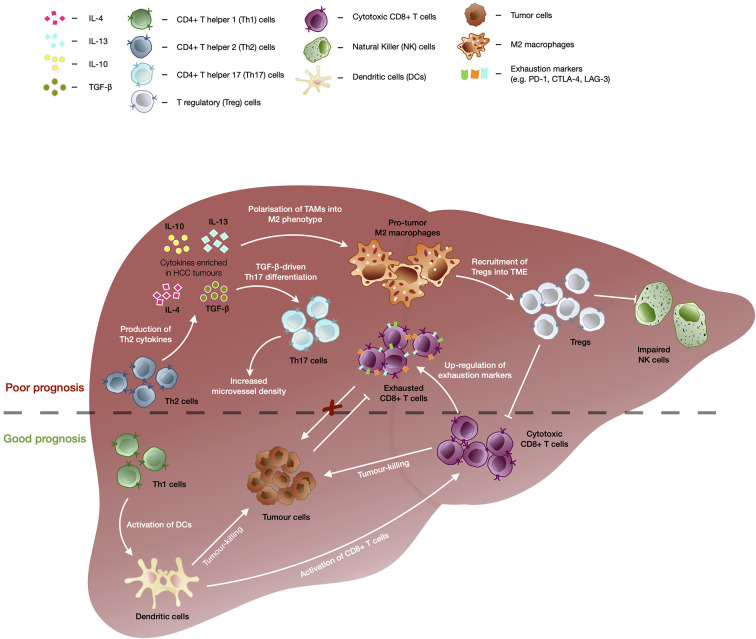
Figure 1.
The immunological events contributing to good versus bad prognosis in HCC. Enrichment of CD4+ T helper 2 (Th2) cells are associated with poor overall survival of HCC patients. TGF-β as well as cytokines secreted by Th2 such as IL-4, IL-10, and IL-13, drives the polarization of tumor-associated macrophages (TAMs) into immunosuppressive M2 macrophage phenotype which further recruits T regulatory cells (Tregs). Tregs in turn further enhances the immunosuppressive tumor microenvironment through inhibition of CD8+ T memory/effector cells’ and natural killer (NK) cells’ tumor-killing capacity, leading to poor prognosis in HCC. TGF-β also drives differentiation of CD4+ T helper 17 (Th17) cells and high frequencies of Th17 have been correlated with increased microvascular invasion and shorter OS and DFS of HCC patients. Presence of CD4+ T helper 1 (Th1) cells correlated with favorable outcomes in HCC as they are able to enhance activation of CD8+ T cells via dendritic cells (DC) and trigger DC-mediated tumor-killing. Despite the capability to kill tumor cells and association with good prognosis in HCC, CD8+ T cells showed upregulation of exhaustion markers (e.g. PD-1, CTLA-4, and LAG-3), which dampens its killing capacity in chronic conditions leading to tumor progression.