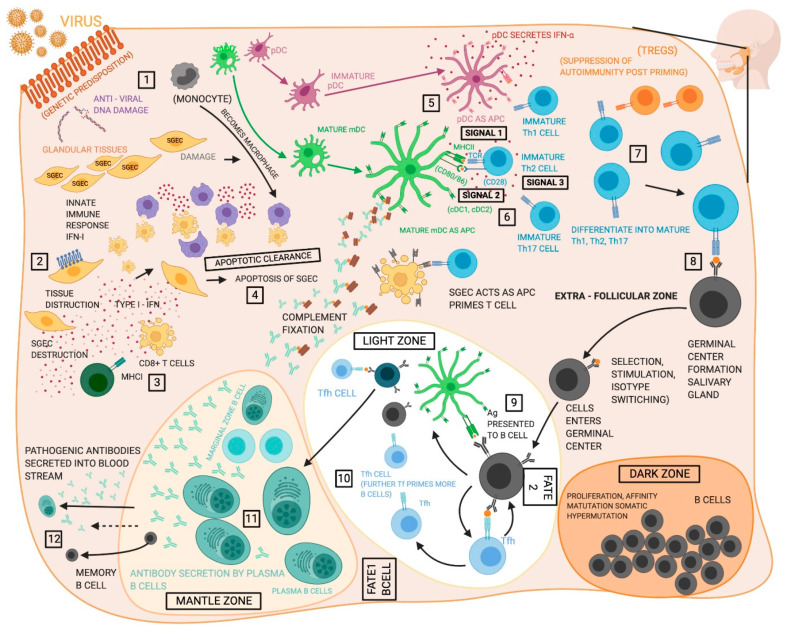
Figure 1.
Proposed functions of different cell types in the pathogenesis of Sjögren’s syndrome (SS). (1) The initiating events in the development of SS remain unclear, but evidence suggests the disease proceeds following an environmental trigger on a susceptible genetic background, likely a viral infection. (2) Salivary gland epithelia cells (SGECs) experience increased apoptosis and act as sources of inflammatory cytokines and chemokines within the salivary gland (SG). (3) CD8+ T cells are poorly understood in SS, but may contribute to tissue destruction in the glands. (4) Macrophages participate in tissue destruction through the release of proteases and cytokines and display reduced efferocytosis allowing unremoved apoptotic cells to act as sources of self-antigen. (5) Type I interferon (T1-IFN) both initiates antiviral activity and exerts an activating effect on cells of the immune system. T1-IFN is produced by multiple cell types but is closely associated with plasmacytoid DCs (pDCs). (6) Myeloid dendritic cells (mDCs) are the dominant antigen presenting cells to T cells, however, macrophages and SGECs also participate. (7) Antigen presentation allows for activation of CD8+ T cells and the Th1, Th2, and Th17 CD4+ T cell subsets, which can then contribute to various aspects of the disease pathology. Th1 cells enter the glands and compose much of the early infiltrates and exacerbate the inflammatory environment with the production of type II interferon, while Th17 cells play an increasingly well recognized role in SS as sources of cytokines including IL-17. Conflicting evidence has caused the roles of regulatory T cells (Tregs) remain indistinct in SS. Th2 cells support the humoral autoimmune response through cytokines incusing IL-4. (8 and 9) T follicular helper (Tfh) cells support B cell development in germinal centers (GC) that include follicular dendritic cell (fDC) networks. Germinal centers exist in the spleen, but about 25% of SS patients develop ectopic germinal centers in the SG containing Tfh and fDC. B cells in the germinal center undergo proliferation, somatic hypermutation and affinity hypermutation in the dark zone of the germinal center. (10) B cells then proceed to germinal center selection by fDCs in the light zone and either leave the germinal center as memory B cells or antibody producing plasma cells (Fate 1), or return to the dark zone for further affinity maturation (Fate 2). (11) The MZ B cells function as part of the adaptive immune system carrying antigens to the germinal centers for more efficient generation of memory B cells and glandular MZB cells are proliferative, activated, and produce autoantibodies. Lastly, (12) plasma cells exhibit hyperactivity and are responsible for the production of pathogenic autoantibodies. Created with BioRender.com.