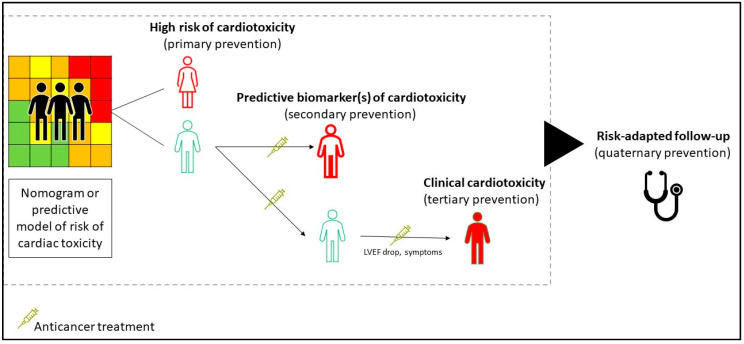
Figure 3.
Proposed framework to identify the critical points for medical interventions to prevent and treat cardiotoxicity. The identification of cancer patients that are more susceptible to cardiac toxicity can prompt the development of interventions of primary prevention, which is adjusted for cancer types, previous treatments, and planned therapies. Validating prognostic and predictive biomarkers is critical for defining the benefits of early interventions, based on quality endpoints of cardiovascular mortality. The current strategy of the management of cardio-toxicity commonly takes the form of a tertiary type, treating patients with functional-structural alterations and cardiovascular symptoms. Eventually, the risk-adapted plans of follow-up can reduce the excessive medicalization and medical harms.