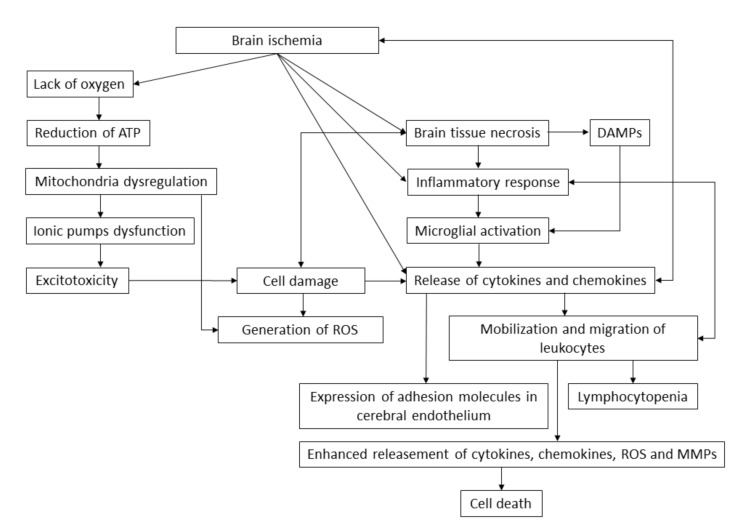
Figure 1.
The brain ischemia pathway. Brain ischemia causes shortages in the oxygen supply, brain tissue necrosis and release of cytokines and chemokines that cause an inflammatory response. Lack of oxygen causes the dysregulation of mitochondria and induces the anaerobic production of adenosine triphosphate (ATP), which generates the reactive oxygen species (ROS). Disorders in the concentration of ions cause excitotoxicity, which results in cell damage and brain tissue necrosis. Necrotic cells release damaged-associated molecular patterns (DAMPs), which induce the activation of microglia, resulting in a massive release of cytokines and chemokines. Pro-inflammatory factors mobilize leukocytes to migrate into the infarct zone enhancing the release of inflammatory response molecules. Cerebral endothelium is stimulated to express the adhesion molecules on its surface and accumulate the cells, narrowing the vessel lumen and elevating the formation of atherosclerotic plaque. The ongoing mobilization of leukocytes results in the immunodeficiency caused by lymphocytopenia, thus increasing the risk of infection, which complicates the stroke by increasing the activation of the immune system and its interaction with endothelial and neural cells.