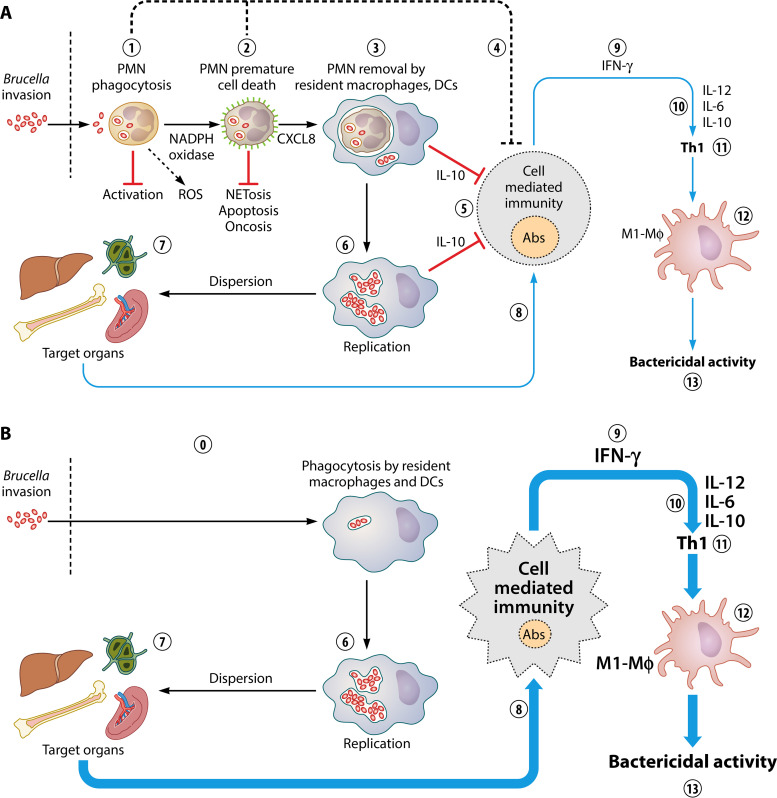
FIG 9.
The Trojan horse hypothesis and modulation of the Th1 response. (A) After the invasion of Brucella organisms, resident PMNs phagocytize the bacteria without inducing significant activation or degranulation (1) nor signs of necrosis, oncosis, or NETosis. Infected PMNs, however, release chemokine CXCL8 and expose phosphatidylserine on the cell surface as an “eat me” signal (in green) (2). Then, in the primarily affected organs, such as the liver, spleen, and BM, Mϕs and DCs phagocytize the Brucella-infected PMNs in a nonphlogistic manner (3). Infected PMNs may have a direct regulatory influence over cells of the adaptive immune response by an unknown mechanism that may involve lipoxins and other mediators (3). Those Mϕs colonized by Brucella-infected PMNs control adaptive immunity by releasing the regulatory cytokine IL-10 (5). This event allows bacterial replication inside mononuclear phagocytic cells such as Mϕs, Mo, and DCs (6), opening a window for bacterial dispersion in the target organs (7). Then, the adaptive immune response begins, with activation of the cell-mediated immunity and release of anti-Brucella antibodies (8), significant quantities of IFN-γ (9), and the subsequent release of IL-12, IL-6, and the regulatory IL-10 (10), promoting a regulated Th1 response (11). The Th1 immune response induces polarization toward M1-type Mϕs (12), which exert an effective bactericidal action, controlling the infection (13). (B) In the absence of PMNs, there is no such regulatory function over the immune system, allowing the direct interaction of Mϕs with the bacterium (0). The fast activation of Mϕs and other mononuclear cells narrows the window for the immune system to respond, favoring an exacerbation of Th1 cell-mediated immunity with very large amounts of IFN-γ, IL-12, and IL-6 cytokines, smaller amounts of antibodies, and increased polarization of bactericidal M1-type Mϕs. The large amounts of IL-10 control the cytokine storm and promote the fast resolution of inflammation. As a consequence of this enhanced activation, the number of bacteria in the target organs decreases, favoring fast resolution of the infection.