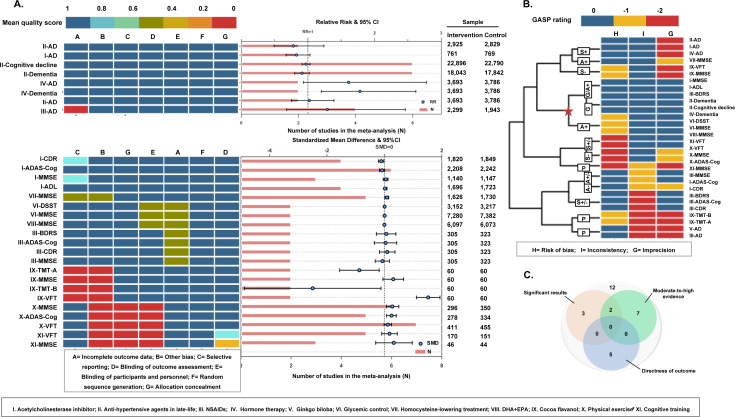
Figure 4.
Risk of bias profile, meta-analysis results, sample size (figure 4A), credibility rating (figure 4B) and summary (figure 4C) for 11 interventions based on randomised controlled trials. When the mean score (for each bias domain) ≤0.5 was regarded as possibly moderate-to-high risk, 17.2% meta-analyses had problems of inadequate concealment of allocations, 27.6% for performance bias, 3.4% for detection bias, 24.1% for incomplete outcome data, 13.8% for selective outcome reporting and 31% for other sources of bias. For the significance of the pooled results, six meta-analyses showed significant associations (figure 4A). For credibility of the pooled results, nine meta-analyses were rated at a moderate-to-high level (G, G/A+ or A+ level), three at a low-to-moderate level (A+/A− or A− level) and 17 at a very low level (S+, S− or P level). Specifically, moderate-to-high credibility of results showed little benefit on the risk of Alzheimer's disease from acetycholinesterase inhibitors, antihypertensive agents in late life, oestrogen therapy, and DHA+EPA supplementation. No robust conclusion could be reached for non-steroidal anti-inflammatory drugs, ginkgo biloba, cocoa flavanol and cognitive training. For directness of outcomes, five meta-analyses examined the associations with AD (figure 4B). Although none showed a good performance in all the above domains, two interventions (physical exercise and total homocysteine-lowering treatment) seem more promising than others (figure 4C).