Abstract
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has taken more than 1 million lives globally. This study, based on the official media releases of the Government of Nepal, analyses the clinical and epidemiological features of the individuals who died as a result of COVID-19 in Nepal from 23 January to 10 August 2020. We found that nearly half of the deaths were among people less than 50 years of age and being female increased the risk of death. The majority of deaths were associated with co-morbidities, the most common being cardiovascular diseases and diabetes followed by respiratory diseases. With the approaching festive season and relaxed lockdown, both government and citizens need to be more cautious about the severity of COVID-19 and take appropriate action.
Keywords: Comorbidity, coronavirus disease, COVID-19, demographics, epidemiology, mortality, Nepal, SARS-CoV-2, symptoms
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (named in the interim as 2019-nCoV) [1], and is of global concern because of its independent zoonotic transmission and rapid transmission rate. As of 1 November 2020, COVID-19 accounts for more than 45 million infections and more than 1 million deaths, and 20% of those infections are in South-East Asia [2]. The first case of COVID-19 infection appeared in China in December 2019 [3]. Nepal saw its first case on 23 January and from 24 March, Nepal implemented a national-level lockdown [4] that ended on 22 July with a few restrictions kept in place. Recently, after the easing of national-level lockdown, Nepal has seen a rapid increase in COVID-19 cases and deaths.
The proper management of a disease requires knowledge of its severity and mortality. The objective of this research is to analyse the clinical and demographic features of the individuals who died as the result of COVID-19 based on the official government reports. All data reported in this manuscript are current as of 10 August 2020.
Materials and methods
Data acquisition
After the appearance of the second case of COVID-19 in Nepal, the Ministry of Health and Population—Nepal started to give regular media briefings [5]. The Ministry has also been releasing situation reports almost every day since 28 January [6]. The media briefings and situation reports explained the major activities of the Government aimed at curbing the disease and the current status of infections, hospitalizations and deaths. By focusing on serious cases including deaths, the data for this research were obtained from those media briefings and situation reports.
Data analysis
Numbers of confirmed cases, confirmed deaths and province-wise deaths were obtained. The symptoms reported, demographics of the deaths including age, sex, co-morbidities and diagnosis time were analysed. When a specific parameter was not explicitly mentioned in the media briefings or situation report, the data were reported as ‘not sure’. The ages of three individuals who died were missing and were replaced with the mean data during analysis.
Results and discussion
Present scenario of COVID-19 infection in Nepal
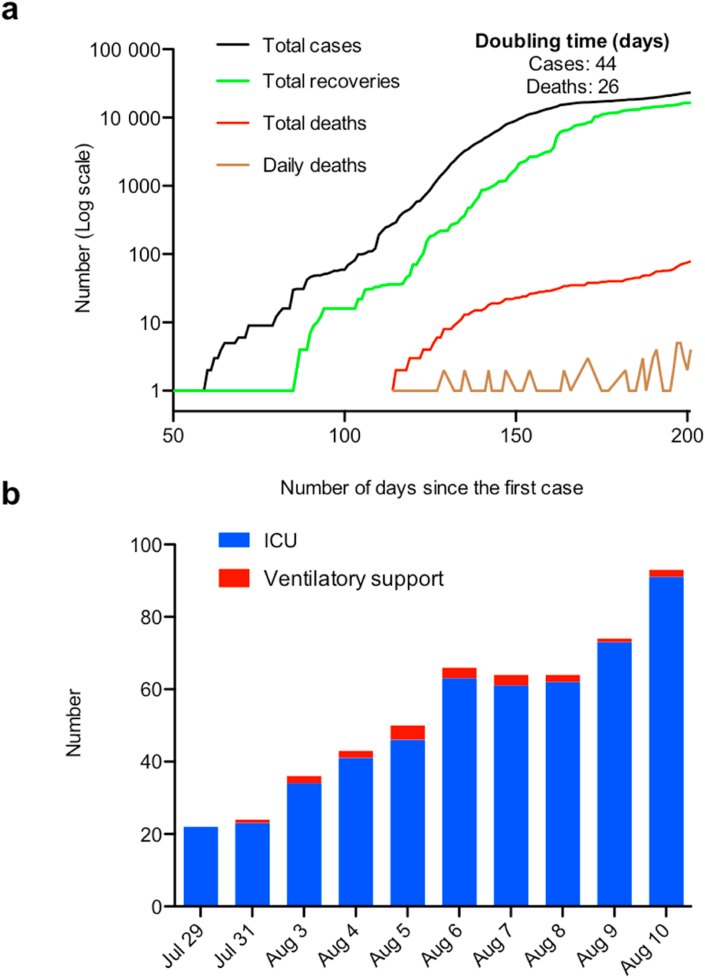
More than 6 months have passed since the detection of the first case on 23 January. Although, the Government of Nepal used both the rapid diagnostic test and real-time RT-PCR for testing SARS-CoV-2 in the early days of the pandemic, Nepal required all the suspected cases confirmed with real-time RT-PCR to be counted in the official numbers. So far, Nepal has performed 452 236 RT-PCR tests and seen a total of 23 310 confirmed cases and 79 deaths, including the death of a Chinese national attributed to COVID-19, with overall case fatality rate of 0.34%. Of the total cases, 16 493 (71%) have already recovered and, based on the data reported on 1 July (SitRep#143) by the Government, the early recovery rates among male and female patients were 27% and 17%, respectively [6]. Recent trends indicate that the number of deaths is increasing faster than the number of cases with the most recent doubling time for number of cases and deaths being 44 and 26 days, respectively (Fig. 1a). Since 29 July, the Ministry of Health and Population—Nepal has released information regarding the number of individuals that require admission to an intensive care unit and ventilatory support. The recent data show that the number of individuals requiring admission to an intensive care unit and ventilatory support is also in increasing trend (Fig. 1b).
Fig. 1.
Coronavirus disease 2019 (COVID-19) in Nepal. (a) Number of cases and deaths due to COVID-19 (the x-axis shows the number of days since the first reported case in Nepal (23 January) and y-axis shows the cumulative cases, recoveries and deaths, and daily deaths in log10 scale). (b) Number of cases requiring admission to intensive care unit (ICU) and ventilatory support from 29 July to 10 August. The data are extracted from refs [5,6]. The doubling time was calculated from the most recent data of 10 August by subtracting the day on which the events were half.
Analysis of infection and death by province
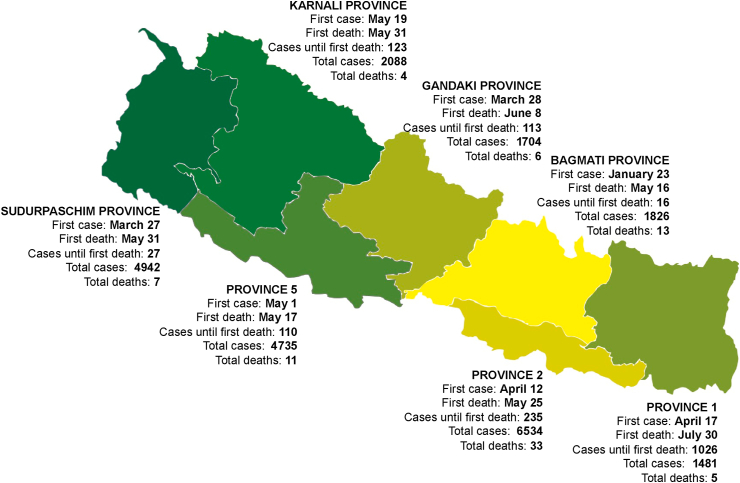
The maximum and minimum numbers of diagnosed cases were found in province 2 and province 1 with 6534 and 1481 cases, respectively. The maximum number of deaths was also seen in province 2, but the lowest number of deaths was observed in Karnali province. Although the total number of cases in Bagmati province was similar to that in Gandaki province, it had the highest case fatality rate (0.71%) (Fig. 2). Bagmati province includes the capital city Kathmandu, a medical hub for Nepal, and includes two of the four level 3 hospitals dedicated for COVID-19 treatment [7]. The higher case fatality rate in spite of health-care preparedness at Bagmati indicates that some severe cases might have been referred from other provinces.
Fig. 2.
Coronavirus disease 2019 situation in Nepal by province. Appearance of first case in the province, first death, number of cases diagnosed until first death with total cases and deaths are reported. Colours of provinces are shown from green to yellow based on the case fatality rate in an ascending order. The lowest (0.14%) and the highest (0.71%) case fatality rates were for Sudurpaschim and Bagmati provinces, respectively. The data are extracted from refs [5,6].
Demographic features of the COVID-19 deaths in Nepal
We found that the mean age of death was 50 years with a range of 0.13 years (49 days) to 85 years and the majority of them (72%) were male (Table 1). Although female patients accounted for only 24% of deaths, because the gender-wise distribution of infection among male and female patients was 5.25:1, the case fatality rate remained higher among female patients (0.51%) compared with male patients (0.29%), and this was consistent with the lower recovery rates among women. Our findings contrast with many reports that indicate being male is highly associated with death due to COVID-19 [8]. Men were at a higher risk of death due to COVID-19 in India [9], the USA [10], Brazil [11] and England [8]. The higher fatality rate among female patients in Nepal could be attributed to other concomitant risk factors such as smoking and non-communicable diseases. Smoking prevalence among women in Nepal is among the highest in South-East Asia [12] and 30% of the women in Nepal have at least one risk factor for non-communicable diseases [13].
Table 1.
Features of coronavirus disease 2019 (COVID-19) deaths in Nepal (n = 79)
| Variables | Frequency | % |
|---|---|---|
| Age (in years) | ||
| Mean ± SD | 49.7 ± 19.2 (range 0.13–85) | |
| <50 years | 39 | 49.4 |
| ≥50 years | 40 | 50.6 |
| Sex | ||
| Male | 57 | 72.1 |
| Female | 19 | 24.1 |
| Not reported | 3 | 3.8 |
| Symptoms present | ||
| Yes | 26 | 32.9 |
| No/Not sure | 53 | 67.1 |
| If yes, (n = 26) | ||
| Fever | 16 | 61.5 |
| Breathing difficulties | 22 | 84.6 |
| Cough | 7 | 26.9 |
| Chest pain | 1 | 3.8 |
| Co-morbidities | ||
| Yes | 48 | 60.7 |
| No/Not sure | 31 | 39.3 |
| If yes, (n = 48) | ||
| Tuberculosis | 5 | 10.4 |
| Renal diseases | 9 | 18.7 |
| Cardiovascular diseases | 15 | 31.2 |
| Diabetes | 15 | 31.2 |
| Respiratory diseases | 8 | 16.7 |
| Asthma, (n = 4) | ||
| Pneumonia, (n = 2) | ||
| Other respiratory problems, (n = 2) | ||
| Liver disease | 1 | 2.1 |
| Stroke and paralysis | 3 | 6.2 |
| Confirmed as COVID-19-positive | ||
| Before death | 27 | 34.2 |
| After death | 39 | 49.4 |
| Not sure | 13 | 16.4 |
| If before death, (n = 27) | ||
| Symptoms present | 11 | 40.7 |
| Symptoms absent | 16 | 59.3 |
| If after death/Not sure, (n = 52) | ||
| Symptoms present | 15 | 28.8 |
| Symptoms absent | 37 | 71.2 |
Nearly half of the deaths occurred in people <50 years of age (Table 1). There was nationwide disparity among the deaths attributed to COVID-19 with a difference between the developed and developing regions. In developed regions, elderly people account for a higher share of the population, and are at significantly higher risk of dying if they develop COVID-19. Countries like the USA [14] and Italy [15] have seen a larger proportion of elderly people, aged >80 years, accounting for the majority of deaths attributed to COVID-19; whereas most deaths occurred in patients aged from 50 to 70 years in countries like India [9], Bangladesh [16], Brazil [11] and Iran [17]. As the life expectancy at birth in Nepal is about 70 years [18], the results from our analysis of COVID-19 deaths in Nepal is particularly alarming.
Clinical features of the COVID-19 deaths in Nepal
We found that only 33% of the cases presented with definitive symptoms, where respiratory difficulties were the most frequently reported symptoms followed by fever (Table 1). The reported incidence of symptoms in Nepal was far lower than reported in China [19] and Italy [15], where at least 84% and 93% of the deaths, respectively, were in individuals with symptoms. In addition, 61% of the deaths were associated with co-morbidities where cardiovascular diseases and diabetes accounted for most co-morbidities (Table 1). Although, the incidence of co-morbidities among deaths was much lower than reported in China [20], South Korea [20], Italy [15] and Brazil [11], these data are similar to those reported from the USA [14]. Given the differences among national data, it is very important to consider the region-specific strategic plan in the management of COVID-19. The higher incidence of cardiovascular disease and diabetes among COVID-19 deaths in Nepal is, in fact, similar to those reported in the other studies [11,14,15,20]. Recent studies have shown the involvement of angiotensin-converting enzyme 2 (ACE2) and the serine protease TMPRSS2 in SARS-CoV-2 entry and binding [21,22], the expression of which have been found to be increased in diabetic patients [23]. Hence, diabetes increases the risk of death from COVID-19, although with proper management and controlled sugar levels, the outcomes after COVID-19 in individuals with diabetes can be improved [24].
We further found that more than half of the individuals who died were diagnosed as SARS-CoV-2-positive after death (Table 1). A study covering two states of India found that about 18% of the deaths were reported as being in linked to COVID-19 either ≤24 hours before death or posthumously [9]. In Nepal, when the SARS-CoV-2 infection was confirmed after death or the data were not available, 71% of the events were reported as without symptoms. We speculate that the posthumous detection of the cases in our setting could be responsible for this result. This might indicate differences in COVID-19 management systems and reporting status among countries. Although posthumous real-time RT-PCR testing facilitated contact tracing, even allowing the isolation/quarantine of people who participated in the funeral rituals in Nepal, this result suggests that a significant number of individuals who died were not diagnosed in time to allow proper management with supportive therapy.
Conclusions
In summary, more than half of the COVID-19 deaths were related to co-morbidity, and breathing difficulties were the most frequently reported symptoms. Although males were vulnerable to infection, we found that, if infected, women were at more risk for death. Interestingly, the majority of fatalities were not among elderly individuals, indicating that the younger population also needs to consider the severity of the disease. Although the Nepal government's management appeared to be effective at first, later—as the result of uncontrolled entry of returnees, lack of ability to conduct massive testing, poorly managed quarantines and lack of adherence to physical distancing measures among citizens—the number of cases and deaths did not decrease even with the strict measures in place [4]. In conclusion, with loosened lockdown, and the upcoming festive seasons, it might be difficult to control the spread of COVID-19. Nepal needs to be more prepared to detect, handle and treat more infections in the coming days before the health-care system becomes overwhelmed.
Conflict of interest
The authors declare no conflict of interest.
Contributor Information
A. Paudel, Email: atmikapd@gmail.com.
S. Panthee, Email: supanthee@gmail.com.
References
- 1.Coronaviridae Study Group of the International Committee on Taxonomy of Viruses The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . WHO; Geneva: 2020. COVID-19 weekly epidemiological update: data as received by WHO from national authorities, as of 1 November 2020, 10 am CEST. [Google Scholar]
- 3.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Panthee B., Dhungana S., Panthee N., Paudel A., Gyawali S., Panthee S. COVID-19: the current situation in Nepal. New Microb New Infect. 2020;37:100737. doi: 10.1016/j.nmni.2020.100737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Government of Nepal Ministry of Health and Population . 2020. Novel coronavirus (COVID-19) media briefing. [Google Scholar]
- 6.Government of Nepal Ministry of Health and Population . SitRep-1-183; 2020. Health sector response to COVID-19. [Google Scholar]
- 7.Government of Nepal Ministry of Health and Population, Health Sector Emergency Response Plan . 2020. COVID-19 pandemic. [Google Scholar]
- 8.Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laxminarayan R., Wahl B., Dudala S.R., Gopal K., Mohan C., Neelima S. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science. 2020 doi: 10.1126/science.abd7672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lewnard J.A., Liu V.X., Jackson M.L., Schmidt M.A., Jewell B.L., Flores J.P. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ. 2020;369:m1923. doi: 10.1136/bmj.m1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Souza W.M., Buss L.F., Candido D.D.S., Carrera J.P., Li S., Zarebski A.E. Epidemiological and clinical characteristics of the COVID-19 epidemic in Brazil. Nat Hum Behav. 2020;4:856–865. doi: 10.1038/s41562-020-0928-4. [DOI] [PubMed] [Google Scholar]
- 12.Government of Nepal . 2012. Brief profile on tobacco control in Nepal. [Google Scholar]
- 13.Bista B., Dhungana R.R., Chalise B., Pandey A.R. Prevalence and determinants of non-communicable diseases risk factors among reproductive aged women of Nepal: results from Nepal Demographic Health Survey 2016. PLoS One. 2020;15 doi: 10.1371/journal.pone.0218840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stokes E.K., Zambrano L.D., Anderson K.N., Marder E.P., Raz K.M., El Burai Felix S. Coronavirus disease 2019 case surveillance—United States, january 22–may 30, 2020. MMWR. 2020;69:759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.SARS-CoV-2 Surveillance Group . Istituto Superiore di Sanit; Italy: 2020. Characteristics of SARS-CoV-2 patients dying in Italy. Report based on available data on September 7th, 2020. [Google Scholar]
- 16.Dey S.K., Rahman M.M., Siddiqi U.R., Howlader A. Exploring epidemiological behavior of novel coronavirus (COVID-19) outbreak in Bangladesh. SN Compr Clin Med. 2020:1–9. doi: 10.1007/s42399-020-00477-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nikpouraghdam M., Jalali Farahani A., Alishiri G., Heydari S., Ebrahimnia M., Samadinia H. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in Iran: a single center study. J Clin Virol. 2020;127:104378. doi: 10.1016/j.jcv.2020.104378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.WHO . WHO; Geneva: August 10, 2020. Countries. Nepal. [Google Scholar]
- 19.Chen L., Yu J., He W., Yuan G., Dong F., Chen W. Risk factors for death in 1859 subjects with COVID-19. Leukemia. 2020;34:2173–2183. doi: 10.1038/s41375-020-0911-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qiu P., Zhou Y., Wang F., Wang H., Zhang M., Pan X. Clinical characteristics, laboratory outcome characteristics, comorbidities, and complications of related COVID-19 deceased: a systematic review and meta-analysis. Aging Clin Exp Res. 2020;32:1869–1878. doi: 10.1007/s40520-020-01664-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peters M.C., Sajuthi S., Deford P., Christenson S., Rios C.L., Montgomery M.T. COVID-19-related genes in sputum cells in asthma. Relationship to demographic features and corticosteroids. Am J Respir Crit Care Med. 2020;202:83–90. doi: 10.1164/rccm.202003-0821OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu L., She Z.G., Cheng X., Qin J.J., Zhang X.J., Cai J. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;31:1068–1077. doi: 10.1016/j.cmet.2020.04.021. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]