Abstract
Introduction
Diaphyseal tibial fractures distal to a well-fixed tibial component although rare present a significant challenge and optimal treatment remains controversial. Displaced periprosthetic tibial shaft fractures are ideally treated with open reduction internal fixation with plate osteosynthesis. However, this treatment method is associated with weight-bearing restrictions, which can be difficult for elderly patients with multiple comorbidities and balance impairment. We present our experience of internal fixation with an intramedullary nail that uses an inferior entry point, standard intramedullary tibial nail, and conventional instrumentation.
Materials and methods
Between 2017 and 2018, three patients with acute tibial shaft fractures distal to a TKA (Felix Type 3A) were treated with an intramedullary nail. Preoperative planning involved assessing proximal tibia to ensure adequate room for implant and instrumentation. The average patient age was 66.3 years (range 59–72 years) and all patients were males. All the patients sustained fractures of distal tibial and fibula diaphysis, after a road traffic accident. There were no complications intraoperatively, and all procedures were completed uneventfully. One patient underwent additional fixation of the fibula.
Results
All patients achieved a radiological fracture union after an average of 20.6 weeks. There were no fixation failures, or nonunions postoperatively. There were no new symptoms relative to the TKA that could be attributed to the tibial nailing procedure.
Conclusion
We recommend that this technique can be used primarily for this fracture pattern distal to a TKA, provided there is adequate space to accommodate the nail and instrumentation proximally anterior to the tibial tray.
Graphic abstract
Keywords: Total knee arthroplasty, Tibia fracture, Periprosthetic fracture, Intramedullary nailing
Introduction
Total knee arthroplasty (TKA) is currently one of the most common adult reconstructive procedures world over [1]. According to Frost and Sullivan’s research, the arthroplasty market in India was expected to grow at a compound annual growth rate of 26.7% during 2010–2017. According to this survey, almost 70,000 joint replacement surgeries were performed in India in the year 2011. With the rising geriatric population and increased utilization in younger patients, this number is expected to double within the next decade [2]. In contrast to periprosthetic supracondylar femur fractures after total knee arthroplasty (TKA), periprosthetic tibial fractures are rare. In a study of over 17,000 TKAs, the incidence of periprosthetic tibial fractures was reported to be 0.4% and the incidence of fracture distal to a stable, well-fixed tibial implant was 0.09% [3]. The incidence of periprosthetic tibia fractures is expected to increase with the rise in the total knee arthroplasty surgeries.
Diaphyseal tibial fractures distal to a well-fixed tibial component present a significant challenge and optimal treatment remains controversial. Fractures with a stable pattern and minimal displacement have been treated nonoperatively. Displaced tibial shaft fractures are ideally treated with open reduction internal fixation with plate osteosynthesis [4]. However, both treatment methods are associated with weight-bearing restrictions, which can be difficult for elderly patients with multiple comorbidities and balance impairment. Prolonged bed rest and immobilization may lead to complications such as loss of muscle strength and endurance, contractures and soft tissue changes, disuse osteoporosis, pressure ulcers, and degenerative joint disease. Cardiovascular complications include an increased heart rate, decreased cardiac reserve, orthostatic hypotension, and venous thromboembolism [5]. Intramedullary nails are often the first choice for fixation of lower limb diaphyseal fractures, as they provide superior biomechanical conditions and also maintain the length and rotation of the limb. However, in the case of periprosthetic tibial shaft fractures, intramedullary nailing is technically demanding due to the presence of tibial baseplate and cement mantle proximally.
To overcome these limitations, Haller et al. described a technique of intramedullary interlocking nailing of periprosthetic tibial shaft fractures distal to the well-fixed tibial tray. However, to navigate the posterior cortex, they have recommended that the distal end of the nail must be bent by utilizing a tabletop bender [6]. In this study, we describe our results using a standard expert intramedullary tibia nail (Expert Tibia Nail; Synthes, Oberdorf, Switzerland) for the surgical treatment of tibia fracture distal to well-fixed TKA prosthesis by this technique without modifying the nail and by using conventional instrumentation in three cases.
Preoperative Planning
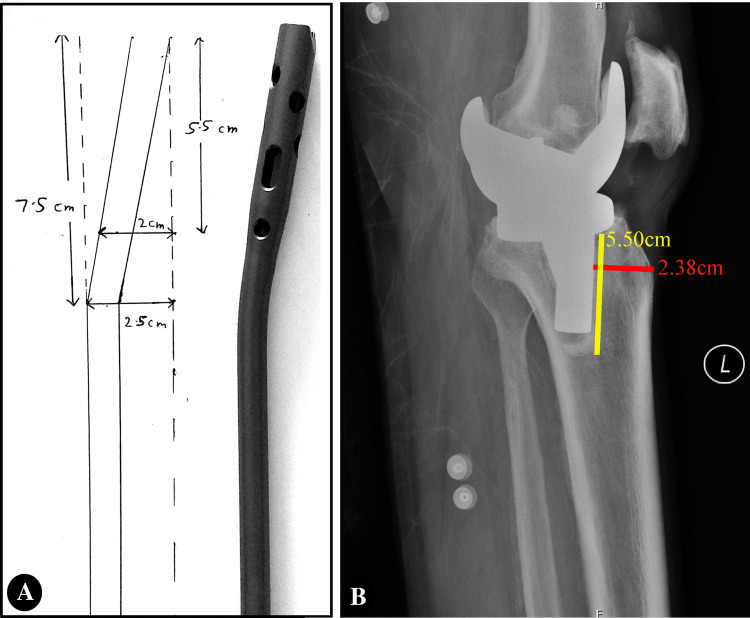
Preoperative lateral radiographs are evaluated to ensure adequate space is available anterior to the tibial tray and cement mantle to accommodate instrumentation and implant (Fig. 1). The maximum length of the stem of the tibial tray along with cement mantle is 5.5 cm in all our study patients. The actual diameter of the corresponding proximal broad part of the nail (8 mm–10 mm size nails) is 11 mm. To accommodate this portion of the nail along with Herzog’s bend without damaging the anterior tibial cortical margin and tibial tray stem with cement mantle posteriorly, a minimum safe distance of 4 mm on either side of the nail was chosen. So, we calculated that a space of 2 cm is required anterior to stem of tibial tray and cement mantle to ensure safe insertion of the instrumentation and intramedullary nail during the procedure. In standard expert intramedullary tibia nail (Expert Tibia Nail; Synthes, Oberdorf, Switzerland), the Herzog’s bend lies at 7.5 cm from the proximal tip of the nail. We have chosen only the interlock nail which fits into this model.
Fig. 1.
Preoperative evaluation of lateral radiograph to ensure adequate space anterior to the tibial tray
Surgical Technique
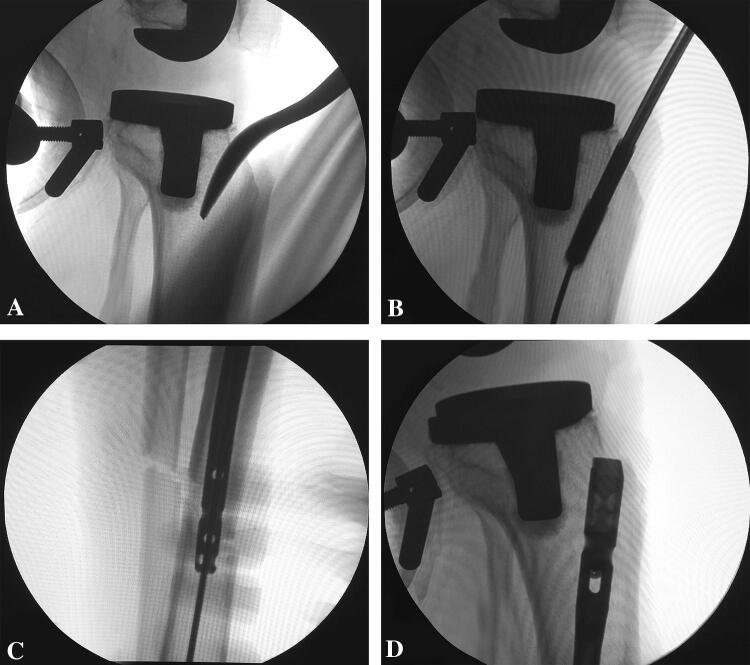
The patient is positioned supine on a fracture table under calcaneum pin traction. The contralateral lower extremity is well padded and secured to a lithotomy leg holder. The fluoroscopy unit is placed on the contralateral side, and the fluoroscopy monitor is positioned at the foot of the bed. The injured lower extremity is then prepped and draped in a usual sterile fashion. For identifying the starting point joint line and tibial tubercle are palpated and verified under fluoroscopy to ensure entry point distal to the tibial tray. A direct midline incision is made extending from the inferior pole of the patella up to the tibial tuberosity. The patellar tendon is sharply divided in line with the orientation of the fibers. An opening awl is then used to gain access to the medullary canal slightly more distal than in a traditional technique avoiding tibial tray under fluoroscopy guidance (Fig. 2a). A ball tip guidewire is passed across the fracture site under fluoroscopy guidance avoiding the tibial tray and correct placement is confirmed under fluoroscopy guidance. Hand reaming is done proximal to the fracture site and sequential power reaming is performed at the fracture site and in the distal tibia (Fig. 2b). After reaming achieves adequate cortical contact, a nail of appropriate small diameter (9 mm diameter) and length is selected. The appropriate sized nail is inserted and advanced under fluoroscopy to verify that the tip of the nail avoids the posterior cortex (Fig. 2c). The final position is verified with fluoroscopy on AP and lateral views (Fig. 2d). Proximal and distal interlocks are placed, and AP and lateral views are obtained with fluoroscopy. Surgical wounds are copiously irrigated and the fibers of the patellar tendon are re-approximated with 2-0 absorbable suture, and the dermis and skin are closed with 3-0 non-absorbable suture.
Fig. 2.
a Lateral C arm image demonstrating a slightly distal starting point. b Lateral C arm image demonstrating the position of power reamer well away from tibial tray. c Lateral C arm image demonstrating the position of the nail as it is maneuvred inside the medullary canal away from the posterior cortex. d Lateral C arm image demonstrating the final position of the proximal end of the intramedullary nail well anterior to the tibial tray
Clinical Experience
Between 2017 and 2018, three patients with acute tibial shaft fractures distal to a TKA were treated with an intramedullary nail in our institution. The average patient age was 66.3 years (range 59–72 years) and all patients were males. All the patients treated in this series sustained fractures of the distal tibial and fibula diaphysis, after a road traffic accident. Preoperative planning involved assessing proximal tibia to ensure adequate room for implant and instrumentation (Fig. 1). There were no complications intraoperatively, and all nailing procedures were completed uneventfully. One patient underwent additional fixation of the fibula. All patients achieved a radiological fracture union after an average of 20.6 weeks. There were no fixation failures, or nonunions postoperatively (Table 1). There were no new symptoms relative to the TKA that could be attributed to the tibia nailing procedure.
Table 1.
Patient characteristics
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age (years) | 72 | 68 | 59 |
| Sex | Male | Male | Male |
| Mechanism of injury | RTA | RTA | RTA |
| AO OTA classification | 42B2c | 42B2c | 42B2c |
| Duration of follow-up | 17 months | 13 months | 12 months |
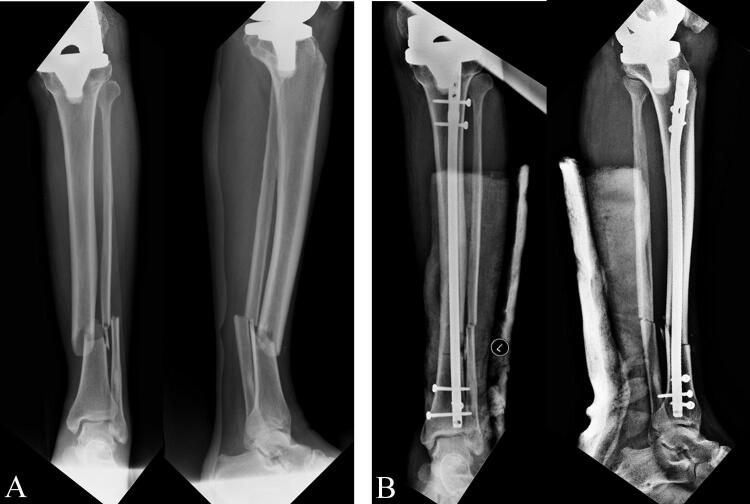
Case 1
A 72-year-old male presented with a Felix Type 3A periprosthetic fracture of the distal tibia and fibula diaphysis (AO OTA Type 42B2c) of the left leg following a road traffic accident. Radiographic imaging of his left knee showed a well-fixed tibial component in mild varus with no signs of loosening or failure (Fig. 3a). At the time of the presentation, the patient was diagnosed with cellulitis of the left leg. After he was medically cleared and recovered from cellulitis, the patient underwent open reduction and plating for fibula and intramedullary nailing for tibia by the above-described procedure. His postoperative hospital course was unremarkable, and the patient was discharged home on postoperative day 7. He was mobilized non-weight bearing with walker support for 6 weeks and subsequently progressed to weight bearing as tolerated. By the 16-week hospital visit, he had no pain at the fracture site and had returned to his baseline ambulation status. At 6-month post-surgery, radiographic imaging demonstrated the healing of 3 of 4 cortices of the tibia and all four cortices of the fibula (Fig. 3b). He continued to do well at the 17-month follow-up visit and had returned to his pre-injury ambulatory status.
Fig. 3.
a Anteroposterior and lateral radiographs of Left leg demonstrating fractures of tibial and fibular shafts distal to TKA prosthesis. b 6-month postoperative radiograph of leg demonstrating healing of three of four cortices of the tibia and all four cortices of the fibula
Case 2
A 68-year-old male presented after sustaining a Felix Type 3A periprosthetic fracture of the distal tibia and fibula diaphysis (AO OTA Type 42B2c) of the right leg in a road traffic accident. Radiographic imaging of his right knee showed a well-fixed tibial component with no signs of loosening or failure (Fig. 4a).
Fig. 4.
a Anteroposterior and lateral radiographs of right leg demonstrating fractures of tibial and fibular shafts distal to TKA prosthesis. b 4-month postoperative radiograph of leg demonstrating healing of three of four cortices of the tibia and all four cortices of the fibula
The patient underwent closed reduction and intramedullary nailing for tibia by the above-described procedure. His postoperative hospital course was unremarkable, and the patient was discharged home on postoperative day 5. He was mobilized non-weight bearing with walker support for 6 weeks and subsequently progressed to weight bearing as tolerated. By the 16-week hospital visit, he had no pain at the fracture site and had returned to his baseline ambulation status. Radiographic imaging demonstrated the healing of three of four cortices of the tibia and all four cortices of the fibula (Fig. 4b). He continued to do well at the 13-month follow-up visit and had returned to his pre-injury ambulatory status.
Case 3
A 59-year-old male presented after sustaining a Felix Type 3A periprosthetic fracture of the distal tibia and fibula diaphysis (AO OTA Type 42B2c) of the left leg. Radiographic imaging of his left knee showed a well-fixed tibial component with no signs of loosening or failure (Fig. 5a). The patient underwent closed reduction and intramedullary nailing for tibia by the above-described procedure (Fig. 5b). His postoperative hospital course was unremarkable, and the patient was discharged home on postoperative day 5. He was mobilized non-weight bearing with walker support for 6 weeks and subsequently progressed to weight bearing as tolerated. By the 20-week hospital visit, he had no pain at the fracture site and had returned to his baseline ambulation status. Radiographic imaging demonstrated the healing of all four cortices of the tibia and all four cortices of the fibula. He continued to do well at the 12-month follow-up visit and had returned to his pre-injury ambulatory status.
Fig. 5.
a Anteroposterior and lateral radiographs of the left leg demonstrating fractures of tibial and fibular shafts distal to the TKA prosthesis. b Immediate postoperative radiograph
Discussion
The prevalence of periprosthetic fractures will increase as the incidence and prevalence of TKA rises. Tibial shaft fractures distal to a stable TKA prosthesis represent an uncommon problem for orthopedic surgeons. The routine treatment options available include external fixation, plating, intramedullary nail, and nonoperative management each with their advantages and disadvantages. Some of these treatment modalities are better suited in patients with a TKA.
Nonoperative management usually consists of casting and/or bracing and prolonged non-weight bearing, which in elderly individuals may lead to limited mobility and related problems due to prolonged bed rest and immobilization like loss of muscle strength and endurance, contractures and soft tissue changes, disuse osteoporosis, pressure ulcers, and degenerative joint disease [5].
External fixation is usually not employed as definitive treatment because of the inherent risks of pin tract infections, poor bone fixation, pin loosening, and a higher incidence of malunion and nonunion in osteopenic patients [7].
Open reduction with plate fixation remains a reasonable option for treating a distal diaphyseal tibial fracture in this scenario. Plates have been shown to have less incidence of malunion or nonunion when compared with nails when treating these injuries, but it is less reliable in osteoporotic patients. Locking plates have been designed to overcome this limitation. However, plate fixation requires restricted weight bearing until the union is achieved, which is difficult in the geriatric age group who usually suffer from osteopenia and poor balance [8, 9]. Also, these are associated with more soft tissue stripping which can be problematic in elderly individuals with poor soft tissue due to diabetes mellitus, peripheral vascular disease, etc.
Intramedullary nail has the advantage of early weight bearing, as it is a load-sharing device and there is preservation of soft tissues around the fracture site. Modern tibial nail designs allow for multiple interlock screws to be placed in the distal fragment to provide better rotational control [10]. These advantages make intramedullary nailing an attractive option in these fractures despite being technically demanding. Other authors have suggested the use of an intramedullary implant placed through a different starting point. Doulens et al. placed a standard intramedullary nail in a retrograde fashion using the medial malleolus as the starting point. They reported an iatrogenic fracture that was subsequently fixed [11]. Zafra-Jimenez et al. reported the use of a retrograde hindfoot nail to treat a distal diaphyseal tibia fracture below a TKA with good results [12]. But this procedure mandates implant removal after fracture union because of the restricted ankle and subtalar motion that can lead to early-onset degeneration of the subtalar joint and has the additional possibility of the potential stress raiser created between the tip of the nail and the TKA implant. Greco et al. described a case report of intragrade nailing of an open tibial shaft fracture. They used the open wound at the fracture site to place a small diameter retrograde femoral nail and an intramedullary reduction tool passed through a proximal window was utilized to impact the nail into the distal segment [13]. However, this technique cannot be used in all periprosthetic fractures, as these are usually low-energy closed injuries. The technique described by Haller et al. allows the insertion of an intramedullary nail through a standard approach. However, to navigate the posterior cortex, they recommend that the distal end of the nail must be bent by utilizing a tabletop bender [6]. This can be difficult to do without experience and can alter the biomechanical properties of the device. Woyski et al. described their technique of suprapatellar nailing of these fractures [14]. Their technique requires specialized instruments and has an inherent theoretical risk of damage to the femoral component and dislodgement of the patellar button.
The technique we describe enables anterograde nailing of these distal tibia and fibula fractures by conventional instrumentation. We recommend that this technique can be used primarily for this fracture pattern distal to a TKA, provided there is adequate space to accommodate the nail and instrumentation proximally anterior to the tibial tray. However anterior and slightly inferior starting point would make treatment of more proximal fractures more difficult.
The limitations of our study include small sample size, single-center study, difficulty in insertion of the nail in patients with well-aligned tibial component, and limited space between anterior tibial cortical margin and stem of the tibial tray.
Conclusion
In our experience, the above technique is a viable alternative for the treatment of these currently rare, but difficult to treat fractures. Tibial component design and position, fracture pattern, and patient characteristics must be considered while deciding the treatment options.
Compliance with Ethical Standards
Conflict of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Ethical standard statement
Ethical committee approval was obtained for this study.
Informed consent
All the three patients were informed about the possibility of sending their anonymised details for publication and consent was obtained.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kurtz, S.M., Lau, E., Ong, K., Zhao, K., Kelly, M., & Bozic, K.J. (2009). Future young patient demand for primary and revision joint replacement: National projections from 2010 to 2030. In Clinical Orthopaedics and Related Research, vol. 467 (pp. 2606–2612). New York: Springer. 10.1007/s11999-009-0834-6 [DOI] [PMC free article] [PubMed]
- 2.Frost and Sullivan. (2011). Overview of Orthopedic Joint Replacement Market in India [Internet]. https://store.frost.com/overview-of-orthopedic-joint-replacement-market-in-india.html. Accessed 5 Mar 2020.
- 3.Felix, N.A., Stuart, M.J., & Hanssen, A.D. (1997). Periprosthetic fractures of the tibia associated with total knee arthroplasty. In Clinical Orthopaedics and Related Research, vol. 345 (pp. 113–124). New York: Springer. [PubMed]
- 4.Hanssen, A.D., & Stuart, M.J. (2000). Treatment of periprosthetic tibial fractures. In Clinical Orthopaedics and Related Research, vol. 380 (pp. 97–98). Lippincott Williams and Wilkins. [DOI] [PubMed]
- 5.Douglas KD, Robert T. Complications of Immobilization and Part 1: Musculoskeletal and cardiovascular complications. Canadian Family Physician. 1993;39(1):1428–1437. [PMC free article] [PubMed] [Google Scholar]
- 6.Haller JM, Kubiak EN, Spiguel A, Gardner MJ, Horwitz DS. Intramedullary nailing of tibial shaft fractures distal to total knee arthroplasty. Journal of Orthopaedic Trauma. 2014;28(12):e296–300. doi: 10.1097/BOT.0000000000000096. [DOI] [PubMed] [Google Scholar]
- 7.Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. Journal of the American Academy of Orthopaedic Surgeons. 2006;14:406–416. doi: 10.5435/00124635-200607000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. Journal of Orthopaedic Trauma. 2011;25(12):736–741. doi: 10.1097/BOT.0b013e318213f709. [DOI] [PubMed] [Google Scholar]
- 9.Mao Z, Wang G, Zhang L, Zhang L, Chen S, Du H, et al. Intramedullary nailing versus plating for distal tibia fractures without articular involvement: A meta-analysis. Journal of Orthopaedic Surgery and Research. 2015;10(1):95. doi: 10.1186/s13018-015-0217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vallier HA. Current evidence: Plate versus Intramedullary nail for fixation of distal tibia fractures in 2016. Journal of Orthopaedic Trauma. 2016;30(11):S2–6. doi: 10.1097/BOT.0000000000000692. [DOI] [PubMed] [Google Scholar]
- 11.Doulens KM, Joshi AB, Wagner RA. Tibial fracture after total knee arthroplasty treated with retrograde intramedullary fixation. The American Journal of Orthopedics (Belle Mead NJ) 2007;36(7):E111–E113. [PubMed] [Google Scholar]
- 12.Zafra-Jiménez JA, Pretell-Mazzini J, Resines-Erasun C. Distal tibial fracture below a total knee arthroplasty: Retrograde intramedullary nailing as an alternative method of treatment: A case report. Journal of Orthopaedic Trauma. 2011;25(7):e74–e76. doi: 10.1097/BOT.0b013e3181f9aa68. [DOI] [PubMed] [Google Scholar]
- 13.Greco N, Goyal K, Tarkin I. Intragrade intramedullary nailing of an open tibial shaft fracture in a patient with concomitant ipsilateral total knee arthroplasty. The American Journal of Orthopedics (Belle Mead NJ). 2015;44(3):E81–E86. [PubMed] [Google Scholar]
- 14.Woyski D, Emerson J. Suprapatellar nailing of Tibial shaft fractures in total knee arthroplasty. Journal of Orthopaedic Trauma. 2016;30(12):e409–e413. doi: 10.1097/BOT.0000000000000656. [DOI] [PubMed] [Google Scholar]