Abstract
Purpose
With the current COVID-19 outbreak, otolaryngologists are most exposed to the risk of infection due to the nature of the specialty.This is why they are required to find safer diagnostic alternatives minimizing aerosol-generating procedures. The aim of this study is to explore the accuracy of transcutaneous laryngeal ultrasonography (TLUSG) in order to assess vocal fold movement.
Materials and methods
We performed blindly both TLUSG and flexible fiberoptic laryngoscopy(FFL) on 38 patients, from March to June 2020. Patients were divided into two groups:the former with normally mobile vocal folds and the latter with unilateral vocal fold paralysis.
Results
On FFL findings, 10/38 patients (26,31%) had unilateral vocal fold paralysis; on TLUSG results, 9/38 patients (23.68%) presented impaired vocal fold motion. In comparison to laryngoscopy, the sensitivity, specificity, positive predictive value and negative predictive value of TLUSG for assessment of vocal fold mobility was 80%, 96.42%, 88.88%, 93.10% respectively. A significant association between the two techniques was found on the Chi-square test: X2 = 19.7722 (p value <0.00001). Cohen's K value showed a substantial agreement: K = 0,79.
Conclusion
Although TLUSG could undoubtedly not replace laringoscopy, it represents a noninvasive and useful diagnostic tool for otolaryngologists especially during covid-19 pandemic.Data collected about its high sensitivity and specificity suggest that TLUSG could be a reliable method to screen vocal fold paralysis without performing aerosol-generating procedures, thus providing clear visualization of laryngeal real-time movements, even in non-compliant or high-risk infection patients. Our results allow us to consider TLUSG as part of the preoperative assessment of vocal folds in patients undergoing thyroidectomy.
Keywords: Transcutaneous laryngeal ultrasonography, TLUSG, COVID-19, Flexible fiberoptic laryngoscopy, Vocal fold paralysis, Otolaryngology
1. Introduction
Coronavirus disease 2019 (COVID-19) is an infectious respiratory disease caused by the novel virus SARS-CoV-2. The World Health Organization declared COVID-19 a global pandemic.
Due to the lack of adequate devices for individual protection during the early stages of the pandemic, many health care workers contracted the infection.
According to the data of Italian National Health Agency, 30,009 health care workers resulted positive for SARS-CoV-2 as of September 24, 2020 [1].
Otolaryngologists are by the nature of their work at high risk for aerosol transmission. They inevitably carry out aerosol-generating procedures, starting from a simple routine examination of the oral cavity up to a fiberoptic laryngoscopy [2].
Appropriate and safer alternative diagnostic and therapeutic strategies can prevent infection among otolaryngologists and their staff [3,4].
During COVID 19 pandemic, we propose the use of transcutaneous laryngeal ultrasonography (TLUSG), as a rapid, noninvasive and risk-free investigative tool. Ultrasound can be used to evaluate vocal fold motion as a first diagnostic step; it is useful to rule out a vocal folds paralysis, in order to conduct an assessment before thyroidectomy or to secure airways and feeding. We don't consider ultrasound as an alternative to the practice of flexible fiberoptic laryngoscopy (FFL); actually we propose laryngoscopy as a second-level examination in order to obtain a correct diagnostic conclusion.
The aim of this study is to explore the accuracy of TLUSG in evaluating vocal fold function, thus providing to otorhinolaryngologists a safe diagnostic technique during COVID-19 pandemic, especially in the preoperative assessment of vocal folds in patients undergoing thyroidectomy.
2. Materials and methods
A total of 38 patients were examined by ENT specialists from March to June 2020s, by means of transcutaneous laryngeal ultrasonography as well as flexible fiberoptic laryngoscopy. Written informed consent was taken from each patient and data were collected in accordance to Helsinki declaration and comparable ethical standards.
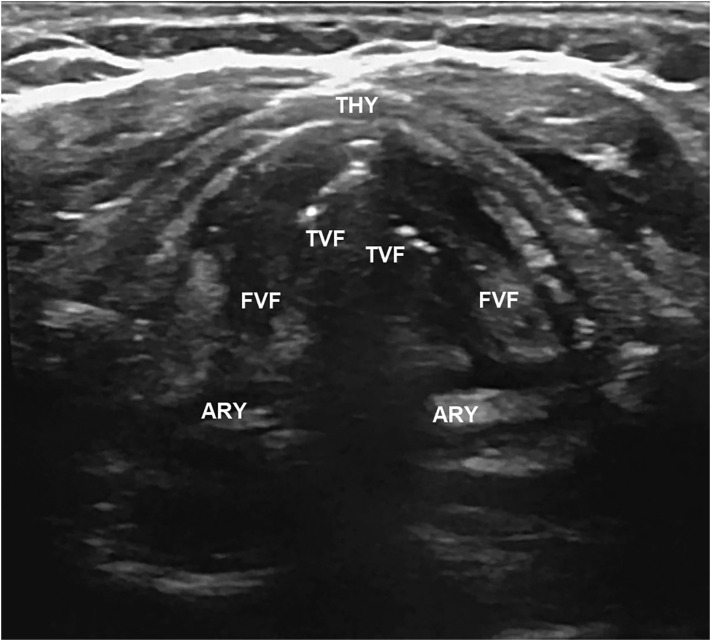
TLUSG was performed during quiet spontaneous breathing, in apnea and in phonation through a 10-MHz linear probe (GE LOGIQ E9). False vocal folds, true vocal fold and arytenoids were designated as laryngeal landmarks for a correct motion visualization (Fig. 1 ). FFL was performed blindly on the same day by a different operator.
Fig. 1.
Sonographic view of normal vocal folds during quiet respiration (abduction); FVF: false vocal fold, TVF: true vocal fold, ARY: arytenoid, THY: thyroid cartilage.
Patients were stratified into two groups according to FFL results: the former with mobile vocal folds (Group N) and the latter with unilateral vocal fold paralysis (Group P). Ultrasound findings were classified as normal or impaired vocal fold motion.
GraphPad Prism® software was used to perform statistical analysis. The evaluation of the accuracy and feasibility of TLUGS for assessing vocal folds mobility was carried out by calculating sensitivity, specificity, positive and negative predictive values. The association between TLUSG and FFL in detecting vocal fold mobility was assessed by using Chi Square with Yates' correction. Cohen's K value was calculated in order to evaluate the concordance between the two techniques. Statistical significance was defined as p < 0.05 with a confidence interval at 95%.
3. Results
Demographic profile and diagnostic features of all patients is depicted in Table 1 .
Table 1.
Demographic profile and diagnostic features.
| Overall (n = 38) |
Group N Normally mobile vocal folds (n = 28) |
Group P Unilateral vocal fold paralysis (n = 10) |
||
|---|---|---|---|---|
|
Age Mean (SD), years |
64.21 (13.88) |
61.14 (13.75) |
72.8 (10.65) |
|
|
Sex Male/female |
23/15 |
15/13 |
8/2 |
|
|
Diagnosis distribution n (%) |
|
5 (50%) 4 (40%) 1 (10%) |
||
Findings from FFL show that 28 patients (73.68%) had bilaterally mobile vocal cords, while 10 patients (26.31%) had unilateral vocal fold paralysis or hypomobility, (including 4 subjects affected by laryngeal cancer).
On TLUSG, bilaterally mobile vocal cords were found in 29 patients (76,31%) while abnormalities in vocal fold motility was detected in 9 patients (23.68%) (Table 2 ).
Table 2.
Comparison of TLUSG with FFL for vocal fold motion assessment (TLUSG: transcutaneous laryngeal ultrasonography; FFL: flexible fiberoptic laryngoscopy).
| TLUSG | FFL |
Total | |
|---|---|---|---|
| Unilateral vocal fold paralysis (Group P) |
Normally mobile vocal folds (Group N) |
||
| Impaired vocal fold motion | 8 | 1 | 9 |
| Normal vocal fold motion | 2 | 27 | 29 |
| Total | 10 | 28 | 38 (grand total) |
In comparison to FFL findings, the sensitivity of TLUSG for assessment of vocal fold mobility was 80%, the specificity was 96.42%, the positive predictive value was 88.88% and the negative predictive value was 93.10%.
Therefore, the Chi-square statistic with Yates correction showed a statistically significant association between the two techniques, with X 2 (1, N = 38) = 19.7722, with p value <0.00001 (significant at p < 0.05).
The concordance between the two techniques and the relative Cohen's K value was calculated, showing a substantial agreement: K = 0,79 (95%: confidence interval). The number of observed agreements was 35 (92.11% of the observations); the number of agreements expected by chance was 23.7 (62.47% of the observations).
Adequate visualization during ultrasound examination was affected by the shape and calcification of the thyroid cartilage, typically in elderly and male patients: due to the prominent protrusion and diffuse calcification of the thyroid cartilage, the operator had to use a lateral or longitudinal approach, in a different acoustic window. In our experience, all the cases of hard visualization due to the calcification of the thyroid cartilage (4/38 patients: 10.52%) were males with a mean age of 74.25.
4. Discussion
Transcutaneous Laryngeal Ultrasonography has been described extensively in the literature, as a non-invasive and painless indirect examination of vocal cords function [5]. It permits a good analysis of the dynamic aspect of the larynx while being inexpensive, rapid, repeatable and well tolerated by the patient.
During the exam, the patient is positioned supine with the neck slightly extended. The US transducer is placed transversely, in the midline, over the middle portion of the thyroid cartilage, by angling the transducer slightly superiorly. The most commonly described sonographic landmarks [6] are the following:
-
-
arytenoids (ARY),
-
-
true vocal folds (TVF),
-
-
false vocal folds (FVF).
On the transverse view, the thyroid cartilage has an inverted V shape, within which the true and false vocal cords are detectable. The true vocal folds are composed of muscle, so they appear hypoechoic, not always well distinguishable, whereas the false vocal folds are composed of echoic fat, they indeed appear hyperechoic; arytenoids cartilages are seen as paired hyperechoic structures underneath the TVF and FVF [7].
Movement is assessed during quiet respiration, observing the normal abduction of the folds during inspiration. If the patient is asked to temporarily stop breathing, the operator can appreciate the adduction of the vocal folds on the midline. Vocal fold mobility can be also evaluated during phonation: the diagnostic criterion for a vocal fold paralysis is the asymmetric abduction and adduction movements of the vocal folds [5]. If the vocal folds are not visible from a midline approach due to acute shape or calcification of the thyroid cartilage, each vocal fold can be assessed laterally to the cartilage [8].
According to several authors TLUSG represents an alternative tool to laryngoscopy to evaluate preoperative recurrent laryngeal nerve function in patients with thyroid disease [9,10].
In comparison with fiberoptic laryngoscopy, the sensitivity of laryngeal ultrasound in vocal fold motion evaluation is reported close to 90% [11] and concordance with laryngoscopy findings may exceed 95% [5].
Shah et al. [12] reported excellent values in terms of sensitivity, specificity, positive predictive value, and negative predictive value of TLUSG in the assessment of vocal cords if compared with videolaryngoscopy (75%, 95.1%, 60%, and 97.5% respectively) The author suggests the TLUSG in patients undergoing thyroidectomy, as a non-invasive, bedside screening tool for assessing vocal cord palsy postoperatively. Data reported in this work seem to be perfectly in line with our results.
However, some studies have highlighted that Laryngeal Ultrasonography should not be considered as an alternative to the practice of video laryngoscopy [13]. As shown in a recent study [14], the sensitivity and specificity of TLUSG for vocal fold motility assessment are significantly decreased in patients with a BMI of 25 or greater and after surgery. In addition, the rate of successful visualization of vocal cord movement by ultrasonography, according to Wong et al. [15], is lower than that achieved by laryngoscopy; some factors, as older age and male sex, can make the examination un-assessable. A low rate of visualization in men compared with women (17% vs 83%) and in patients with vs without thyroid cartilage calcification (42% vs 83%) is reported also in a multicentric study on 510 patients [16].
In spite of the limits of laryngeal ultrasound, we support this technique as a screening method for detecting vocal fold motion abnormalities, especially in a pandemic context in order to avoid contagion of health workers.
Our experience during COVID-19 era let us consider TLUSG as an aerosol-generating free procedure, useful for otorhinolaryngologists in particular in the preoperative evaluation of laryngeal function in patients addressed to thyroidectomy, as recommended by other authors [17]. We recommend subsequent laryngoscopy in all dysphonic patients and other cases of suspected vocal cords paralysis [18].
Ultrasound examination is safe performed, following standard and transmission-based precautions like proper use of protective equipment (face-masks, goggles, face protective shield, surgical gown and gloves) and transducer cleaning and disinfection [19].
Further experience with the TLUSG examination can pave the way for new prospects of laryngeal ultrasound use in ENT Departments like the ultrasound-guided identification of the cricothyroid membrane in the management of cricothyrotomy [20,21], the assessment of laryngeal pathologies in children including dysphonia and stridor [22] or a diagnostic complement to laryngoscopy and tomography in patients with laryngeal cancer [23,24].
As a future perspective, such a wide use of laryngeal ultrasonography would need an analysis on a larger group of patients in order to standardize the technique and increase the operator expertise in TLUSG procedure.
5. Conclusions
Otolaryngologists are currently required to find airway management strategies to reduce infectious risk and to adopt safer diagnostic alternatives minimizing aerosol-generating procedures, in order to protect themselves and others [25]. Because of this requirement, we propose the transcutaneous laryngeal ultrasonography as a new and evolving imaging technique in the assessment of vocal fold function. Our experience shows a significant concordance between TLUSG and FFL in detecting laryngeal function, encouraging us to consider laryngeal ultrasonography a promising method to screen for vocal cord paralysis.
In conclusion, although TLUSG can't replace laryngoscopy, it's a reproducible, noninvasive, comfortable diagnostic tool, with high sensitivity and specificity. It provides a clear visualization of laryngeal real-time movements, also in non-compliant or high-risk infection patients. Our results allow us to consider TLUSG as part of the preoperative routine in patients pending surgical intervention of thyroidectomy.
We expect that in a future perspective TLUGS will play a role also in the management of infantile disphonia, in ultrasound-guided airway procedures and in the evaluation of laryngopharyngeal cancers.
CRediT authorship contribution statement
Sciancalepore Pasqua Irene: Conceptualization, Methodology, Writing- Original draft preparation, Investigation, Formal analysis;
Anzivino Roberta: Validation, Data curation, Writing- Reviewing and Editing, Investigation;
Petrone Paolo: Supervision, Project administration, Investigation;
Petrone Domenico: Supervision, Resources;
Quaranta Nicola: Supervision.
Funding
None.
Declaration of competing interest
None.
References
- 1.https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard
- 2.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS ONE. 2012;7(4) doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chun-hui L., Xun H., Meng C. Expert consensus on personal protection in different regional posts of medical institutions during novel coronavirus pneumonia (COVID-19) epidemic period. Chin J Infect Control. 2020;19(3):1–15. [Google Scholar]
- 4.Chan J.Y.K., Wong E.W.Y., Lam W. Practical aspects of otolaryngologic clinical services during the 2019 novel coronavirus epidemic. JAMA Otolaryngol Head Neck Surg. 2020;348:1967–1976. doi: 10.1001/jamaoto.2020.0488. [DOI] [PubMed] [Google Scholar]
- 5.Gambardella C., Offi C., Romano R.M. Transcutaneous laryngeal ultrasonography: a reliable, non-invasive and inexpensive preoperative method in the evaluation of vocal cords motility-a prospective multicentric analysis on a large series and a literature review. Updates Surg. 2020 doi: 10.1007/s13304-020-00728-3. [DOI] [PubMed] [Google Scholar]
- 6.Wong K.P., Woo J.W., Youn Y.K., Chow F.C., Lee K.E. Lang BH (2014) The importance of sonographic landmarks by transcutaneous laryngeal ultrasonography in post-thyroidectomy vocal cord assessment. Surgery. 2014;156(6):1590–1596. doi: 10.1016/j.surg.2014.08.061. [DOI] [PubMed] [Google Scholar]
- 7.Loveday E.J. Ultrasound of the larynx. Imaging. 2003;15:109–114. [Google Scholar]
- 8.Woo J.W., Suh H., Song R.Y., Lee J.H., Yu H.W., Kim S.J. A novel lateral-approach laryngeal ultrasonography for vocal cord evaluation. Surgery. 2016;159(1):52–56. doi: 10.1016/j.surg.2015.07.043. [DOI] [PubMed] [Google Scholar]
- 9.Wang C.P., Chen T.C., Yang T.L., Chen C.N., Lin C.F., Lou P.J. Transcutaneous ultrasound for evaluation of vocal fold movement in patients with thyroid disease. Eur J Radiol. 2012;81(3):e288–e291. doi: 10.1016/j.ejrad.2011.09.020. [DOI] [PubMed] [Google Scholar]
- 10.Cheng S.P., Lee J.J., Liu T.P., Lee K.S., Liu C.L. Preoperative ultrasonography assessment of vocal cord movement during thyroid and parathyroid surgery. World J Surg. 2012;36(10):2509–2515. doi: 10.1007/s00268-012-1674-1. [DOI] [PubMed] [Google Scholar]
- 11.Wong K.P., Au K.P., Lam S., Lang B.H. Lessons learned after 1000 cases of transcutaneous laryngeal ultrasound (TLUSG) with laryngoscopic validation: is there a role of TLUSG in patients indicated for laryngoscopic examination before thyroidectomy? Thyroid. 2017;27(1):88–94. doi: 10.1089/thy.2016.0407. [DOI] [PubMed] [Google Scholar]
- 12.Shah M.K., Ghai B., Bhatia N., Verma R.K., Panda N.K. Comparison of transcutaneous laryngeal ultrasound with video laryngoscope for assessing the vocal cord mobility in patients undergoing thyroid surgery. AurisNasus Larynx. 2019;46(4):593–598. doi: 10.1016/j.anl.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 13.Sidhu S., Stanton R., Shahidi S., Chu J., Chew S., Campbell P. Initial experience of vocal cord evaluation using grey-scale, real-time, B-mode ultrasound. ANZ J Surg. 2001;71(12):737–739. doi: 10.1046/j.1445-1433.2001.02257.x. [DOI] [PubMed] [Google Scholar]
- 14.Kandil E., Deniwar A., Noureldine S.I. Assessment of vocal fold function using transcutaneous laryngeal ultrasonography and flexible laryngoscopy. JAMA Otolaryngol Head Neck Surg. 2016;142(1):74–78. doi: 10.1001/jamaoto.2015.2795. [DOI] [PubMed] [Google Scholar]
- 15.Wong K.P., Lang B.H., Chang Y.K., Wong K.C., Chow F.C. Assessing the validity of transcutaneous laryngeal ultrasonography (TLUSG) after thyroidectomy: what factors matter? Ann Surg Oncol. 2015;22(6):1774–1780. doi: 10.1245/s10434-014-4162-z. [DOI] [PubMed] [Google Scholar]
- 16.Carneiro-Pla D., Miller B.S., Wilhelm S.M. (2014) Feasibility of surgeon-performed transcutaneous vocal cord ultrasonography in identifying vocal cord mobility: a multi-institutional experience. Surgery. 2014;156(6):1597–1604. doi: 10.1016/j.surg.2014.08.071. [DOI] [PubMed] [Google Scholar]
- 17.Noel J.E., Orloff L.A., Sung K. Laryngeal evaluation during the COVID-19 pandemic: transcervical laryngeal ultrasonography. Otolaryngol Head Neck Surg. 2020 doi: 10.1177/0194599820922984. [DOI] [PubMed] [Google Scholar]
- 18.Amis R.J., Gupta D., Dowdall J.R., Srirajakalindini A., Folbe A. Ultrasound assessment of vocal fold paresis: a correlation case series with flexible fiberoptic laryngoscopy and adding the third dimension (3-D) to vocal fold mobility assessment. Middle East JAnaesthesiol. 2012;21(4):493–498. [PubMed] [Google Scholar]
- 19.World Federation for Ultrasound in Medicine and Biology Safety Committee (Jacques S. Abramowicz, Iwaki Akiyama, David Evans, J. Brian Fowlkes, KarelMarsal, YusefSayeed and Gail terHaar), Abramowicz J.S., Basseal J.M. World federation for ultrasound in medicine and biology position statement: how to perform a safe ultrasound examination and clean equipment in the context of COVID-19. Ultrasound Med Biol. 2020;2020 doi: 10.1016/j.ultrasmedbio.2020.03.033. (S0301-5629(20)30149-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kristensen M.S. (2011) Ultrasonography in the management of the airway. ActaAnaesthesiol Scand. 2011;55(10):1155–1173. doi: 10.1111/j.1399-6576.2011.02518.x. [DOI] [PubMed] [Google Scholar]
- 21.Siddiqui N., Arzola C., Friedman Z., Guerina L., You-Ten K.E. Ultrasound improves cricothyrotomy success in cadavers with poorly defined neck anatomy: a randomized control trial. Anesthesiology. 2015;123(5):1033–1041. doi: 10.1097/ALN.0000000000000848. [DOI] [PubMed] [Google Scholar]
- 22.Shirley F., Oshri W., Ari D., Gad F. The role of laryngeal ultrasound in the assessment of pediatric dysphonia and stridor. Int J PediatrOtorhinolaryngol. 2019;122:175–179. doi: 10.1016/j.ijporl.2019.04.017. [DOI] [PubMed] [Google Scholar]
- 23.Rzepakowska A., Osuch-Wójcikiewicz E., Bruzgielewicz A., Niemczyk K. (2015) How useful is ultrasound in the assessment of local advancement of laryngeal cancer? Otolaryngol Pol. 2015;69(2):21–26. doi: 10.5604/00306657.1149637. [DOI] [PubMed] [Google Scholar]
- 24.Dhoot N.M., Choudhury B., Kataki A.C., Kakoti L., Ahmed S., Sharma J. Effectiveness of ultrasonography and computed tomography in assessing thyroid cartilage invasion in laryngeal and hypopharyngeal cancers. J Ultrasound. 2017;20(3):205–211. doi: 10.1007/s40477-017-0259-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Balakrishnan K., Schechtman S., Hogikyan N.D., Teoh A.Y.B., McGrath B., Brenner M.J. COVID-19 pandemic: what every otolaryngologist-head and neck surgeon needs to know for safe airway management. Otolaryngol Head Neck Surg. 2020;162(6):804–808. doi: 10.1177/0194599820919751. [DOI] [PubMed] [Google Scholar]