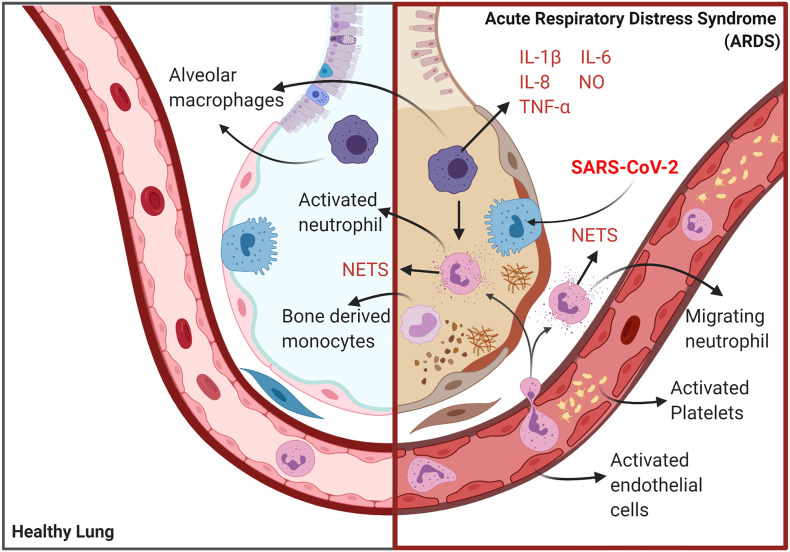
Fig. 1.
The pathophysiology of COVID-19 ARDS. Initial infection and activation of type 2 alveolar cells and alveolar macrophages by SARS-CoV-2 results in the secretion of IL-6, PICs, NO and several chemokines which activate vascular endothelial cells platelets and neutrophils ultimately forming a platelet neutrophil complex. The interplay between vascular endothelial cells activated platelets and activated primed neutrophils produces a highly coagulative and inflammatory state described as immunothrombosis. The translocation of neutrophils and platelets into the pulmonary microvasculature results in severe epithelial layer damage alveolar fibrin deposition and the formation of microthrombi. The translocation of NET producing neutrophils into alveoli and lung interstitium coupled with their delayed apoptosis results in the development cytokine storm producing extreme tissue damage and often fatal lung dysfunction created by several feedforward loops involving interplay between PICS DAMPS ROS, activation of the NLRP3 inflammasome activation, alveolar macrophage pyroptosis, influx of inflammatory bone derived monocytes and necroptosis.