Abstract
Background
The objective of this study was to investigate medication adherence and the associated influencing factors in patients with chronic obstructive pulmonary disease (COPD) who were treated in a primary general hospital in Shanghai China during the 2019 novel coronavirus (COVID-19) pandemic.
Methods
From March to April 2020, all of the COPD patients treated in our department in the last 7 years were interviewed by telephone. The basic patient data and each questionnaire item were collected, and influencing factors were analyzed by the Chi-square test, U test, and univariate and multivariate logistic regression analyses.
Results
A total of 191 patients with COPD were queried, and 84 (44.0%) valid questionnaires were obtained. Among them, individuals with group B symptoms were most represented (45.2%); 53.6% had Medical Research Council (MRC) dyspnea levels of 2 or above. Chronic obstructive pulmonary disease assessment test (CAT) had an average of 9 [3, 13], and 52.4% of patients used two-drug combination therapy. Medication adherence was both good in ordinary times and over the past 2 months of the pandemic, and 88.8% of patients had no acute exacerbation during the pandemic. The CAT scores of male patients <70 years old, and patients with general outpatient follow-up and regular gargling were reduced (P<0.05). Drug combination and doctor’s supervision were favorable factors affecting medication adherence during the 2 months of the pandemic, while possible depression was an unfavorable factor (P<0.05).
Conclusions
During the pandemic, medication adherence in patients with COPD was similar to that in regular times, and was significantly related to drug combination, doctor’s supervision, and accompanying mood disorders. An effective way to improve patient adherence and disease control could be strengthening follow-up education and diagnosing and treating depression and other complications.
Keywords: Chronic obstructive pulmonary disease (COPD), medication, adherence, COVID-19
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic respiratory disease characterized by continuous airflow limitation which seriously endangers human health. According to survey results from 2012 to 2015 in China, the prevalence of COPD in individuals over 20 years was 8.6%, and that of people over 40 years was 13.7% (1).
In the current outbreak of the 2019 novel coronavirus disease (COVID-19), patients with chronic pulmonary diseases such as COPD have a poor prognosis and a high mortality rate (2). Therefore, standardized and efficient management of COPD is particularly important. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommends inhaled therapy (bronchodilator or inhaled glucocorticoids) as the first choice for stable patients (3). The standard treatment in the stable period of COPD is very important for the tertiary prevention of the disease.
Our department investigated discharged COPD patients in 2016, and the adherence of inhaled medication was only 46.2% (4). For patients with poor adherence, measures such as outpatient education and pharmacist intervention were strengthened in the later stage. Due to the pandemic situation, during the time period spanning from late January to April 2020, it was recommended that travelling and unnecessary medical treatments be reduced, which might have hindered maintenance treatment of COPD. Therefore, the present study was conducted to assess the treatment status, medication adherence, and the associated influencing factors in patients with COPD during the COVID-19 pandemic. The findings will hopefully provide clinicians with a basis for further intervention measures.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-6016).
Methods
Study design
The present cross-sectional study was performed in Ruijin Hospital North, Shanghai, China. The contact information of all COPD patients discharged from our department between January 2012 and January 2019 or followed up in our outpatient department between March 2020 and April 2020 were collected. Patients were interviewed by telephone and included if they had a sufficient level of understanding and communication ability. The patient themselves or family members provided telephone contact information and volunteered to participate in the investigation. Diagnosis of COPD was performed according to the GOLD spirometry definition (2). Exclusion criteria were the following: other uncontrolled systemic complications, cognitive impairment, inability to communicate correctly, or poor compliance with the investigation.
The included patients underwent a telephone follow-up survey by trained investigators. The follow-up survey questionnaire for COPD was developed and reviewed for revisions, and included questions on basic information, treatment data, symptoms, possible negative emotions (screened by the Self Rating Anxiety Scale (SAS) and Self Rating Depression Scale (SDS) for telephone survey), and preventive measures during the COVID-19 pandemic. Patients were rated based on GOLD guidelines (3), symptom scores by the Medical Research Council (MRC) dyspnea scale, and the chronic obstructive pulmonary disease assessment test (CAT). Patients with an MRC level ≥2 or CAT score ≥10 (high value) were assigned to the highly symptomatic group (groups B and D), while the remaining patients were assigned to the slightly symptomatic group (groups A and C). For risk, patients with ≥2 acute exacerbations within 1 year or >1 hospitalizations were assigned to the high-risk group (groups C and D), while the remaining patients were assigned to the low-risk group (groups A and B).
Data collection
Basic information
Demographic data were assessed, including age, gender, nationality, occupation, and education background. Clinical information was recorded, including disease course, history of exacerbations, smoking history, symptoms, follow-up form, drug use, inhalation time, medication adherence, possible combination of adverse mood behaviors, and measures for epidemic prevention.
Medication adherence
The prescriptions and drug information of outpatients were assessed, and phone calls were made to check the dosage and frequency of drug use. Adherence was determined by the following formula: dose compliance (%) = number of days with right dose in 30 days/30 × 100%; dose compliance >80% indicated good adherence, with other values being considered poor adherence (5).
Possible combination of mood disorders
Telephone calls were made for follow-up at various times, and sensitive topics such as suicidal tendencies were avoided. Several representative questions were selected from the SAS and SDS in order to increase compliance through use as a standard for determining the presence of any mood disorders. SAS was scored as follows: (I) feeling nervous and more anxious than usual; (II) easily upset or fearful; (III) easily feeling weak and tired). SDS was scored as follows: (I) feeling depressed; (II) often experiencing poor sleep; (III) waking up during sleep.
Ethics
The study was conducted in adherence to the guidelines of the Declaration of Helsinki (as revised in 2013). This study design was approved by the Ethics Committee of Ruijin Hospital (Shanghai, China). Because the medical records and other information were obtained from previous clinical practice, and investigation did not adversely affect the rights and health of the subjects, patients were exempt from informed consent.
Statistical analysis
Data are presented as mean ± standard deviation (SD), median [interquartile range (IQR)], or percentage. The outcome of interest was medication adherence over the past 2 months (during COVID-19 pandemic times). Differences between patients with and without good adherence were assessed by the Chi-square test for categorical variables. Then, a two-step correlation analysis was conducted. Firstly, univariate regression analysis was carried out to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for determining the associations of covariates with outcomes. In the second step, a multivariate regression model was used to estimate the odds ratios and 95% confidence intervals for the associations of covariates with outcomes adjusted for variables with statistical significance in univariate analysis. A P value <0.05 was considered statistically significant.
Results
Patient characteristics
A total of 191 patients with COPD were enrolled, of whom 22 were excluded due to death. Therefore, 169 were contacted by telephone; 32 did not answer, 30 did not cooperate with the investigation, and 23 were unable to accurately respond to the questionnaire. Finally, 84 valid questionnaires were obtained from March to April 2020.
Among the respondents, 85.7% were male, 98.8% were of Han ethnicity, and 67.9% had a junior high school education or below. The participants were aged 48 to 90 years (averaging 72.2±9.8 years), and 76.2% had a history of smoking. Among these individuals, 45.2% had group B symptoms, 53.6% had MRC levels ≥2, and CAT scores averaged 9 [3, 13] points. Maintenance treatment included inhalation alone [long-acting anticholinergic agents (LAMA), long-acting β2 agonists (LABA), or inhaled corticosteroids (ICS) with long-acting β2 agonists (ICS + LABA)]; combined inhalation preparations (LAMA + ICS + LABA); and inhalation products combined with oral medication (e.g., acetylcysteine, theophylline).
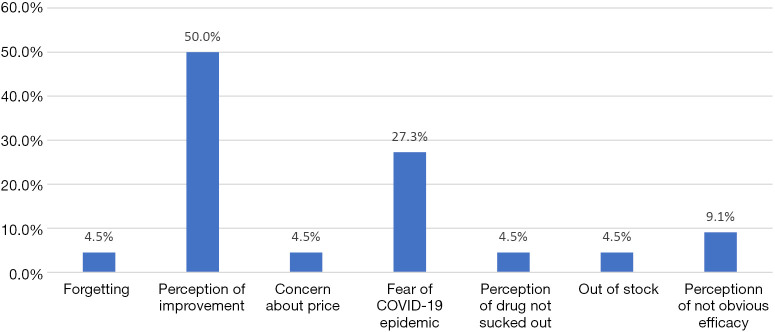
In regular times and over the past 2 months of the pandemic period, the patients with good medication adherence accounted for 75% and 73.8% of the total cases, respectively. Reasons for poor compliance (Figure 1) mostly included perception of improvement; other reasons were forgetting medication or dispensers, perception of ineffective absorption, and concern about the high cost. A total of 27.3% of patients over the past 2 months did not return to the hospital for prescription for fear of the COVID-19 pandemic; 85.7% chose to visit the hospital with a worsened condition, including 55.6% that selected the original treatment hospital.
Figure 1.
Cause distribution of poor compliance over the past 2 months of the COVID-19 pandemic (n=22).
Patients with possible anxiety and depression accounted for 20.2% and 31% of cases, respectively. The former group presented most commonly with the symptoms of self-conscious fatigue and emotional tension, while the latter had sleep disturbance.
Correlation analysis of symptoms, treatment compliance, and acute exacerbation over the past 2 months of the COVID-19 pandemic
The U test showed that the CAT scores of male patients <70 years old, who followed up in the general outpatient department, and gargled regularly were lower (P<0.05) and had milder symptoms over the past 2 months of pandemic compared with regular times. The exacerbation rate in the low-risk group was also lower over the past 2 months (χ2=18.188, P<0.01).
Over the past 2 months, patient compliance in the low-exacerbation risk group was better than that of the high-risk group (χ2=5.697, P=0.035). The compliance of combination users was better (χ2=4.163, P=0.041). The patients whose inhalation times were ≥45 months had better compliance (χ2=3.941, P=0.047). The patients who accepted continuous doctor supervision had better compliance (χ2=6.301, P=0.012). Patients with possible depression had poor compliance (χ2=5.060, P=0.024). There were no significant differences in compliance for other factors over the past 2 months of pandemic compared with regular times (Table 1).
Table 1. Baseline patient characteristics according to medication adherence over the past 2 months of the COVID-19 pandemic.
| Variable | Total patients, n=84 (%) | Good adherence, n=62 (%) | Poor adherence, n=22 (%) | P value* |
|---|---|---|---|---|
| Male | 72 (85.7) | 54 (75.0) | 18 (25.0) | 0.504 |
| Han ethnicity | 83 (98.8) | 61 (73.5) | 22 (26.5) | 1.000 |
| ≥70 years old | 48 (57.1) | 35 (72.9) | 13 (27.1) | 0.830 |
| Course ≥10 years | 42 (50.0) | 33 (78.6) | 9 (21.4) | 0.321 |
| Retired/unemployed | 58 (69.0) | 42 (67.7) | 16 (72.7) | 0.664 |
| Junior high school or above | 27 (32.1) | 17 (63.0) | 10 (37.0) | 0.120 |
| Combined medication | 60 (71.4) | 48 (80.0) | 12 (20.0) | 0.041 |
| Inhalation ≥45 months | 42 (50.0) | 35 (83.3) | 7 (16.7) | 0.047 |
| No exacerbation in 2019 | 65 (77.4) | 52 (80.0) | 13 (20.0) | 0.035 |
| General outpatient follow-up | 59 (70.2) | 47 (79.7) | 12 (20.3) | 0.061 |
| Continuous doctor supervision | 53 (63.1) | 44 (83.0) | 9 (17.0) | 0.012 |
| History of smoking | 64 (76.2) | 48 (75.0) | 16 (25.0) | 0.657 |
| Stabilization evaluation | ||||
| Group A | 27 (32.1) | 21 (33.9) | 6 (27.3) | 0.056 |
| Group B | 38 (45.2) | 31 (50.0) | 7 (31.8) | |
| Group C | 5 (6.0) | 4 (6.5) | 1 (4.5) | |
| Group D | 14 (16.7) | 6 (9.7) | 8 (36.4) | |
| Symptoms | ||||
| Less symptomatic | 32 (38.1) | 25 (78.1) | 7 (21.9) | 0.480 |
| More symptomatic | 52 (61.9) | 37 (71.2) | 15 (28.8) | |
| Exacerbation risk group | ||||
| Low risk | 65 (77.4) | 52 (80.0) | 13 (20.0) | 0.035 |
| High risk | 19 (22.6) | 10 (52.6) | 9 (47.4) | |
| Possible depression | 26 (31.0) | 15 (57.7) | 11 (42.3) | 0.024 |
| Possible anxiety | 17 (22.2) | 10 (58.8) | 7 (41.2) | 0.132 |
*, P value obtained by the Chi-square test comparing good and poor adherence groups over the past 2 months. P<0.05 indicates statistical significance.
Univariate logistic regression analysis revealed that adherence over the past 2 months was significantly associated with medication, doctor’s supervision, exacerbation risk, a history of exacerbation in 2019, and possible depression (P<0.05, Table 2). Multivariate logistic regression analysis revealed drug combination and doctor’s supervision were favorable factors affecting adherence over the past 2 months, while possible depression was an unfavorable factor (P<0.05, Table 2).
Table 2. Univariate and multivariate regression analyses of poor medication adherence over the past 2 months of the COVID-19 pandemic.
| Variable | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | ||
| Age | 0.897 | 0.334–2.408 | 0.830 | – | – | NS | |
| Sex | 0.667 | 0.179–2.479 | 0.545 | – | – | NS | |
| Combined medication | 0.350 | 0.125–0.979 | 0.046 | 0.258 | 0.079–0.842 | 0.025 | |
| Inhalation <45 months | 2.778 | 0.994–7.766 | 0.051 | – | – | NS | |
| No continuous doctor supervision | 3.531 | 1.284–9.708 | 0.015 | 5.390 | 1.671–17.381 | 0.005 | |
| Low risk | 0.278 | 0.094–0.823 | 0.021 | – | – | NS | |
| Exacerbation in 2019 | 3.600 | 1.215–10.669 | 0.021 | – | – | NS | |
| Possible depression | 3.133 | 1.132–8.672 | 0.028 | 3.691 | 1.187–11.480 | 0.024 | |
OR, odds ratio; CI, confidence interval; NS, no significant difference.
Discussion
COPD is a common chronic airway disease, which mainly occurs in individuals over 40 years old. It is characterized by chronic cough and phlegm, and shortness of breath after physical activity, and is easily exacerbated in the winter and spring. Prolonged progression of symptoms, irreversible damage to lung function, and gradual onset of cardiovascular complications all lead to decreased quality of life and increased disability and mortality. The 2019 novel coronavirus, which has been prevalent since November 2019, has caused infections and even severe pneumonia and death in various provinces and cities across China. On January 30, 2020, the World Health Organization (WHO) declared COVID-19 to be a public health emergency of international concern. On February 11, 2020, the WHO termed the associated disease “coronavirus disease 2019” (COVID-19) (6). COVID-19’s epidemiological data in China show an average age of 48.9 years for hospitalized patients with confirmed disease (2), with a high fatality rate of 5.1%, and a fatality rate in ≥80 year-old individuals as high as 14.8% (7). After adjustments for age and smoking status are rendered, COPD (HR =2.671, 95% CI: 1.424–5.048), diabetes, high blood pressure, and malignant tumors become risk factors for the composite end point (2). Before the pandemic is over, it is essential to monitor the disease and ensure the effective management of patients with COPD as a focus population.
In this study, the average age of patients with stable COPD was 72.2±9.8 years, and 76.2% had a history of smoking, which is consistent with the epidemiological characteristics of the Chinese population (1). Group B (45.2%) was the most represented, and individuals with MRC levels of 2 or above accounted for 53.6% of patients; CAT scores ranged from 0 to 26, with an average score of 9 [3, 13]. The acute exacerbation rates were 22.6% and 6% in 2019 and over the past 2 months, respectively, which reflects the clinical characteristics of “more symptoms, lower risk”. It was found that nocturnal dyspnea in patients with COPD was associated with future exacerbation of the disease (HR =2.3; 95% CI: 1.7–3.0), affecting admission rate (HR =3.2; 95% CI: 2.3–4.4) and mortality (HR =1.7; 95% CI: 1.2–2.3); in addition, significant early morning/daytime symptoms at baseline also predicted acute exacerbation in the following 6 months (P<0.01) (8). Therefore, more attention should be paid to the current stable follow-up population.
This survey showed that patients ≥70 years of age, of male gender, with history of exacerbation over the past 2 months, no continuous doctor supervision, community follow-up, and irregular gargle, had more symptoms (high CAT scores, P<0.05). This may be explained by the fact that as lung function in aged patients declines further, males often encounter occupational risk factors or smoke, repeated and recent exacerbations increase airway inflammation and airflow limitation, and lack of knowledge about standard treatment concepts reduces patient acceptance, medication adherence, and disease management (9). Meanwhile, irregular gargles can easily lead to oropharyngeal complications with the inhaled drugs, such as hormonal disturbance, causing irregular medication use (interruption or withdrawal), acute exacerbation of upper respiratory tract infection, and reduce disease control. In clinical practice, attention should be paid to such individuals, through monitoring the patient condition, encouraging outpatient follow-up, promoting the reduction of risk factors, and regulating the use of drugs and mouthwash. It should also be noted that patients who are elderly, involved in community follow-up, and use mouthwash irregularly may have low education, low income, and are women, or are living alone; disease risk reduction in these patients should not be ignored (10,11).
COPD is a chronic airway inflammatory disease characterized by incomplete reversible airflow limitation. Past exacerbation can further damage the airway structure and function, accelerate disease progression, and increase the risk of repeated exacerbation. In this study, the exacerbation rate over the past 2 months among the high-risk patients was still higher (P<0.05), suggesting that attention should be paid to the condition of the high-risk population in screening, which may include controlling exacerbating factors such as smoking, dust inhalation, and recurrent respiratory infections; timely correction (smoking cessation, and community flu virus and pneumococcal vaccines, etc.); urging drug therapy; and preventing further adverse events as much as possible.
Treatment adherence in patients with COPD is an important component in the whole process of disease management. Indeed, poor adherence may lead to more symptoms, decreased lung function (12), repeated acute exacerbations, increased mortality, and decreased quality of life (13).
In this study, maintenance treatment in COPD patients included inhaled drugs alone (LAMA, LABA, or ICS + LABA), combined inhaled preparations (LAMA + ICS + LABA), and inhaled preparations combined with oral medications (such as acetylcysteine and theophylline), which met the recommendations of the GOLD guidelines (3). Medication adherence in patients with COPD ranges from 30.3% to 81.2% in the early stage (13-16), and decreases with time within 6 months (16). In 2016, our department investigated 39 patients with COPD discharged from the hospital, among whom 46.2% had good adherence with inhaled medication; part of the poor adherence was related to non-active drug education and intervention after discharge (4). In the following 4 years, through the construction of a special outpatient follow-up, regular publicity and educational strategies with the participation of pharmacists, and taking advantage of the characteristics of the newly built third-level hospital in the suburbs (patients mainly originate from the local resident population), our department has promoted the doctor–patient connection and co-treatment, and has striven to improve the management of COPD. In this expanded study population, the adherence of patients with COPD during discharge and outpatient follow-up was significantly improved over the past 2 months, reaching 73.8%. The reasons for poor adherence included lack of voluntary improvement, forgetting, and drug withdrawal, corroborating previous reports (17,18). Perception of improvement or lack of drug efficacy is related to the patient’s lack of education concerning disease, while drug failure is related to insufficient inhaler technology. A total of 27.3% of patients in this study were worried about the COVID-19 pandemic, which led to treatment reduction or discontinuation. This requires clinical specialists strengthen the daily supervision in particular, including providing information about the disease outbreak and drug effects, clarifying the medical technology, performing supervision and follow-up, answering questions, and removing unnecessary concerns; in patients with drug cost issues, treatment should use effective drugs with suitable cost, which can improve compliance; existing monitor technology should be improved in patients with non-compliance for suction equipment (19-21).
Evidence shows that treatment adherence in patients with COPD has significantly negative correlations with current smoking status (17), FEV1% (13,17), and age differences (22,23), but is not significantly correlated with gender and disease course (22,23). In this study, no assessment of current lung function was performed in the form of telephone interviews, and the statistical results did not indicate any associations of adherence over the past 2 months with smoking, age, or gender. Due to differing criteria for the definition of exacerbation (e.g., elevated or low frequency according to GOLD guidelines, or whether the average number of all-cause emergency visits/hospitalizations per month is greater than or equal to 1) and the time of the adherence survey, discrepant findings have been reported for the association of exacerbation risk with adherence (14,24). Univariate logistic regression analysis in this study showed that low risk had a favorable influence on medication adherence over the past 2 months (P<0.05), which is in accordance with Albrecht et al.’s findings (24). This may be related to reduced emergency medical treatment/hospitalization, a higher level of patience, self-confidence, and adherence to the management strategy in such individuals. However, multivariate regression analysis showed no significant difference, which might have been a result of the small sample size of this study. A future study by our group will expand the sample size to confirm the present findings.
In this study, drug combination was a favorable factor affecting treatment adherence in over the past 2 months (P<0.05). Patients with combined drugs usually have many symptoms, poor lung function or high risk of exacerbation, frequent medical visits, and more opportunities to receive treatment and education, and are more likely to pay attention to the prognoses of their conditions and to attach more importance to the drug treatment plan formulated by doctors, improving adherence. It has been reported that adherence to inhalation medication in patients with COPD is negatively correlated with FEV1% (13,17), which also partly reflects the effect of combination therapy on adherence.
The above multifactor regression analysis suggested a correlation between doctor supervision and compliance over the past 2 months (P<0.05), again emphasizing the usefulness of active medical intervention and good doctor–patient communication for improved disease management and efficacy. Cognitive impairment may affect the inhalation technique and adherence. To improve treatment adherence, clinicians, pharmacists, and nurses should educate COPD patients about the disease, drug effects, and inhalation techniques, and supervise medication use (18,22,25-28). It was reported that 3 consecutive months of follow-up supervision of inhaled drugs (the 7-step method) significantly and gradually improves the disease control rate, subjective symptoms, and the quality of life in patients with COPD (26). The integration strategy of joint participation is more conducive to the optimal management in the stable period (29).
With the promotion of the three-level diagnosis and treatment system, the gradual decline of common chronic diseases in the grassroots level in China, and the availability of primary treatment hospitals and large comprehensive/specialized hospitals, community medical staff have also contributed to the follow-up and supervision of COPD patients. Indeed, relevant research has evinced the value of the guidance provided by health care personnel and community pharmacists (18,23,25,28).
Patients with COPD are prone to depression and anxiety (30), with an incidence of depression between 5.5% and 51.5% (31), which is related to factors such as the long course of disease, decreased activity and poor health status (32), long-term oxygen therapy (33), and increased burden to health and personal finances. Depression may have a negative impact on treatment maintenance due to the decreased expectation of disease outcome or complex treatment regimens (24), resulting in reduced adherence (16) and an increased risk of acute exacerbation requiring hospitalization (31,34). Application of antidepressant drugs and the treatment of complications could affect the individual’s adherence and prognosis (24,35).
During the COVID-19 pandemic, there may be aggravation of an already negative emotional state, which might affect medication adherence and treatment efficacy in the stabilization period, and/or induce or aggravate the original somatic symptoms. This survey showed that COPD with possible depression represented 31% of all cases, and possible depression was an independent risk factor for poor treatment adherence over the past 2 months, which is consistent with Albrecht, et al.’s results (16). This reveals the importance of managing these individuals to ensure stable treatment and reduce the risk of acute exacerbation through monitoring and intervention of adverse emotions.
Some limitations in this study should be addressed. First, due to the limited manpower and time, face-to-face investigation could not be guaranteed, and patients often had concerns about frequent visits to the hospital during the epidemic, so we adopted a telephone follow-up method for this study; although these interviews were conducted by trained staff, and doctors’ orders and prescriptions were also coordinated, there might still have been uncertainty in the answers received. Secondly, considering the tentativeness of the patients interviewed to participate by telephone (due the total length of time and the sensitivity of the topics), anxiety and depression were investigated without formally or completely determining the SAS, SDS, and only a few representative subjects were selected. The statistical results of the survey need to thus be further verified. Thirdly, due to the small sample size and limited follow-up time, more cases are required for statistical analysis in the future, in order to identify more accurate and reliable influencing factors. Finally, although our department has reported similar medication adherence in the past, it was not with the same group of patients as the group in this study; the former sample was small (<50), and thus a head-to-head comparison with the results of this study is not strictly feasible.
Conclusions
Overall, having multiple symptoms has remained an obvious feature of patients with stable COPD during the COVID-19 pandemic; other characteristics include good medication adherence and a reduced recent exacerbation rate. Fear of COVID-19 has affected hospital prescriptions and continuous treatment. Age, exacerbation history, negative emotional states, and other factors could affect symptom scores, recent adherence, and recent acute exacerbation. Clinicians should strengthen patient supervision and monitoring; encourage integrated medical teams including pharmacists, nurses and psychologists; and improve disease management. Further studies are required to confirm these findings.
Supplementary
The article’s supplementary files as
Acknowledgments
We would like to thank Dr. Dong Liu for her excellent statistical contribution and Guangzhou Yujia Biotechnology Co., Ltd for their help to this study.
Funding: This work was supported by the Youth Foundation of Shanghai Municipal Commission of Health and Family Planning (No. 20174Y0184).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in adherence to the guidelines of the Declaration of Helsinki (as revised in 2013). This study design was approved by the Ethics Committee of Ruijin Hospital (Shanghai, China). Because the medical records and other information were obtained from previous clinical practice, and investigation did not adversely affect the rights and health of the subjects, patients were exempt from informed consent.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-6016
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-6016
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-6016). The authors have no conflicts of interest to declare.
(English Language Editor: J. Gray)
References
- 1.Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet 2018;391:1706-17. 10.1016/S0140-6736(18)30841-9 [DOI] [PubMed] [Google Scholar]
- 2.Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. Eur Respir J 2020;55:2000547. 10.1183/13993003.00547-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mirza S, Clay RD, Koslow MA, et al. COPD Guidelines: A Review of the 2018 GOLD Report. Mayo Clin Proc 2018;93:1488-502. 10.1016/j.mayocp.2018.05.026 [DOI] [PubMed] [Google Scholar]
- 4.Lin Jia-Yuan, Le He Bin Xu, et al. Investigation on adherence to inhaled medication among patients with chronic obstructive pulmonary disease. Journal of Clinical Pulmonary Medicine 2017;22:658-661. [Google Scholar]
- 5.López-Campos JL, Esther QG, Laura CH, et al. Status of and strategies for improving adherence to COPD treatment. Int J Chron Obstruct Pulmon Dis 2019;14:1503-15. 10.2147/COPD.S170848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO main website. Available online: www.who.int. Date last accessed: March 10, 2020.
- 7.Epidemiology of COVID-19 emergency response mechanism, Chinese center for disease control and prevention, analysis of epidemiological characteristics of COVID-19. Chinese Journal of Epidemiology 2020,41:145-51.32064853 [Google Scholar]
- 8.Miravitlles M, Ribera A. Understanding the impact of symptoms on the burden of COPD. Respir Res 2017;18:67. 10.1186/s12931-017-0548-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baiardini I, Rogliani P, Santus P, et al. Disease awareness in patients with COPD: measurement and extent. Int J Chron Obstruct Pulmon Dis 2018;14:1-11. 10.2147/COPD.S179784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tøttenborg SS, Lange P, Johnsen SP, et al. Socioeconomic inequalities in adherence to inhaled maintenance medications and clinical prognosis of COPD. Respir Med 2016;119:160-7. 10.1016/j.rmed.2016.09.007 [DOI] [PubMed] [Google Scholar]
- 11.Jenkins CR, Chapman KR, Donohue JF, et al. Improving the Management of COPD in Women. Chest 2017;151:686-96. 10.1016/j.chest.2016.10.031 [DOI] [PubMed] [Google Scholar]
- 12.Gregoriano C, Dieterle T, Breitenstein AL, et al. Use and inhalation technique of inhaled medication in patients with asthma and COPD: data from a randomized controlled Trial. Respir Res 2018;19:237. 10.1186/s12931-018-0936-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Humenberger M, Horner A, Labek A, et al. Adherence to inhaled therapy and its impact on chronic obstructive pulmonary disease (COPD). BMC Pulm Med 2018;18:163. 10.1186/s12890-018-0724-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scalone G, Nava S, Ventrella F, et al. Pharmacological approach and adherence to treatment recommendations in frequently and non-frequently exacerbating COPD patients from Italy: MISTRAL - The prospective cohort, observational study. Pulm Pharmacol Ther 2018;53:68-77. 10.1016/j.pupt.2018.09.001 [DOI] [PubMed] [Google Scholar]
- 15.Horvat N, Locatelli I, Kos M, et al. Medication adherence and health-related quality of life among patients with chronic obstructive pulmonary disease. Acta Pharm 2018;68:117-25. 10.2478/acph-2018-0006 [DOI] [PubMed] [Google Scholar]
- 16.Albrecht JS, Park YJ, Hur P, et al. Adherence to Maintenance Medications among Older Adults with Chronic Obstructive Pulmonary Disease. Ann Am Thorac Soc 2016;13:1497-504. 10.1513/AnnalsATS.201602-136OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duarte-de-Araújo A, Teixeira P, Hespanhol V, et al. COPD: understanding patients’ adherence to inhaled medications. Int J Chron Obstruct Pulmon Dis 2018;13:2767-73. 10.2147/COPD.S160982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abdulsalim S, Unnikrishnan M, Manu MK, et al. Structured pharmacist-led intervention programme to improve medication adherence in COPD patients: A randomized controlled study. Res Social Adm Pharm 2018;14:909-14. 10.1016/j.sapharm.2017.10.008 [DOI] [PubMed] [Google Scholar]
- 19.van Boven JF, Cushen B, Sulaiman I, et al. Personalising adherence-enhancing interventions using a smart inhaler in patients with COPD: an exploratory cost-effectiveness analysis. NPJ Prim Care Respir Med 2018;28:24. 10.1038/s41533-018-0092-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taylor TE, Zigel Y, De LC, et al. Advances in Audio-Based Systems to Monitor Patient Adherence and Inhaler Drug Delivery. Chest 2018;153:710-22. 10.1016/j.chest.2017.08.1162 [DOI] [PubMed] [Google Scholar]
- 21.Blasi F, Raddi F, Miravitlles M, et al. Interactive Monitoring Service and COPD: Is it Possible to Reduce Nonadherence? COPD 2015;12:227-32. 10.3109/15412555.2014.933796 [DOI] [PubMed] [Google Scholar]
- 22.Barja-Martínez E, Casas-González S, Simón-López AF, et al. Adherence to inhaled therapy in the outpatient setting. Enferm Clin 2019;29:34-8. [DOI] [PubMed] [Google Scholar]
- 23.Price D, Keininger DL, Viswanad B, et al. Factors associated with appropriate inhaler use in patients with COPD - lessons from the REAL survey. Int J Chron Obstruct Pulmon Dis 2018;13:695-702. 10.2147/COPD.S149404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albrecht JS, Khokhar B, Huang TY, et al. Adherence and Healthcare Utilization among Older Adults with COPD and Depression. Respir Med 2017;129:53-8. 10.1016/j.rmed.2017.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alton S, Farndon L. The impact of community pharmacy-led medicines management support for people with COPD. Br J Community Nurs 2018;23:214-9. 10.12968/bjcn.2018.23.6.214 [DOI] [PubMed] [Google Scholar]
- 26.Dudvarski Ilic A, Zugic V, Zvezdin B, et al. Influence of inhaler technique on asthma and COPD control: a multicenter experience. Int J Chron Obstruct Pulmon Dis 2016;11:2509-17. 10.2147/COPD.S114576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scullion J. The Nurse Practitioners' Perspective on Inhaler Education in Asthma and Chronic Obstructive Pulmonary Disease. Can Respir J 2018;2018:2525319. 10.1155/2018/2525319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hesso I, Gebara SN, Kayyali R. Impact of community pharmacists in COPD management: Inhalation technique and medication adherence. Respir Med 2016;118:22-30. 10.1016/j.rmed.2016.07.010 [DOI] [PubMed] [Google Scholar]
- 29.Wu CX, Hwang CH, Tan WS, et al. Effectiveness of a chronic obstructive pulmonary disease integrated care pathway in a regional health system: a propensity score matched cohort study. BMJ Open 2018;8:e019425. 10.1136/bmjopen-2017-019425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chronic obstructive pulmonary disease group, Chinese respiratory society. Guidelines for the diagnosis and treatment of chronic obstructive pulmonary disease (2013 revision). Chin J Tuberc Respir Dis 2013;36:255-64. [Google Scholar]
- 31.Underner M, Cuvelier A, Peiffer G, et al. The influence of anxiety and depression on COPD exacerbations. Rev Mal Respir 2018;35:604-25. 10.1016/j.rmr.2018.04.004 [DOI] [PubMed] [Google Scholar]
- 32.Xiao T, Qiu H, Chen Y, et al. Prevalence of anxiety and depression symptoms and their associated factors in mild COPD patients from community settings, Shanghai, China: a cross-sectional study. BMC Psychiatry 2018;18:89. 10.1186/s12888-018-1671-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kayhan F, Ilik F, Karamanli H, et al. Major depression in long-term oxygen therapy dependent chronic obstructive pulmonary disease. Perspect Psychiatr Care 2018;54:6-10. 10.1111/ppc.12169 [DOI] [PubMed] [Google Scholar]
- 34.Blakemore A, Dickens C, Chew-Graham CA, et al. Depression predicts emergency care use in people with chronic obstructive pulmonary disease: a large cohort study in primary care. Int J Chron Obstruct Pulmon Dis 2019;14:1343-53. 10.2147/COPD.S179109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wei YJ, Simoni-Wastila L, Albrecht JS, et al. The association of antidepressant treatment with COPD maintenance medication use and adherence in a comorbid Medicare population: a longitudinal cohort study. Int J Geriatr Psychiatry 2018;33:e212-e220. 10.1002/gps.4772 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as