Highlights
-
•
Mental health issues are frequently underestimated in developing countries, although they are expected to be highly prevalent, particularly in the context of a severe socio-economic crisis and political instability.
-
•
Fear of COVID-19 and fear of poverty were independently associated with higher stress and anxiety, while family satisfaction and financial wellness were linked to lower stress.
-
•
Combined fear of COVID-19 and financial distress were associated with further stress and anxiety.
Keywords: COVID-19, fear of poverty, fear of COVID-19, financial well-being, anxiety, stress
Abstract
The COVID-19 pandemic has affected physical and mental health worldwide, particularly vulnerable populations with lower social and economic status. This study explored the independent and combined effects of the COVID-19 and economy-related variables on stress and anxiety among Lebanese adults in a developing country facing a severe socio-economic crisis and political turmoil. A cross-sectional study was conducted online between May 10 and 20, 2020, using the snowball sampling technique. All individuals over 18 were eligible. The final sample included 502 respondents.
Higher stress and anxiety were associated with younger age, female gender, previous higher socio-economic status, having a family member with a chronic disease, fear of not getting access to treatment, fear of COVID-19, and physical violence at home. However, financial wellness and higher family satisfaction were significantly associated with lower stress. The multivariate analysis showed a significant interaction between fear of COVID-19 and financial wellness on estimated marginal means of stress and anxiety. The combined presence of fear of the pandemic and financial hardship is associated with higher stress and anxiety, particularly among women and younger Lebanese adults with difficult home circumstances. Thus, healthcare professionals need to screen for mental health problems among subgroups presenting multiple risk factors.
1. Introduction
In the era of the COVID-19 pandemic, fear has become one of the most common feelings (Lwin et al., 2020), affecting people worldwide with varying intensities (Asmundson and Taylor, 2020). This fear may originate from worrying for oneself, family members, or loved ones, of contracting the severe form of the disease, requiring hospitalization, or even leading to death (Wang et al., 2020).
In response to signs of mental distress observed among some populations in the world early during the pandemic, Holmes and collaborators (Holmes et al., 2020) recently published recommendations to assess mental health consequences among vulnerable communities during a pandemic (Holmes et al., 2020). Low-income workers would constitute one such vulnerable group (Kantamneni, 2020). The vulnerability of populations in developed countries is known to be lower than that of developing countries (Pega et al., 2017; Perehudoff et al., 2019), particularly when the latter also endure a severe socio-economic crisis and political instability as in Lebanon (Bizri et al., 2020).
Lebanon, a Middle-Eastern developing country, declared its first case on February 21 and, at the time of writing, continues to be affected by its consequences on morbidity (over 1,000 positive cases/7,000,000 persons over a period of three months) and mortality (n=26) (Public Health Ministry and Information Ministry, 2020). Although these figures are considered relatively moderate, the pandemic has severely damaged the country's economy due to the strict containment measures imposed by the government since March 15 to limit the spread of the infection (Douglas et al., 2020). The COVID-19 outbreak coincided with an unprecedented economic crisis in Lebanon, where the Lebanese pound has lost 85% of its value. Lebanon has been suffering from severe economic hardship that has its roots in the aftermath of the 1975-1990 civil war and has been aggravated by political turmoil, corruption, and mismanagement of the country's resources (Lebanon economic monitor, 2019). In 2011, the Lebanese population was estimated at 5,202,343 inhabitants, and reached 6,848,925 in 2018 (The World Bank. Lebanon, 2020) following the inflow of Syrian refugees escaping their country embattled since early 2012 (Arezki et al., 2018), further increasing the burden on Lebanon.
The sudden rise in population size, coupled with a dysfunctional system, affected several sectors, particularly the economy, health, and education. Consequently, the World Bank recently downgraded Lebanon from a high-income to upper-middle-income country (Arezki et al., 2018). Many Lebanese have lost their jobs or seen their businesses slow down or go bankrupt. While many of them look to emigrate, most cannot settle outside of the country, thus being forced into living a precarious life of economic insecurity that threatens the whole social construct (Lebanon economic monitor, 2019).
In this context of a “double-hit”, the mental health of the general Lebanese population is likely to be affected. A recent cross-sectional study conducted just before the current crisis showed that around one-third of Lebanese adults were in mental distress (Obeid et al., 2020). Moreover, pandemic-related (Shuja et al., 2020) and poverty-related (Cooper, 2011) fears may both trigger psychological distress and lead to mental illnesses. Therefore, we hypothesize that their combined effects may interact and further increase stress and anxiety. Consequently, this study aimed to assess the independent and combined effects of the COVID-19 and economy-related variables on stress and anxiety among Lebanese adults.
2. Methods
2.1. Study design and sampling
A cross-sectional study was conducted between May 10 and 20, 2020, using an online-based questionnaire created on Google forms. Due to the government-mandated sanitary lockdown, the survey was distributed to all participants through social media platforms and WhatsApp groups, using the snowball sampling technique. All individuals over 18 years of age with access to the internet were eligible; no exclusion criteria were applied. A total of 502 respondents filled out the questionnaire that required between 15 and 20 minutes to complete.
2.2. Ethical approval
The Institutional Review Board of the American University of Science and Technology approved this study protocol (IRB application number AUST-IRB-20200527-01). The topic was explained to all participants in the introductory section of the survey, and consent to participate was implicit. The anonymity of participants was guaranteed throughout the process of data collection and analysis.
2.3. Minimal sample size calculation
The minimum sample size was calculated using the G-Power software version 3.0.10. The calculated effect size was 0.0526, expecting a squared multiple correlation coefficient of 0.05 (R2 deviation from 0) related to the Omnibus test of multiple regression. The minimum necessary sample was n=454, considering an alpha error of 5%, a power of 80%, and allowing 25 predictors to be included in the model.
2.4. Questionnaire
The online questionnaire was available in Arabic, the native language in Lebanon. It consisted of three parts. The first part assessed the socio-demographic features of the participants, such as age, gender, marital status, educational level, employment status, region, and current household monthly income, divided into five levels, according to the official exchange rate (1 USD = 1,500 LBP): no income, low <675,000LBP (450 USD), moderate 675,000-1,500,000LBP (450-1,000 USD), intermediate 1,500,000-3,000,000 LBP (1,000-2,000 USD), and high income > 3,000,000 LBP (2,000 USD). Socioeconomic status was assessed using quartiles of individual income: the household income was divided by the household size, giving a mean income per person. This value distribution was then divided into four quartiles, the lowest quartile related to the lowest socioeconomic status and the highest quartile corresponding to the highest socioeconomic status. Other questions gathered information about medical coverage, smoking and alcohol consumption, self-perception of the financial situation, physical activity before and during the COVID-19 pandemic, and having been infected or in contact with people infected with the virus.
The second part of the questionnaire consisted of a set of 20 questions related to current employment and how it was affected by either the economic crisis (October 2019-February 2020) or the COVID-19 pandemic (March 2020-April 2020), taken separately. This part was only intended for working people and those seeking a job. Examples of the questions asked: Do you have to go out to make a living despite the sanitary lockdown? Are you able to apply social distancing while working (1.5-2m safety distance)? Did your company change the working hours because of the economic crisis or the COVID-19 pandemic? Has your salary/income been affected by the economic crisis or the COVID-19 pandemic? Are you worried about the long-term impact of the economic crisis or the COVID-19 pandemic on your business/job? Did the economic crisis or the COVID-19 pandemic result in decreasing the salaries of employees? Did the economic crisis or the COVID-19 pandemic cause the dismissal of some employees? What were the criteria used to lay-off employees?
The third part of the questionnaire consisted of validated scales allowing the objective evaluation of the fear of COVID-19, distress, and anxiety along with other economic measures. The scales were used after obtaining the due permission from their copyright holders when necessary.
2.4.1. The fear of COVID-19 scale
This 7-item tool is used to measure the extent of fear of the COVID-19 in adult people (Ahorsu et al., 2020). It is scored on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). The total score is calculated by summing the answers to all questions and varies from 1 to 35. Higher scores indicate a greater fear of COVID-19. The Cronbach's alpha for this scale was 0.893.
2.4.2. The Beirut Distress Scale-22 (BDS-22)
The BDS-22 is a scale validated in Lebanon (Barbour et al., 2012), used to measure the level of stress in the general Lebanese adult population. It consists of 22 questions exploring six domains: depressive symptoms, demotivation, psychosomatic symptoms, mood deterioration, intellectual inhibition, and anxiety. Responses are rated on a 4-point Likert-type scale from 0 (not at all) to 3 (all of the times), with higher scores indicating higher levels of stress. The Cronbach's alpha for this scale was 0.965.
2.4.3. The Lebanese Anxiety Scale-10 (LAS-10)
The LAS-10 is a 10-item scale validated in Lebanon (Hallit et al., 2020) used to screen for anxiety in the general Lebanese adult population. Questions 1 to 7 are scored on a 5-point Likert scale from 0 (not present) to 4 (very severe), while items 8-10 are graded on a 4-point Likert scale from 1 (never/almost never) to 4 (almost always), with higher scores indicating higher anxiety. The Cronbach's alpha for this scale was 0.919.
2.4.4. The Family APGAR index
This short self-reported instrument evaluates the satisfaction with global family function (Good et al., 1979). It consists of five questions, each corresponding to a component of family function, i.e., Adaptation, Partnership, Growth, Affection, and Resolve (APGAR). All five items are scored on a 3-point Likert scale: 0 (hardly ever), 1 (some of the time), and 2 (almost always). The total score is obtained by summing the answers to all items and ranges from 0 to 10. Higher scores indicate higher satisfaction with family function. The Cronbach's alpha for this scale was 0.927.
2.4.5. The InCharge Financial Distress/Financial Well-Being scale (IFDFW)
This tool includes eight items that assess the perceived financial distress/financial well-being on a linear scale from 1 to 10 (Prawitz et al., 2006). Lower scores reflect higher financial distress and lower well-being. The Cronbach's alpha for this scale was 0.925. Since this tool is copyrighted, written permission was obtained from the authors to use it and validate it in Lebanon.
2.4.6. Translation procedure and piloting
All the scales used were translated into Arabic, except for the BDS-22 and LAS-10, already validated and available in this language. Three authors performed the forward translation, and the other three, the back translation. Discrepancies between original and translated versions were resolved by consensus; for each scale, zero to one question needed discussion regarding the equivalence between the English and Arabic versions. The questionnaire was then pilot-tested on ten people unfamiliar with the study to check the clarity and reach the final version; only two work-related questions of the sociodemographic part were reformulated for a better comprehension of the questionnaire. The answers of the pilot sample were not included in the final dataset.
2.5. Statistical analysis
Data from Google forms were generated and collected on Excel sheets then transferred to IBM SPSS® software version 23.0 for analysis. Before analyzing it, the database was weighted according to gender, age, and dwelling region, based on figures from the Central Administration of Statistics (Huang and Zhao, 2020). For descriptive analysis, frequency and percentage were used for categorical variables, mean and standard deviation for quantitative variables. For dependent variables (BDS-22 for psychological distress and LAS-10 for anxiety), the median and interquartile range was presented as well; the normal distribution of these variables was confirmed by visual inspection of the histogram, with skewness and kurtosis lower than 1. These conditions are considered compatible with normality in a sample size larger than 300 (Mishra et al., 2019).
For the bivariate analysis of continuous variables, the Student's T-test was used to compare the means between 2 groups and ANOVA to compare between three groups or more, after checking for homogeneity of variances using the Levene's test. In case variances were not homogenous, the corrected T-Test and the Kruskal-Wallis test were used, respectively. After ANOVA and Kruskal-Wallis significant testing, post hoc analyses were conducted using Bonferroni adjustment. A Spearman correlation coefficient was used between continuous variables, and a gamma coefficient to assess the association between ordinal variables. In all cases, a p-value lower than 0.05 was considered significant. To estimate effect size, the Eta squared was used to compare means and the coefficient of variation (r-squared) to calculate correlations.
As for the multivariable analysis, two multiple linear regressions were conducted to assess the correlates of dependent variables in the whole sample, after checking the residues normality, the linearity of the relationship, the absence of multicollinearity, and the homoscedasticity assumptions; a stepwise method was used to reach the most parsimonious model. In both models, the beta coefficient, its 95% Confidence Interval, and the p-value were reported. Independent variables introduced in the models were those that had a p-value lower than 0.1 in the bivariate analysis, taking into account the maximum number allowed of variables to be included given the sample size: sociodemographic, family, health, fear of COVID-19, and economics related variables were added as appropriate. The R-squared and adjusted R-Squared were calculated for the full model, and the partial Eta squared for individual items.
Also, a multivariate analysis using the General Linear Model was conducted on the same dependent variables (BDS-22 and LAS-10); the ENTER method was used to come up with the appropriate model with appropriate assumptions. It allowed assessing the interaction between fear of COVID-19 (FOC) and financial wellness (IFDFW) scales by calculating the estimated marginal means for stress and anxiety among subjects with FOC (high/low categories) and IFDFW (high/low categories): the two variables were dichotomized into high and low categories according to the median. Contrasts shape evaluation (linear, quadratic, cubic, and others) assessed the increase through categories.
3. Results
3.1. Stress, anxiety, and sociodemographic characteristics
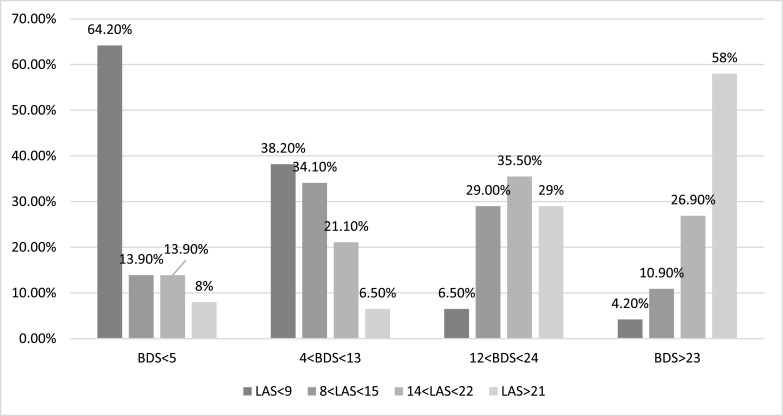
In this sample of the general Lebanese population, psychological distress, as measured by the BDS-22, had a mean of 16.09 (SD=15.38) and a median of 12 [IQR: 4;23], while the values for anxiety (LAS-10) were 15.30 (SD=8.82), and 14 [IQR:8;21], respectively. The normality of the two scales was assumed since skewness and kurtosis were lower than 1 for both, and the sample size larger than 300. The Spearman correlation coefficient between the two scales was 0.613 (p<0.001), while the gamma coefficient between their respective quartiles was 0.657 (p<0.001) (Fig. 1 ).
Fig. 1.
Association between psychological distress (BDS-22) and anxiety (LAS-10) quartiles
(Gamma = 0.657; P<0.001).
Half of the participants were females; the mean age was 42.7 years, the majority were married (58%), had a university degree (88%), and reported their region of residence as Mount Lebanon (44%). The highest percentage of respondents lived in a household of fewer than four persons (32%), and 41% had no dependent children currently. Furthermore, 49% were occasional alcohol consumers, about 67% never smoked cigarettes, and 72% never smoked water pipe. Around 6% reported verbal violence at home, and less than 2% reported other types of violence. The majority of the sample had a job (or was looking for one), 10% were housewives and never worked, 10% were university students, and 8% were retired. A detailed description is presented in Table 1 .
Table 1.
Sociodemographic characteristics, stress and anxiety.
| Characteristic | Frequency(%) N=502(100%) | Unadjusted BDS-22-Mean (SD) | p-value | Eta squared | Unadjusted LAS-10-Mean (SD) | p-value | Eta squared |
|---|---|---|---|---|---|---|---|
| Gender Male Female |
237(47.3%) 265(52.7%) |
13.42(14.45) 18.49(15.83) |
<0.001 | 0.025 |
14.40(9.29) 16.10(8.32) |
0.032 | 0.006 |
| Marital status Single Married Widowed/Divorced |
189(37.6%) 290(57.8%) 23(4.6%) |
19.15(17.62) 14.17(13.22) 15.37(17.70) |
0.003 Ref 0.001 0.161 |
0.024 |
15.23(9.25) 15.28(8.59) 16.03(8.59) |
0.919 | 0.000 |
| Level of education Less than university University degree |
58(11.5%) 445(88.5%) |
17.26(16.32) 15.94(15.28) |
0.542 | 0.000 |
14.58(9.20) 15.39(8.78) |
0.516 | 0.004 |
| Dwelling region Beirut (capital) Mount Lebanon South Lebanon Bekaa plain North Lebanon |
84(16.7%) 222(44.2%) 69(13.8%) 47(9.5%) 80(15.9%) |
12.86(12.88) 16.42(15.48) 15.96(14.31) 16.40(16.42) 18.55(17.48) |
0.095 | 0.022 |
14.71(8.00) 15.59(9.06) 13.68(9.44) 16.30(8.33) 15.89(8.70) |
0.416 | 0.011 |
| Household size Lower than 4 persons 4 persons 5 persons 6 and more |
161(32.1%) 137(27.2%) 122(24.2%) 83(16.5%) |
17.65(15.52) 11.66(12.57) 17.48(15.94) 18.35(17.23) |
<0.001 Ref <0.001 0.668 0.910 |
0.036 |
14.60(8.48) 14.47(9.14) 16.46(8.51) 16.29(9.27) |
0.148 | 0.010 |
| Dependent children None 1 child 2 children 3 or more |
207(41.2%) 46(9.1%) 132(26.3%) 118(23.4%) |
17.64(16.80) 19.35(18.20) 12.79(12.45) 15.83(14.05) |
0.107 | 0.022 |
14.51(9.09) 18.21(9.29) 14.95(8.30) 15.94(8.57) |
0.059 | 0.018 |
| Number of rooms < 5 rooms 5 rooms 6 rooms 7 or more |
167(33.2%) 138(27.6%) 109(218%) 87(17.4%) |
18.13(16.55) 15.12(14.54) 13.50(14.46) 17.01(15.16) |
0.075 | 0.018 |
15.88(8.99) 15.10(9.26) 15.98(8.86) 13.64(7.58) |
0.208 | 0.009 |
| Alcohol consumption Previous None Occasional Regular |
14(2.8%) 197(39.3%) 248(49.3%) 44(8.7%) |
29.52(20.69) 17.23(17.01) 14.99(13.88) 12.98(11.30) |
0.315 | 0.015 |
26.35(7.36) 14.72(8.47) 15.25(8.60) 14.63(9.97) |
<0.001 Ref <0.001 <0.001 <0.001 |
0.048 |
| Cigarette smoking Previous None Occasional Regular |
21(4.1%) 334(66.6%) 87(17.4%) 60(11.9%) |
20.86(19.52) 15.82(15.92) 16.49(14.57) 15.41(11.50) |
0.680 | 0.000 |
18.52(10.37) 14.41(8.61) 17.38(8.45) 16.08(9.37) |
0.009 1.000 Ref 0.030 1.000 |
0.019 |
| Waterpipe smoking Previous None Occasional Regular |
27(5.3%) 363(72.3%) 79(15.7%) 33(6.7%) |
21.42(15.85) 16.04(15.48) 14.02(13.30) 17.39(18.01) |
0.182 | 0.003 |
22.93(8.70) 14.77(8.74) 16.52(9.73) 14.64(7.71) |
<0.001 <0.001 Ref 0.753 0.508 |
0.051 |
| Violence at home* Verbal violence vs no Physical violence vs no Sexual violence vs no Other violence vs no No violence |
30(5.9%) 8(1.6%) 7(1.4%) 8(1.6%) 472(94.1%) |
23.00(16.12) 37.46(15.80) 37.57(16.51) 37.46(15.80) 15.66(15.25) |
0.011 <0.001 <0.001 <0.001 Ref |
0.020 0.036 0.032 0.036 |
20.57(9.47) 31.94(0.49) 31.85(0.38) 31.94(0.49) 14.96(8.69) |
0.001 <0.001 <0.001 <0.001 Ref |
0.027 0.063 0.054 0.063 |
| Professional status Works/looking for a job Housewife/never work Student Retired |
361(71.9%) 52(10.3%) 50(9.9%) 40(7.9%) |
16.19(15.56) 15.10(13.09) 19.99(18.82) 11.72(10.14) |
0.794 | 0.010 |
15.37(8.93) 14.24(8.29) 16.26(9.65) 14.77(7.55) |
0.683 | 0.006 |
| Mean (SD) | Unadjusted Correlation coefficient r |
p-value | R squared | Unadjusted Correlation Coefficient r | p-value | R squared | |
| Age in years | 42.47(14.06) | -0.136 | 0.003 | 0.018 | -0.068 | 0.144 | 0.005 |
| APGAR family | 7.81(2.72) | -0.313 | <0.001 | 0.098 | -0.129 | <0.001 | 0.017 |
More than one answer is possible
Females, previous alcohol drinkers, previous water pipe smokers, and people experiencing violence at home (mostly physical, verbal, sexual, and other types), and those with lower family APGAR scores had significantly higher stress and anxiety; older participants and those living in a household of four had significantly lower stress. Previous alcohol consumers, occasional cigarette smokers, and previous waterpipe smokers had higher anxiety. The largest effect size was observed in violence at home, previous waterpipe smoking status, family size, and APGAR (Table 1).
3.2. Economic characteristics, stress, and anxiety
Participants who subjectively classified themselves as below the poverty line before the crisis had significantly higher stress and anxiety, in addition to those currently labeling themselves in this category. Lower-income categories also had higher stress, while those in socioeconomic status quartile 3 (middle-upper socioeconomic class) had the lowest stress level. Higher fear of poverty was associated with higher stress and anxiety, while financial well-being was correlated with lower stress and anxiety. Regarding stress, the largest effect size regarding was seen in fear of poverty, financial well-being, and the subjective assessment of socioeconomic status before and after COVID-19. As for anxiety, the largest effect size was found in the subjective assessment of socioeconomic status before COVID-19 (Table 2 ).
Table 2.
Economic characteristics, stress and anxiety.
| Characteristic | Frequency(%) N=502(100%) | Unadjusted BDS-22 Mean(SD) | p-value | Eta-Squared | Unadjusted LAS-10 Mean(SD) | p-value | Eta Squared |
|---|---|---|---|---|---|---|---|
| Subjective assessment before COVID No answer Rich Middle class Middle to low Below poverty line |
5(1.0%) 30(6.1%) 448(89.2%) 11(2.1%) 8(1.6%) |
13.39(11.19) 18.75(17.70) 15.32(14.68) 21.80(21.40) 43.43(13.30) |
0.003 0.001 0.001 <0.001 0.022 Ref |
0.063 |
15.42(9.88) 16.13(8.53) 14.92(8.67) 16.60(8.10) 30.92(5.60) |
<0.001 0.015 <0.001 <0.001 0.004 Ref |
0.056 |
| Subjective assessment after COVID No answer Rich Middle class Middle to low Below poverty line |
14(2.8%) 5(1.1%) 327(65.1%) 137(27.2%) 19(3.8%) |
15.10(13.37) 23.92(19.62) 14.64(14.73) 17.58(15.37) 28.81(20.18) |
0.005 0.090 0.477 0.002 0.025 Ref |
0.039 |
14.54(7.85) 19.09(9.39) 14.57(8.66) 16.25(8.73) 20.31(11.01) |
0.025 0.621 1.000 0.054 0.573 Ref |
0.024 |
| Current Health Coverage No Health coverage Private insurance Social security Other public coverage |
53(10.5%) 205(40.8%) 155(30.9%) 90(17.8%) |
18.69(17.92) 15.87(14.77) 17.62(16.61) 12.43(12.18) |
0.220 | 0.012 |
15.76(10.11) 14.97(8.29) 16.53(9.40) 13.62(7.95) |
0.137 | 0.013 |
| Household income Less than 675,000LP 675,000-1,500,000LP 1,500,000-3,000,000LP More than 3,000,000LP |
15(2.9%) 64(12.8%) 149(29.7%) 274(54.5%) |
21.24(20.20) 23.64(18.67) 15.11(13.91) 14.58(14.51) |
0.018 0.215 0.003 0.312 Ref |
0.038 |
17.61(10.39) 15.94(9.26) 16.01(8.68) 14.63(8.70) |
0.273 | 0.007 |
| Socio-economic quartile Quartile 1 Quartile 2 Quartile 3 Quartile 4 |
134(26.6%) 142(28.3%) 119(23.7%) 101(20.1%) |
18.34(16.07) 16.30(16.47) 12.30(13.25) 16.70(14.46) |
0.006 Ref 0.299 0.001 0.421 |
0.021 |
16.87(9.20) 14.58(8.23) 15.26(9.07) 14.21(8.84) |
0.083 | 0.012 |
| Mean (SD) | Unadjusted Correlation (r) | p-value | R-Squared | Unadjusted Correlation (r) | p-value | R-squared | |
| Fear of poverty scale | 6.90(2.65) | 0.230 | <0.001 | 0.053 | 0.192 | <0.001 | 0.037 |
| IFDWF financial well-being scale | 39.9(17.33) | -0.262 | <0.001 | 0.069 | -0.119 | 0.010 | 0.014 |
3.3. Professional characteristics, stress, and anxiety
Table 3 presents the details of the association between professional characteristics, stress, and anxiety. Those who earn daily wages, who were looking for a job before the economic crisis, licensed during the COVID-19 crisis, and currently looking for a job had, significantly higher levels of stress and anxiety. The increase in anxiety was similar, whether due to the economic situation or to the COVID-19 crisis. Those who worked in enterprises that permanently closed or decreased shifts had significantly higher levels of stress and anxiety compared to those who had no change in their employment status. Participants whose enterprise temporarily closed and whose income decreased by 75% had significantly higher mean anxiety scores. Furthermore, overall salary changes and dismissal from work increased stress and anxiety among respondents. Finally, participants worried about how the situation would affect their employment had significantly higher stress and anxiety. Looking for a job and professional changes since the economic crisis start had a large effect size on stress, while enterprise changes since both the economic crisis and COVID-19 started had a large effect size related to anxiety (Table 3).
Table 3.
Professional characteristics, stress and anxiety.
| Characteristic | Frequency(%) N=361(100%) | Unadjusted BDS-22 Mean(SD) | p-value | Eta-Squared | Unadjusted LAS-10 Mean(SD) | p-value | Eta-Squared |
|---|---|---|---|---|---|---|---|
| Public sector work Private sector work |
65(17.9%) 296(82.1%) |
18.70(17.64) 15.64(15.05) |
0.152 | 0.004 | 16.90(10.05) 15.04(08.65) |
0.173 | 0.002 |
| Income basis Own business Project basis Monthly income Daily wages |
81(22.4%) 11(3.1%) 246(68.1%) 23(6.4%) |
12.54(11.23) 18.59(16.62) 16.02(15.58) 29.32(20.84) |
0.005 Ref 0.764 0.150 <0.001 |
0.060 |
15.04(8.08) 15.66(8.91 14.93(8.98) 20.98(9.81) |
0.018 Ref <0.001 0.448 <0.001 |
0.025 |
| Healthcare profession No Yes |
173(48.0%) 187(37.3%) |
16.70(16.20) 15.71(14.98) |
0.549 | 0.001 |
15.24(8.56) 15.49(9.28) |
0.786 | 0.001 |
| Work Before Economic Crisis* Works on his/her own versus no Owns an enterprise versus no Managerial position versus no Employee versus no Looking for a job versus no |
130(35.9%) 93(25.7%) 155(42.8%) 208(57.7%) 41(11.3%) |
15.88(14.77) 14.94(14.21) 16.22(15.28) 17.30(15.72) 26.00(19.07) |
0.777 0.372 0.974 0.111 0.001 |
0.000 0.003 0.000 0.009 0.056 |
16.11(8.66) 16.06(9.42) 14.96(8.63) 16.06(9.57) 18.63(8.82) |
0.237 0.387 0.313 0.077 0.012 |
0.003 0.001 0.005 0.011 0.021 |
| Work DURING COVID crisis* Goes to work now versus no Has absolutely go out versus no Applies social distancing versus no I was licensed from work versus no Job can't be done from home vs no |
197(54.6%) 176(35.1%) 142(39.3%) 16(04.4%) 70(13.9%) |
15.76(15.11) 15.81(15.94) 13.74(14.89) 29.01(17.97) 18.07(16.01) |
0.568 0.655 1.000 0.001 0.261 |
0.000 0.000 0.037 0.030 0.005 |
15.75(9.26) 15.23(8.83) 14.46(8.27) 20.78(11.51) 17.93(8.26) |
0.368 0.764 1.000 0.071 0.008 |
0.003 0.001 0.077 0.017 0.017 |
| Current position AFTER COVID* Works on his/her own versus no Owns an enterprise versus no Managerial position versus no Employee versus no Looking for a job versus no |
125(34.7%) 87(24.0%) 145(40.1%) 205(56.7%) 50(13.9%) |
16.46(15.22) 15.01(14.90) 15.41(14.83) 16.83(15.34) 23.86(18.05) |
0.809 0.422 0.437 0.370 0.005 |
0.000 0.003 0.002 0.004 0.041 |
16.24(8.67) 15.90(9.76) 15.74(9.38) 15.99(9.41) 17.97(9.45) |
0.177 0.551 0.523 0.129 0.049 |
0.003 0.000 0.004 0.007 0.011 |
| Change since economic crisis start No change Permanent closure Temporary closure Work from home Decrease shifts Does not apply |
135(37.4%) 11(3.05%) 53(14.7%) 20(5.5%) 80(22.2%) 61(16.9%) |
12.24(11.84) 31.46(19.15) 15.61(15.60) 19.92(18.89) 17.16(15.58) 20.11(18.13) |
0.002 Ref 0.007 0.110 0.092 0.016 0.003 |
0.079 |
12.64(8.77) 24.75(9.35) 16.87(8.54) 18.51(9.61) 16.73(8.49) 15.56(7.86) |
<0.001 Ref <0.001 0.037 0.070 0.012 0.429 |
0.091 |
| Change since COVID crisis No change Permanent closure Temporary closure Work from home Decrease shifts Does not apply |
46(12.7%) 21(5.8%) 63(17.5%) 79(21.9%) 106(29.4%) 46(12.7%) |
15.37(14.70) 18.51(16.52) 19.16(16.55) 15.37(13.91) 15.05(14.96) 15.87(18.57) |
0.597 | 0.011 |
11.90(8.37) 19.00(6.92) 17.53(9.36) 14.88(8.38) 16.52(9.43) 12.42(7.68) |
0.001 Ref 0.001 0.002 0.058 0.005 0.886 |
0.054 |
| Current Personal Income change No change in income Decrease by 25% Decrease by 50% Decrease by 75% Temporary no salary Was licensed |
152(42.1%) 48(13.3%) 77(21.3%) 53(14.7%) 22(6.1%) 9(2.49%) |
15.08(14.95) 20.18(16.85) 14.19(13.89) 16.62(16.51) 20.53(23.56) 19.36(15.97) |
0.236 | 0.028 |
14.43(9.33) 15.99(8.47) 14.01(8.40) 19.53(8.32) 15.18(8.58) 15.44(8.22) |
<0.001 Ref 1.000 1.000 0.005 1.000 1.000 |
0.047 |
| Current enterprise salary change No change in salaries Decrease by 25% Decrease by 50% Decrease by 75% Temporary no salary Does not apply |
153(42.4%) 58(16.1% 74(20.5%) 13(3.6%) 14(3.9%) 49(13.6%) |
13.13(14.02) 19.76(15.63) 18.11(16.76) 17.20(21.98) 19.21(18.18) 17.51(14.56) |
0.018 Ref 0.003 0.029 0.527 0.131 0.061 |
0.034 |
12.65(8.56) 19.15(9.23) 17.82(8.46) 12.88(11.26) 15.77(8.79) 16.28(7.07) |
<0.001 Ref <0.001 <0.001 1.000 1.000 0.157 |
0.081 |
| Current enterprise employees licensing No change Licensing by 25% Licensing by 50% Licensing by 75% Licensing all employees Does not apply |
231(64.0%) 36(10.0%) 19(5.3%) 7(1.9%) 7(1.9%) 61(16.9%) |
13.42(13.77) 21.49(18.24) 32.91(21.40) 28.36(22.11) 9.50(5.77) 17.93(13.65) |
0.001 Ref 0.015 0.001 0.007 0.147 0.023 |
0.128 |
14.00(8.78) 19.01(10.15) 18.87(6.41) 18.14(10.86) 10.92(8.05) 17.63(8.06) |
0.001 Ref 0.022 0.311 1.000 1.000 0.062 |
0.063 |
| Mean (SD) | Unadjusted Correlation (r) | p-value | R-square | Unadjusted Correlation (r) | p-value | R-square | |
| Years of experience | 16.81(10.30) | -0.145 | 0.007 | 0.021 | -0.066 | 0.222 | 0.004 |
| Years current position | 12.88(10.19) | -0.085 | 0.115 | 0.007 | 0.016 | 0.764 | 0.000 |
| Worry that crisis would affect job | 7.80(2.51) | 0.143 | 0.008 | 0.020 | 0.121 | 0.024 | 0.015 |
More than one option is possible
3.4. COVID-19 exposure, health matters, stress, and anxiety
As for health-related matters, doing physical activity during confinement significantly reduced stress, while fear of going out to receive treatment for chronic disease, worrying about not having access to therapy, having a family member with a chronic disease, and worrying for them increased both stress and anxiety. The largest effect size was found for fear of COVID-19, worrying about family members, and fear of not accessing treatment in case of a disease (Table 4 ).
Table 4.
COVID-19 exposure, health characteristics, stress and anxiety.
| Characteristic | Frequency(%) N=502(100%) | Unadjusted BDS-22 Mean(SD) | p-value | Eta Squared | Unadjusted LAS-10 Mean(SD) | p-value | Eta Squared |
|---|---|---|---|---|---|---|---|
| Had COVID-19 infection No COVID-19 infection |
3(0.6%) 499(99.4%) |
24.07(22.17) 16.04(15.35) |
0.349 | 0.001 | 16.62(5.99) 15.29(8.85) |
0.787 | 0.001 |
| Contact with COVID-19 (work, family, store) No contact with COVID-19 |
18(3.5%) 484(96.5%) |
13.12(21.29) 16.20(15.15) |
0.555 | 0.004 | 12.24(9.68) 15.41(8.78) |
0.139 | 0.006 |
| Knows someone infected Does not know anybody infected |
145(28.8%) 357(71.2%) |
14.94(15.52) 16.57(15.32) |
0.283 | 0.001 | 16.08(9.06) 14.98(8.72) |
0.208 | 0.004 |
| Visiting/receiving friends No visiting/receiving friends |
109(21.8%) 393(78.2%) |
18.28(17.76) 15.49(14.63) |
0.134 | 0.006 | 14.80(8.44) 15.43(8.93) |
0.506 | 0.001 |
| Visiting/receiving family No visiting/receiving family |
311(61.9%) 191(38.1%) |
16.31(14.85) 15.74(16.26) |
0.687 | 0.001 | 15.63(8.67) 14.75(9.07) |
0.274 | 0.005 |
| Physical activity No physical activity |
321(64.0%) 181(36.0%) |
14.06(14.45) 19.71(16.35) |
<0.001 | 0.030 | 14.91(8.43) 15.99(9.46) |
0.189 | 0.004 |
| Chronic disease No chronic disease |
103(20.5%) 399(79.5%) |
13.83(12.56) 16.68(16.00) |
0.055 | 0.003 | 15.12(8.05) 15.34(9.02) |
0.817 | 0.000 |
| Regular treatment for chronic disease No regular treatment Does not apply |
127(25.4%) 40(8.0%) 334(66.6%) |
16.95(15.60) 20.62(18.59) 15.22(14.81) |
0.183 | 0.010 | 16.00(9.13) 14.14(8.89) 15.17(8.70) |
0.457 | 0.002 |
| Fear no access to treatment No Yes Does not apply |
153(30.5%) 136(27.0%) 213(42.4%) |
11.80(13.03) 22.16(16.22) 15.32(15.26) |
<0.001 <0.001 Ref <0.001 |
0.069 |
12.72(8.17) 19.46(8.34) 14.50(8.68) |
<0.001 <0.001 Ref <0.001 |
0.097 |
| Fear to go out get treatment No Yes Does not apply |
217(43.2%) 77(15.4%) 208(41.4%) |
13.71(13.88) 23.30(16.14) 15.90(15.84) |
<0.001 <0.001 Ref 0.001 |
0.046 |
14.48(9.06) 17.78(8.01) 15.22(8.73) |
0.018 0.014 Ref 0.088 |
0.018 |
| Family member has chronic disease No Yes Does not apply |
199(39.6%) 261(52.1%) 42(8.3%) |
14.22(14.22) 17.28(16.06) 17.67(15.92) |
0.063 | 0.013 |
13.98(7.78) 16.08(9.25) 16.61(9.02) |
0.048 Ref 0.009 0.055 |
0.017 |
| Worried family member No Yes Does not apply |
96(19.1%) 268(53.4%) 138(27.4%) |
10.94(12.13) 19.12(16.67) 13.81(13.43) |
<0.001 Ref <0.001 0.257 |
0.053 |
12.53(8.80) 17.06(8.88) 13.79(7.98) |
<0.001 Ref <0.001 0.821 |
0.041 |
| Mean(SD) | Unadjusted Correlation (r) | p-value | R-Squared | Unadjusted Correlation (r) | p-value | R-Squared | |
| Fear of COVID-19 | 11.35(6.03) | 0.408 | <0.001 | 0.166 | 0.282 | <0.001 | 0.080 |
3.5. Correlates of stress and anxiety: multivariable analysis
In the multivariable analysis, higher stress was associated with lower age, female gender, previous higher socioeconomic status, having a family member with chronic disease, being afraid of not having access to treatment, fear of COVID-19, and physical violence at home, while financial wellness and higher APGAR family scores were significantly associated with lower stress. Financial well-being, fear of COVID-19, and age had the largest effect size; the full model could explain around 75% of the stress (Table 5 ).
Table 5.
Multivariable analyses: Correlates of stress and anxiety.
| Model | Unstandardized beta | p-value | 95%CI of Unstandardized beta | Partial Eta Squared | R-Square (Adjusted R-Squared) of Model |
|---|---|---|---|---|---|
|
Correlates of stress (All sample)* Fear of COVID-19 score Age Physical violence at home APGAR family score IFDFW wellness score Female gender Socioeconomic status (higher versus lower) Afraid no access to a chronic treatment Family member with chronic disease |
0.975 -0.288 39.325 -1.316 -0.137 4.520 1.546 3.430 0.512 |
<0.001 <0.001 <0.001 <0.001 <0.001 <0.001 0.004 0.008 0.027 |
0.786; 1.163 -0.367; -0.208 30.215; 48.435 -1.724; -0.908 -0.203; -0.071 2.365; 6.675 0.494; 2.598 0.900; 5.959 0.057; 0.967 |
0.369 0.393 0.020 0.163 0.435 0.069 0.029 0.033 0.063 |
0.808(0.733) |
|
Correlates of anxiety (All sample)* Afraid no access to a chronic treatment Fear of COVID-19 score Physical violence at home Age Fear of poverty score APGAR family score Family member with chronic disease Worried for family member Number of dependent children Current cigarette smoking Female gender Socioeconomic status (higher versus lower) |
2.933 0.325 23.969 -0.098 0.424 -0.408 0.488 2.338 1.177 2.672 1.898 0.842 |
<0.001 <0.001 <0.001 0.001 0.002 0.002 0.001 0.002 0.001 0.008 0.007 0.023 |
1.300; 4.566 0.204; 0.447 18.070; 29.868 -0.154; -0.041 0.151; 0.696 -0.663; -0.152 0.199; 0.777 0.867; 3.809 0.502; 1.851 0.714; 4.631 0.521; 3.275 0.116; 1.568 |
0.024 0.345 0.015 0.444 0.046 0.099 0.054 0.018 0.075 0.032 0.012 0.015 |
0.820(0.684) |
Stepwise Likelihood ratio method; linear regression, assumptions checked. Included in first step: age, gender, household size, number of dependent children, number of rooms, alcohol consumption, cigarette consumption, waterpipe consumption, fear of COVID score, violence at home (physical, sexual, other), Professional status (forced), socioeconomic status, fear of poverty scale, APGAR family score, having a chronic disease, being afraid of no access to treatment, being afraid of going out for treatment, having a family member with a chronic disease, being worried about a family member with chronic diseases, sports during confinement, IFDWF wellness scale
Similar factors affected anxiety, in addition to fear of poverty, worrying about a family member with a chronic disease, the number of dependent children, and current cigarette smoking. The largest effect size was detected in fear of COVID-19, age, and APGAR family scale; the model could explain around 70% of the anxiety (Table 5).
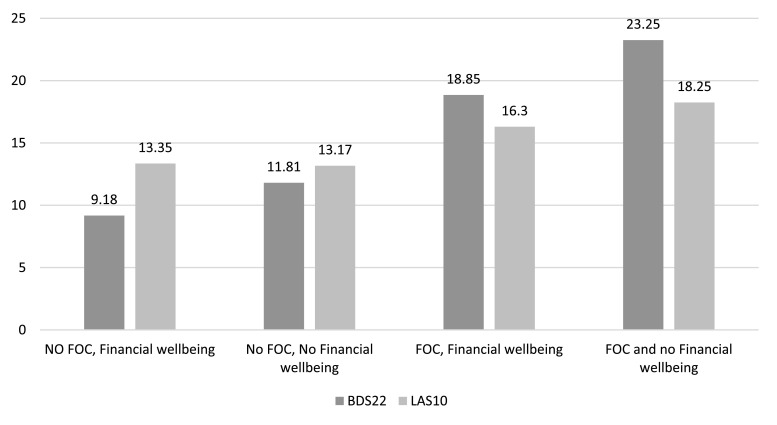
3.6. Interaction between fear of COVID and financial wellness scores
The multivariate analysis showed a significant interaction between fear of COVID-19 (FOC) and financial wellness (IFDFW) scores on estimated marginal means of stress (p<0.001) and anxiety (p<0.001). Estimated marginal means showed a significant linear increase of contrasts between the four categories of people: those with no FOC and IFDFW (Category 0), those with no FOC and no IFDFW (Category 1), those with FOC and IFDFW (Category 2), and those with FOC and no IFDFW (Category 3) (Fig. 2 ). Compared to people with no fear of COVID-19 and financial well-being (BDS-22=9.18; LAS-10=13.35), financial distress added some stress (BDS-22=11.81) and anxiety (LAS-10=13.17), followed by a higher increase related to the fear of COVID-19 (BDS-22=18.85 and LAS-10=16.30), while the highest increase in stress (BDS-22=23.25) and anxiety (LAS-10=18.25) was found in subjects presenting high fear of COVID-19 and financial distress.
Fig. 2.
Estimated marginal means of stress (BDS-22) and anxiety (LAS-10), through categories of Fear of COVID (FOC) and Financial Well-being (IFDFW). p<0.001 for linear increase per category.
4. Discussion
This study explored the cumulative effect of the COVID-19 pandemic and the current economic situation on mental health among the general population in Lebanon. Our results showed that higher stress and anxiety levels were associated with younger adulthood, female gender, previous higher socioeconomic status, having a family member with a chronic disease, being afraid of not getting access to treatment, fear of COVID-19, and physical violence at home. Moreover, higher anxiety was also associated with fear of poverty, the number of dependent children, current cigarette smoking, and worrying about a family member with a chronic disease. However, financial wellness and higher APGAR family scores were associated with lower stress levels.
4.1. COVID-19 and health related factors
Although the pandemic is relatively new, a review of preliminary evidence from China suggests that symptoms of anxiety and depression (16-28%) and self-reported stress (8%) are common psychological reactions to the COVID-19 pandemic and may be associated with disturbed sleep (Rajkumar, 2020). An explanation for this increase in mental health issues is the excess use of social media and exposure to COVID-19 related information and misinformation (Gao et al., 2020). Indeed, COVID-19 might be considered similar to deep existential crises or a traumatic experience that may lead to the appearance or exacerbation of a severe mental disorder and loss of life meaning and satisfaction (Tomaszek and Muchacka-Cymerman, 2020)
Moreover, our results showed that younger adults and female gender were associated with higher stress during the pandemic. This finding is similar to that described in China, where student status, female gender, and having a chronic illness were significantly associated with a higher psychological impact of the outbreak and higher levels of stress and anxiety (p<0.05). Although researchers did not compute the fear of COVID-19, they found that worrying about contracting the disease and about family members getting it was also associated with higher stress and anxiety (Wang et al., 2020). Another study from China found that younger age was a major factor correlated to generalized anxiety disorder, and that younger people were at risk of mental illness (Huang and Zhao, 2020). In Northern Spain, younger individuals with chronic diseases reported more symptoms than the rest of the population, particularly at the start of the pandemic (Ozamiz-Etxebarria et al., 2020), while in Italy, the female gender, younger age, and having relatives infected with COVID-19 were associated with higher anxiety (Mazza et al., 2020). Regional studies also found similar results. Indeed, in Turkey, the female gender and having a chronic disease (among other factors) were associated with anxiety during the current pandemic (Ozdin and Bayrak Ozdin, 2020). An Iranian study also found that female gender, younger age, and having a family member with COVID-19 were associated with higher levels of anxiety (Moghanibashi-Mansourieh, 2020). A possible explanation of those common findings is that women might have a biological tendency towards stress and anxiety (Songtachalert et al., 2018), feel challenged by taking care of their families and children in the context of homeschooling, and be more subject to gender-based violence (Keynejad et al., 2020), while younger people may be worried about their future and generally have higher need for in-person peer-interaction/dating (which are off-limits during lockdown), leading to increased stress/anxiety during and after the pandemic (Groarke et al., 2020; Zhao et al., 2020). Further studies are needed to add more insights and confirm these results.
Another finding of the study is that physical violence at home was associated with higher stress and anxiety, contrary to family satisfaction measured by the APGAR scale. These results are in line with those of other published works showing that family support enhances mental health (Cheng et al., 2017; Sprusinska, 1994), while domestic violence is a source of mental disorders (Akyazi et al., 2018). Specific studies should address these concepts and their differential effects on the mental health of women versus men.
4.2. Economic insecurity
A previous higher socioeconomic status and a current fear of poverty were associated with higher stress, while current financial wellness was correlated with lower stress. A higher number of dependent children was also associated with anxiety. A previous study has shown that rising unemployment, poverty, and social insecurity are associated with stress (Cooper, 2011). The association is even steeper in low- and middle-income countries, where diversity of poverty measures is related to several mental disorders (Lund et al., 2010).
The current situation might result in alarming consequences, including increased trends in the prevalence of psychiatric illnesses, such as anxiety, mood disorders, and suicide rates (Haw et al., 2015; Ozamiz-Etxebarria et al., 2020), alcohol-related disorders, and illicit drug use (Cooper, 2011). Higher anxiety was correlated to economic insecurity and smoking status, similarly to an Italian study in which job security perception appeared to be the most important predictive factor for anxiety and smoking compared to other socioeconomic factors. It is noteworthy that the association got stronger as the insecurity grew, while a high income was associated with decreased anxiety (Bert et al., 2018). Studies reported that the detrimental consequences of employment insecurity on stress and mental health persisted until older age (Kalil et al., 2010). Whether the current mental problems identified by our study will have a long-term impact on the general Lebanese population should be evaluated using prospective studies.
4.3. Interaction between fear of COVID-19 and financial wellness
The analysis of the combined effect of the COVID-19 pandemic and financial wellness (IFDFW) demonstrated that the presence of both COVID-19 fear and financial hardship significantly increased stress and anxiety (p<0.001 for both interactions). Although studies did not previously discuss a similar topic, it is evident that the Lebanese population is at an increased risk of severe mental health disorders that should be addressed, particularly among those living with both fears of COVID-19 and poverty. A review based on a theoretical model explored the effect of economic uncertainty on mental health in the COVID-19 pandemic context. They argued that economic and employment uncertainties might affect psychological well-being through social identity disturbance (Godinic et al., 2020). Therefore, we believe that our results only reveal the tip of the iceberg; the most vulnerable populations were probably not reached by our study. Health authorities should take adequate measures to train health professionals on screening and identifying these disorders in both general and primary healthcare settings, and refer them for specialized medical management (Geyti et al., 2018). Moreover, improving access to psychiatric care is also recommended, taking the example of developed countries. Telepsychiatry, currently limited in Lebanon (Pereira-Sanchez et al., 2020), might be an efficient tool since it offers an opportunity for mental health management during confinement.
4.4. Strengths and limitations
The validated scales used had very good to excellent reliability, and the sample size had adequate power for conducting the multivariate analysis, with appropriate adjustment on multiple potential confounders. Moreover, exposure-effect relationships were shown for associations between continuous independent and dependent variables. Despite weighting over gender, age, and geographical regions, selection bias might be present, as the sample included a high percentage of university-educated participants, probably due to the use of online data collection thus, leading to the participation of more educated individuals, with high computer literacy, and internet access. However, since the education level was taken into account in the multivariable analysis and did not significantly affect stress and anxiety, it is unlikely that it would significantly bias our results. Another potential limitation is the information bias related to the self-assessment and declaration of information, which might cause a non-differential error and drive the results towards the null, leading to underestimation of some associations. Finally, despite the inclusion of several potential confounders in the multivariable models, residual confounding is still possible. Additional face-to-face studies that take into account all these pitfalls would be recommended in the future to confirm our results. Longitudinal studies are also warranted to follow up on the mental health of Lebanese, particularly after the steepening of the socio-economic crisis, the surge of COVID-19 cases, the overwhelming of the health system, and finally, the blast of Beirut that occurred on August 4. We hypothesize that the mental health of Lebanese might have worsened alarmingly.
5. Conclusion
The fears of COVID-19 and economic insecurity are associated with higher stress and anxiety, particularly among women and younger Lebanese subjects with difficult home circumstances. The combined presence of pandemic-related fears and financial hardship further increased stress and anxiety, demonstrating the need to screen for mental health problems among subgroups presenting multiple risk factors.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Pascale SALAMEH: Methodology, Formal analysis, Writing - original draft, Supervision. Aline HAJJ: Writing - review & editing. Danielle A BADRO: Writing - review & editing. Carla ABOU SELWAN: Writing - review & editing. Randa AOUN: Writing - review & editing. Hala SACRE: Conceptualization, Writing - review & editing, Project administration.
Declaration of competing interest
The authors have no conflict of interest to declare.
Acknowledgments
The authors would like to thank all the persons who helped distribute the questionnaire, particularly Dr Fady Farhat, Dr Zahraa Shaitly, Mrs Joumana Sleilaty, and Mr Jihad Gerges.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113520.
Appendix. Supplementary materials
References
- Ahorsu D.K., Lin C.Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00270-8. https://10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akyazi S., Tabo A., Guveli H., Ilnem M.C., Oflaz S. Domestic Violence Victims in Shelters: What Do We Know About Their Mental Health? Community Ment Health J. 2018;54(3):361–369. doi: 10.1007/s10597-018-0240-1. https://10.1007/s10597-018-0240-1 [DOI] [PubMed] [Google Scholar]
- Arezki R., Mottaghi L., Barone A., Fan R.Y., Harb A.A., Karasapan O.M., Matsunaga H., Nguyen H., de Soyres F. Middle East and North Africa Economic Monitor. World Bank; Washington, DC: 2018. A New Economy in Middle East and North Africa. ©. [Google Scholar]
- Asmundson G.J.G., Taylor S. Coronaphobia: Fear and the 2019-nCoV outbreak. J Anxiety Disord. 2020;70 doi: 10.1016/j.janxdis.2020.102196. https://10.1016/j.janxdis.2020.102196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbour B., Saadeh N., Salameh P. Psychological distress in Lebanese young adults: constructing the screening tool ‘BDS-22.’. International Journal of Culture and Mental Health. 2012;5(2):94–108. https://10.1080/17542863.2011.563043 [Google Scholar]
- Bert F., Gualano M.R., Thomas R., Vergnano G., Voglino G., Siliquini R. Exploring the possible health consequences of job insecurity: a pilot study among young workers. Gac Sanit. 2018 doi: 10.1016/j.gaceta.2018.08.011. https://10.1016/j.gaceta.2018.08.011 [DOI] [PubMed] [Google Scholar]
- Bizri A., Khachfe H., Fares M., Musharrafieh U. COVID-19 Pandemic: An Insult Over Injury for Lebanon. Journal of Community Health. 2020 doi: 10.1007/s10900-020-00884-y. https://10.1007/s10900-020-00884-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y., Zhang L., Wang F., Zhang P., Ye B., Liang Y. The effects of family structure and function on mental health during China's transition: a cross-sectional analysis. BMC Fam Pract. 2017;18(1):59. doi: 10.1186/s12875-017-0630-4. https://10.1186/s12875-017-0630-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper B. Economic recession and mental health: an overview. Neuropsychiatr. 2011;25(3):113–117. [PubMed] [Google Scholar]
- Douglas M., Katikireddi S.V., Taulbut M., McKee M., McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369:m1557. doi: 10.1136/bmj.m1557. https://10.1136/bmj.m1557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231924. https://10.1371/journal.pone.0231924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geyti C., Dalsgaard E.M., Sandbaek A., Maindal H.T., Christensen K.S. Initiation and cessation of mental healthcare after mental health screening in primary care: a prospective cohort study. BMC Fam Pract. 2018;19(1):176. doi: 10.1186/s12875-018-0864-9. https://10.1186/s12875-018-0864-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godinic D., Obrenovic B., Khudaykulov A. Effects of Economic Uncertainty on Mental Health in the COVID-19 Pandemic Context: Social Identity Disturbance, Job Uncertainty and Psychological Well-Being Model. International Journal of Management Science and Business Administration. 2020;6(1):61–74. [Google Scholar]
- Good M.-J., Smilkstein G., Good B., Shaffer T., Arons T. The Family APGAR Index: A Study of Construct Validity. The Journal of Family Practice. 1979;8(3):577–582. [Google Scholar]
- Groarke J.M., Berry E., Graham-Wisener L., McKenna-Plumley P.E., McGlinchey E., Armour C. Loneliness in the UK during the COVID-19 pandemic: Cross-sectional results from the COVID-19 Psychological Wellbeing Study. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0239698. https://10.1371/journal.pone.0239698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallit S., Obeid S., Haddad C., Hallit R., Akel M., Haddad G., Soufia M., Khansa W., Khoury R., Kheir N., Abi Elias Hallit C., Sacre H., Salameh P. Construction of the Lebanese Anxiety Scale (LAS-10): a new scale to assess anxiety in adult patients. Int J Psychiatry Clin Pract. 2020:1–8. doi: 10.1080/13651501.2020.1744662. https://10.1080/13651501.2020.1744662 [DOI] [PubMed] [Google Scholar]
- Haw C., Hawton K., Gunnell D., Platt S. Economic recession and suicidal behaviour: Possible mechanisms and ameliorating factors. Int J Soc Psychiatry. 2015;61(1):73–81. doi: 10.1177/0020764014536545. https://10.1177/0020764014536545 [DOI] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. https://10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. https://10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalil A., Ziol-Guest K.M., Hawkley L.C., Cacioppo J.T. Job insecurity and change over time in health among older men and women. J Gerontol B Psychol Sci Soc Sci. 2010;65B(1):81–90. doi: 10.1093/geronb/gbp100. https://10.1093/geronb/gbp100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantamneni N. The impact of the COVID-19 pandemic on marginalized populations in the United States: A research agenda. J Vocat Behav. 2020 doi: 10.1016/j.jvb.2020.103439. https://10.1016/j.jvb.2020.103439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keynejad, R., Hanlon, C., Howard, L., 2020. Psychological interventions for common mental disorders in women experiencing intimate partner violence in low-income and middle-income countries: a systematic review and meta-analysis. 7 (2), 173-190. https://10.1016/S2215-0366(19)30510-3. [DOI] [PMC free article] [PubMed]
- Lebanon economic monitor . Global Practice for Macroeconomics, Trade & Investment, Middle East and North Africa Region. 2019. so when gravity beckons, the poor don't fall.http://documents.worldbank.org/curated/en/349901579899850508/pdf/Lebanon-Economic-Monitor-So-When-Gravity-Beckons-the-Poor-Dont-Fall.pdf (accessed 22 May 2020) [Google Scholar]
- Lund C., Breen A., Flisher A.J., Kakuma R., Corrigall J., Joska J.A., Swartz L., Patel V. Poverty and common mental disorders in low and middle income countries: A systematic review. Soc Sci Med. 2010;71(3):517–528. doi: 10.1016/j.socscimed.2010.04.027. https://10.1016/j.socscimed.2010.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lwin M.O., Lu J., Sheldenkar A., Schulz P.J., Shin W., Gupta R., Yang Y. Global Sentiments Surrounding the COVID-19 Pandemic on Twitter: Analysis of Twitter Trends. JMIR Public Health Surveill. 2020;6(2):e19447. doi: 10.2196/19447. https://10.2196/19447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int J Environ Res Public Health. 2020;17(9) doi: 10.3390/ijerph17093165. https://10.3390/ijerph17093165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra P., Pandey C.M., Singh U., Gupta A., Sahu C., Keshri A. Descriptive statistics and normality tests for statistical data. Ann Card Anaesth. 2019;22(1):67–72. doi: 10.4103/aca.ACA_157_18. https://10.4103/aca.ACA_157_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102076. https://10.1016/j.ajp.2020.102076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obeid S., Lahoud N., Haddad C., Sacre H., Akel M., Fares K., Salameh P., Hallit S. Factors associated with depression among the Lebanese population: Results of a cross-sectional study. Perspect Psychiatr Care. 2020 doi: 10.1111/ppc.12518. https://10.1111/ppc.12518 [DOI] [PubMed] [Google Scholar]
- Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. 2020;36(4) doi: 10.1590/0102-311X00054020. https://10.1590/0102-311X00054020 [DOI] [PubMed] [Google Scholar]
- Ozdin S., Bayrak Ozdin S. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry. 2020 doi: 10.1177/0020764020927051. https://10.1177/0020764020927051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pega F., Liu S.Y., Walter S., Pabayo R., Saith R., Lhachimi S.K. Unconditional cash transfers for reducing poverty and vulnerabilities: effect on use of health services and health outcomes in low- and middle-income countries. Cochrane Database Syst Rev. 2017;11 doi: 10.1002/14651858.CD011135.pub2. https://10.1002/14651858.CD011135.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perehudoff S.K., Alexandrov N.V., Hogerzeil H.V. Legislating for universal access to medicines: a rights-based cross-national comparison of UHC laws in 16 countries. Health Policy Plan. 2019;34(Supplement_3):iii48–iii57. doi: 10.1093/heapol/czy101. https://10.1093/heapol/czy101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira-Sanchez V., Adiukwu F., El Hayek S., Bytyci D.G., Gonzalez-Diaz J.M., Kundadak G.K., Larnaout A., Nofal M., Orsolini L., Ramalho R., Ransing R., Shalbafan M., Soler-Vidal J., Syarif Z., Teixeira A.L.S., da Costa M.P. COVID-19 effect on mental health: patients and workforce. Lancet Psychiatry. 2020;7(6):e29–e30. doi: 10.1016/S2215-0366(20)30153-X. https://10.1016/S2215-0366(20)30153-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prawitz, A., Garman, E.T., Sorhaindo, B., O'Neill, B., Kim, J., Drentea, P., 2006. Incharge Financial Distress/Financial Well-Being Scale: Development, Administration, and Score Interpretation Financial Counseling and Planning 17 (1), 34-50.
- Public Health Ministry and Information Ministry. Daily situation report, 2020. https://corona.ministryinfo.gov.lb (accessed 25 May 2020).
- Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102066. https://10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuja K.H., Aqeel M., Jaffar A., Ahmed A. COVID-19 Pandemic and Impending Global Mental Health Implications. Psychiatr Danub. 2020;32(1):32–35. doi: 10.24869/psyd.2020.32. https://10.24869/psyd.2020.32 [DOI] [PubMed] [Google Scholar]
- Songtachalert T., Roomruangwong C., Carvalho A.F., Bourin M., Maes M. Anxiety Disorders: Sex Differences in Serotonin and Tryptophan Metabolism. Curr Top Med Chem. 2018;18(19):1704–1715. doi: 10.2174/1568026618666181115093136. https://10.2174/1568026618666181115093136 [DOI] [PubMed] [Google Scholar]
- Sprusinska E. The Family APGAR Index: study on relationship between family function, social support, global stress and mental health perception in women. Int J Occup Med Environ Health. 1994;7(1):23–32. [PubMed] [Google Scholar]
- Tomaszek K., Muchacka-Cymerman A. Thinking about My Existence during COVID-19, I Feel Anxiety and Awe—The Mediating Role of Existential Anxiety and Life Satisfaction on the Relationship between PTSD Symptoms and Post-Traumatic Growth. International Journal of Environmental Research and Public Health. 2020;17:7062. doi: 10.3390/ijerph17197062. https://10.3390/ijerph17197062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. https://10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank. Lebanon, 2020. https://data.worldbank.org/country/lebanon (accessed 22 May 2020).
- Zhao S.Z., Wong J.Y.H., Wu Y., Choi E.P.H., Wang M.P., Lam T.H. Social Distancing Compliance under COVID-19 Pandemic and Mental Health Impacts: A Population-Based Study. Int J Environ Res Public Health. 2020;17(18) doi: 10.3390/ijerph17186692. https://10.3390/ijerph17186692 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.