Abstract
Understanding processes that support the well-being of the unprecedented numbers of forcibly displaced people throughout the world is essential. Growing evidence documents post-migration stressors related to marginalization as key social determinants of refugee mental health. The goal of this RCT was to rigorously test a social justice approach to reducing high rates of distress among refugees in the U.S. The 6-month multi-level, strengths-based Refugee Well-being Project (RWP) intervention brought together university students enrolled in a 2-semester course and recently-resettled refugees to engage in mutual learning and collaborative efforts to mobilize community resources and improve community and systems responsiveness to refugees. Data collected from 290 Afghan, Great Lakes African, Iraqi, and Syrian refugees at four time points over 12 months was used to test the effectiveness of RWP to reduce distress (depression and anxiety symptoms) and increase protective factors (English proficiency, social support, connection to home and American cultures). Intention-to-treat analyses using multilevel modeling revealed significant intervention effects for all hypothesized outcomes. Results provide evidence to support social justice approaches to improving refugee mental health. Findings have implications for refugees worldwide, and for other immigrant and marginalized populations who experience inequities in resources and disproportionate exposure to trauma/stress.
Keywords: advocacy, community-based participatory research, multilevel intervention, mutual learning, refugee mental health, social determinants of mental health
As migration and displacement throughout the world continue to grow, it has become even more urgent to understand and ameliorate the burden of social inequities and health disparities experienced by refugees and other immigrants, who typically have higher rates of psychological distress, lingering physical ailments, limited material resources, and loss of meaningful social roles and support, which are often compounded by poverty, discrimination, and devaluation of their cultural practices (Annan, Green, & Brier, 2013; Beiser & Hou, 2017; Kim, 2016; Miller & Rasmussen, 2014; Rasmussen et al., 2010). At the end of 2018, there were 70.8 million forcibly displaced people worldwide (UNHCR, 2019). Of that number, 25.9 million were refugees, who left their country of origin because of a well-founded fear of persecution, conflict, or violence. Four of the largest refugee groups most recently resettled in the U.S. are Afghans, Africans from the Great Lakes Region (Burundi, Democratic Republic of Congo, Republic of the Congo, Rwanda), Iraqis, and Syrians, who together comprise more than 33% of refugees resettled in the U.S. from 2008–2016 (U.S. Department of Homeland Security, 2018).
Refugees are at high risk for mental health problems because of being exposed to violence and conflict in their home countries, fleeing under life-threatening conditions, being separated from family, living in unsafe overcrowded camps without access to adequate food, education, health care, or employment, and because of the extensive stress associated with beginning their lives in a new country. A meta-analysis of 145 studies found that almost one-third of refugees (30.6%) have PTSD (Steel et al., 2009). Similarly, refugees in the United States experience higher rates of psychological distress than the general population or other immigrants (Fazel, Wheeler, & Danesh, 2005; Pham, Vinck, & Stover, 2009; Porter & Haslam, 2005).
Early research on refugee mental health focused on the relationship between past traumas and mental health problems with an emphasis on individual trauma-focused solutions (Hinton et al., 2005; Neuner, Schauer, Klaschik, Karunakara, & Elbert, 2004; Stepakoff et al., 2006). However, growing research has documented the link between post-migration stressors and mental health among refugees (Miller & Rasmussen, 2010; Rasmussen et al., 2010), which, for refugees in the U.S., include limited English proficiency, lack of social support and valued social roles, and poverty. English proficiency is associated with mental health, including predicting lower levels of depression 10 years post-resettlement (Beiser & Hou, 2001). Social support is also strongly associated with and/or a powerful predictor of refugee mental health (Birman & Tran, 2008; Carlsson, Mortensen, & Kastrup, 2006; Miller et al., 2002), and has been found to be more related to depression symptoms than past trauma (Gorst-Unsworth & Goldenberg, 1998).
Refugees are also at high risk for mental health problems because of stressors related to living in poverty. Upon arrival, refugees receive 3–6 months of financial assistance from the U.S. government. During this time, they are rapidly trying to learn English and find employment, which is challenging for refugees with limited or different educational backgrounds or job skills. Thus, many refugees work in low-wage jobs with limited hours, benefits, and job security (Haines, 2010). In 2007, the average household income for refugee families who had been in the U.S. for two to seven years was about $23,000 per year (Office of Refugee Resettlement, 2008). The current sociopolitical climate has further exacerbated refugees’ psychological distress, particularly those from Africa and the Middle East, who have faced growing legal and social discrimination and marginalization based on their race, religion, culture, and country of origin (Alemi & Stempel, 2018; Edge & Newbold, 2013; Nakash, Nagar, Shoshani, Zubida, & Harper, 2012). Although all of these post-migration stressors negatively impact refugees’ mental health, it is also important to consider how they can be conversely conceptualized as protective factors (e.g., inclusion and connection to host country’s culture, valuing of and connection to one’s native culture, English proficiency, social support, valued social roles, and access to resources) that can be measured and promoted.
A high proportion of refugees experiencing distress do not seek mental health services (Weine et al., 2000). Reasons for this include lack of familiarity with Western treatments; prioritizing practical help because of resettlement stressors causing distress (e.g., unemployment, poverty, family dislocation); stigma; and lack of trust (Behnia, 2003; Weine et al., 2000). Thus, there is a need to reach refugees soon after they resettle with universal, non-stigmatizing interventions that reduce post-migration stressors and strengthen protective factors.
RWP Intervention
The Refugee Well-being Project (RWP) intervention involves a sustainable and replicable partnership model between refugees, community organizations, and universities (see Figure 1 for conceptual model). Refugee families and undergraduate advocates were paired to work together for six months to: a) increase refugees’ ability to navigate their new communities; b) improve refugees’ access to community resources; c) enhance meaningful social roles by valuing refugees’ cultures, experiences, and knowledge; d) reduce refugees’ social isolation; and e) increase communities’ responsiveness to refugees. The RWP intervention was implemented by university students enrolled in a two-semester service learning course, and had two elements: 1) Learning Circles, which involved cultural exchange and one-on-one learning opportunities, and; 2) Advocacy, which involved collaborative efforts to mobilize community resources related to health, housing, employment, education, and legal issues and to create policy/system changes.
Figure 1.

Refuge Well-being Project (RWP) Conceptual Model
Meeting together in weekly Learning Circles, refugees and their student partners learned from each other during cultural exchange time designed to facilitate the sharing of cultural and intergenerational knowledge and to help refugees recognize their personal contributions and their potential to effect changes in their communities. During one-on-one learning time, refugee and student participants practiced English, filled out job applications, and engaged in other activities refugees wanted to pursue to expand knowledge, improve skills, or accomplish goals. Students received ten weeks of intensive preparation in the classroom and weekly supervision and close support during the six months of learning and advocacy. A strength of RWP is that it utilized the natural resource of university students who benefit from community-based learning opportunities and have time through the course to develop relationships that facilitate transformative change.
Several important aspects of the RWP intervention are that it is holistic, multilevel, and strengths-based, and has an explicit social justice orientation that is informed by an ecological perspective. A holistic intervention is essential because it addresses the multiple sources of refugees’ psychological distress, including psychological (past traumas), material (poverty, lack of access to resources), physical (lingering physical ailments from war, violence and deprivation experienced in conflict situations), social (loss of meaningful social roles and social support), educational (limited English proficiency, literacy), and cultural (disconnection from traditional cultural practices). A strengths-based perspective is important because refugees have survived in the face of tremendous hardships and have numerous strengths on which to build, including cultural knowledge (of their own culture and often extensive cross-cultural experience), resourcefulness (experience operating in resource scarce situations), effective coping strategies (that have enabled them to survive and successfully resettle), multilingual abilities (many arrive already speaking two or more languages), and often strong family and community bonds and support. Refugees are often pathologized by well-intentioned service providers and systems, rather than recognizing that most are resilient people who have faced abnormally difficult circumstances. Not only is it crucial for refugees’ mental health and well-being to acknowledge their expertise and build upon their strengths, but also their knowledge, experiences, and strengths are assets and knowledge from which other Americans can benefit. Thus, mutual learning is an intentional and core component of RWP. This emphasis also ensures that RWP is appropriate for multiple linguistic and cultural groups who can participate simultaneously and learn from one another as well as from longer-term residents of the United States.
An ecological perspective focuses on multiple levels of context, including microsystem (e.g., family, school, work settings), ecosystem (e.g., other formal and informal social structures), and macrosystem (e.g., political, legal, economic and other social systems) that impact an individual’s health and development, with emphasis on improving the fit between individuals and their environments. Thus, RWP focuses not only on refugees adjusting to their environment, but also on changing environments when they are inequitable or constraining (e.g., mobilization or redistribution of resources). Ensuring that the intervention creates change at multiple levels is important because refugees have urgent learning, resource, and health needs that must be addressed at the individual level in order to enable them to work collectively with other Americans to create community and system-level changes that address the root causes of mental health disparities and social inequities, which result in sustainable social change.
The RWP intervention was first developed and implemented in 2000–2001 by academic and community partners in Michigan (Goodkind, Hang, & Yang, 2004), and adapted and implemented six additional years by academic and community partners in New Mexico (Goodkind, Githinji, & Isakson, 2011) before collaboratively developing an RCT design and acquiring funding from the National Institutes of Health in 2013. Initial pilot testing of the RWP demonstrated feasibility, appropriateness, acceptability, and preliminary evidence that the intervention decreased Hmong, African, and Iraqi participants’ psychological distress and increased protective factors (Goodkind, 2005; 2006; Goodkind et al., 2014). Findings also indicated that students engaged in mutual learning with their refugee partners (Goodkind, 2006) and that the RWP fostered transformative learning experiences through which refugees’ and students’ critical awareness was increased, which provided an impetus to work toward social change at multiple levels (Hess et al., 2014). For a more detailed description of the RWP intervention, see Goodkind (2005) and Goodkind, Githinji, & Isakson (2011).
Method
Study Objectives and Design
As a community-based participatory research project designed to better understand resettlement stressors, prevent psychological distress, and promote mental health, well-being, and integration of refugees, the overall objective of the RWP was to make U.S. communities and health, legal, social service, and other systems more welcoming, equitable, and responsive to the needs and goals of refugees. The aim of the RCT of the RWP intervention was to demonstrate that addressing social determinants of mental health through a social justice approach contributes to improved mental health for refugees. The RCT was funded by the National Institute of Minority Health and Health Disparities (R01MD007712) and approved by the University of New Mexico’s Human Research Protections Office. The mixed method RCT employed a longitudinal randomized waitlist control group design with 4 data collection points over 12 months.
A convergent parallel mixed methods design was used to guide collection and analysis of quantitative and qualitative data; this paper involves multilevel modeling of the quantitative data. The sample size of 143 households, each with an average of 2 adult participants, provided .80 power to detect small-to-medium differences in post-intervention intercept or slope of change over time (d = 0.25) at 2-tailed p < .05, using 3-level multilevel modeling (4 time points at level 1, individuals within households at level 2, and households at level 3) with randomization at level 3. Optimal Design software was used for power estimation (Spybrook, et al., 2011).
Participants
A total of 290 refugee adults from 143 households were enrolled in the study in a series of four cohorts from October 2013 to November 2016 in a mid-sized city in the Southwestern United States. About equal numbers of participants were from each of three main regions: 36.2% Afghan,2 32.8% Iraqi and Syrian,3 and 31.0% Great Lakes African,4 and 52% were women. More than half (58%) were married, with 33% single, 7% widowed, and 2% divorced. Participants’ ages ranged from 18 to 71, with a mean age of 34.6. At the first interview time point, participants had been in the U.S. an average of 30 weeks. Almost half (49%) had not finished high school, 19% were high school graduates, and 31% reported having completed some post-secondary education. Most participants (70.3%) had children, with an average of 2.3 children and a range of 0 to 9. See Table 1 for additional demographic information.
Table 1.
Study Participant Demographics by Condition
| Control Group | Intervention Group | Total | ||
|---|---|---|---|---|
| Nationality | # (%) | # (%) | # (%) | |
| Iraqi/Syrian | 50 (53%) | 45 (47%) | 95 (33%) | |
| Afghan | 65 (62%) | 40 (38%) | 105 (36%) | |
| Great Lakes African | 56 (62%) | 34 (38%) | 90 (31%) | |
| Gender | ||||
| Male | 81 (59%) | 57 (41%) | 138 (48%) | |
| Female | 90 (59%) | 62 (41%) | 152 (52%) | |
| Spent Time in a Refugee Camp | ||||
| Yes | 56 (57%) | 42 (43%) | 98 (34%) | |
| No | 115 (60%) | 77 (40%) | 192 (66%) | |
| Marital Status | ||||
| Single | 60 (63%) | 36 (38%) | 96 (33%) | |
| Married | 100 (59%) | 69 (41%) | 169 (58%) | |
| Divorced | 1 (17%) | 5 (83%) | 5 (2%) | |
| Widowed | 10 (53%) | 9 (47%) | 19 (7%) | |
| Other Descriptives | Mean (SD) | Mean (SD) | Mean (SD) | |
| Age | 33.51 (10.73) | 36.18 (12.47) | 34.60 (11.53) | |
| # of People in Household | 5.31 (2.22) | 4.58 (2.09) | 5.01 (2.20) | |
| # of Children in Household | 2.30 (2.27) | 2.24 (2.22) | 2.27 (2.25) | |
| Years of Education | 9.82 (5.42) | 10.34 (5.62) | 10.03 (5.50) | |
| Weeks in United States | 27.29 (26.39) | 33.68 (29.80) | 29.91 (27.97) | |
Procedures
Recruitment.
All refugees 18 and older from Afghanistan, the Great Lakes Region of Africa, Iraq and Syria who had arrived in the U.S. within the past three years and were living in the city where the study took place were invited to participate. Bilingual/bicultural research team members from the three regions contacted all refugee households, based on complete lists of refugees resettled each year that were compiled in coordination with the two refugee resettlement organizations in the city and on community networks developed since the RWP began in 2006. Team members called and arranged a meeting with each household to explain the study and obtain informed consent. Each adult in the household could make an independent decision about study participation; a household was only considered to have refused participation if no adults from the household agreed to participate. Of 161 households contacted, 143 (88.8%) agreed to participate in the study; 17 households were not interested in participating, and one household was ineligible because the one adult in the household was unavailable at the time the intervention would be held. No households were excluded due to severe cognitive functioning problems, or mental or physical illness that was so severe as to impede participation in a group. See Figure 2 for details of household and individual refusal and ineligibility and participant flow.
Figure 2.
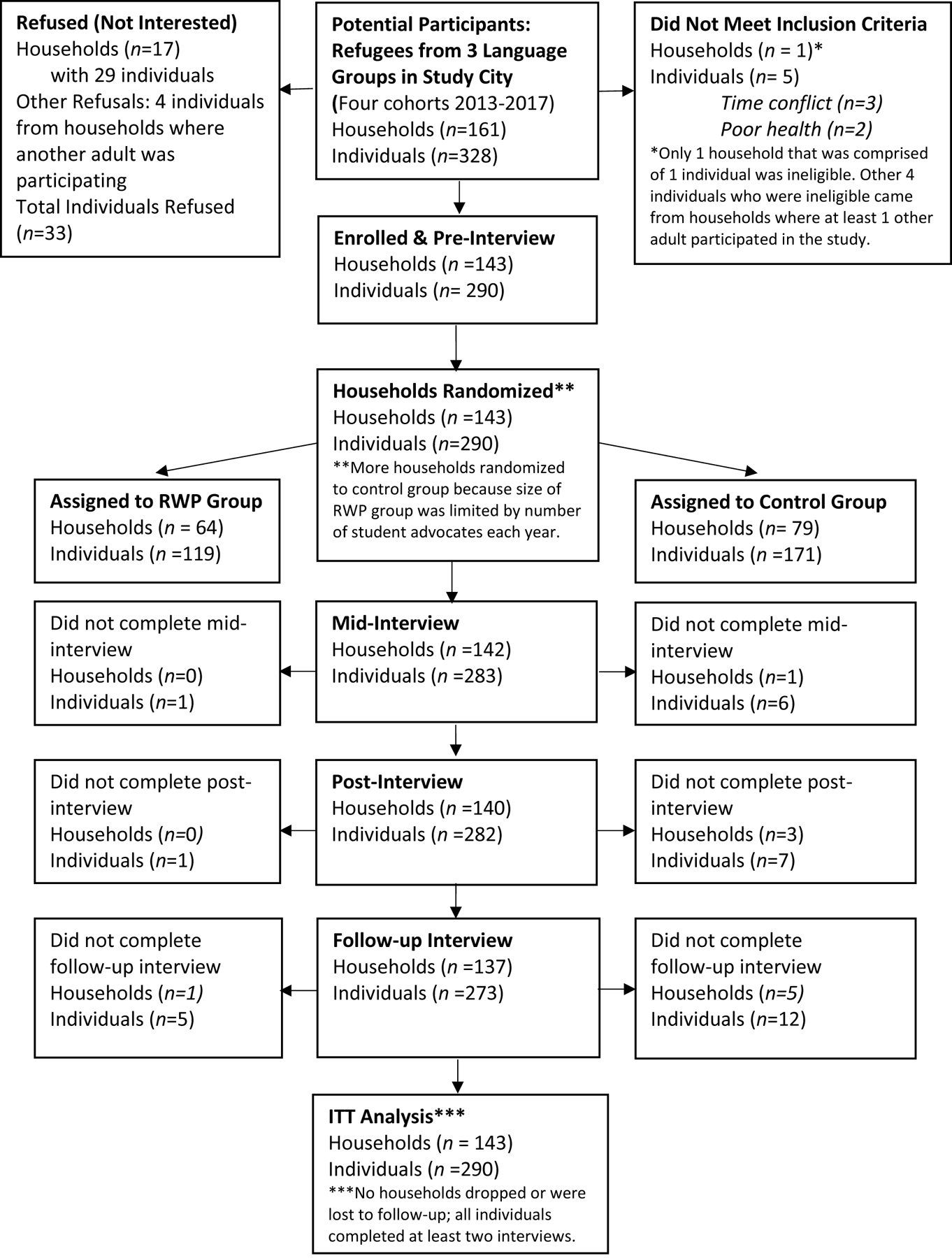
Consolidated Standards of Reporting Trials (CONSORT) diagram showing flow of participants through the trial. RWP = Refugee Well-being Project intervention; ITT = intention to treat.
Randomization strategy.
Participants were randomized at the household level into intervention and waitlist control groups. To address concerns of mistrust, the study’s community advisory council decided that random assignment should occur at a public meeting, to which all participants were invited. After completion of all pre-interviews for each cohort, household ID numbers were placed into a box. ID numbers were color-coded by two stratification variables (3 national/regional origin groups and absence or presence of clinically significant PTSD symptom score of at least one adult in the household to ensure that households with more serious distress were distributed evenly in intervention and control groups). Randomization meetings were held at a local community center; all study participants were informed of the time and location and transportation was provided, if needed. At randomization meetings, interpreters were present and the process of selecting ID numbers was explained. In addition to the benefit of participants being able to observe that the process was unbiased, another advantage of this approach was that research staff could meet with participants after randomization to explain their group assignment and make plans for the first Learning Circle for those in the RWP intervention group (hereafter RWP group) or the stress management session for those in the waitlist control group (61 of 172 participants in the waitlist control group elected to attend the stress management session).
Intervention implementation.
Refugee households assigned to the RWP group were matched with 1–3 student advocates, depending upon the number of people in the household aged 5 and above (1–3 people = 1 advocate, 4–6 people = 2 advocates, 7 or more people = 3 advocates). They participated in weekly 2-hour Learning Circles for six months (described previously) and student advocates devoted an additional 4 or more hours per week to working with their refugee partners on advocacy activities as defined by the unmet needs and goals of the refugee participants. Participants in the control group were invited to attend a stress management session and to participate in RWP after all time points of data collection were complete. In-person interpretation was provided at Learning Circles and stress management sessions.
Data collection.
Each refugee participant completed 4 interviews over a period of 12 months: pre, mid, and post (spaced 3 months apart) and a 6-month post-intervention follow-up. Quantitative data were collected via computer-assisted personal interviews at each participant’s home with a bilingual/ bicultural interviewer in the participant’s native language. Pre-interviews also included a qualitative semi-structured component for all participants, and a subset of participants (n=66) completed a qualitative semi-structured component at mid, post, and follow-up time points. Participants received gift cards to compensate for their time completing the interviews ($20 for pre, $30 for mid, $40 for post, $50 for follow-up). To ensure fidelity of intervention implementation, extensive process data was collected, including weekly progress reports and logbooks from undergraduate advocates, observations of Learning Circles, and interviews with student-refugee dyads to explore their experiences working together.
Measures
All measures used in the study have a history of successful implementation with refugees and culturally diverse populations. Measures were translated and back-translated from English into Arabic, Dari, French, Kiswahili, and Pashto using the TRAPD (Translation, Review, Adjudication, Pretesting, and Documentation) process (Survey Research Center, 2016).
Acculturation.
Because connection to one’s native culture and to one’s host country have both been found to be protective for refugee mental health, we included measures of Home (refugee’s native culture) and American acculturation. These constructs were measured by modified, parallel versions of the Language, Identity and Behavior (LIB) Acculturation Scale (Birman, Trickett, & Vinokurov, 2002). Each scale was comprised of 8 items that assessed multiple dimensions of acculturation (e.g., “How much do you eat American [or Iraqi] food? How much do you know about American [or Afghan] culture?”). Likert-type responses ranged from 0=“not at all” to 3=“very much.” Cronbach’s alphas at each time point for Home acculturation and American acculturation ranged from .75–.84 and .76–.82, respectively.
English proficiency.
Perceived English Proficiency (PEP) was measured by the mean of four items that asked participants to rate how well they understand, speak, read, and write English. Response choices ranged from 0=“not at all” to 3=“like a native” (Rumbaut, 1989). Cronbach’s alphas at the four time points ranged from .92–.93. PEP is highly correlated with objective measures of English proficiency (Rumbaut, 1989).
Social support.
The Multi-Sector Social Support Inventory Scale (MSSSI; Layne et al., 2009) measured three types of perceived social support, which are typically salient for refugees: family, ethnic community, and non-ethnic community throughout the past month. Each of the three parallel scales included the same 9 items related to subjective attachment (e.g., I feel like I “fit in” and belong with the members of the African community) and perceived support from other community members (e.g., I can count on members of my family if I need help). Response choices ranged from 0=“never” to 4=“almost always.” Higher scores reflect greater perceived social support. Cronbach’s alphas for family, ethnic community, and non-ethnic community social support ranged from .85–.89, .91–.93, and .88–.90, respectively.
Emotional distress.
The Hopkins Symptom Checklist (HSC-25) is a self-report measure of anxiety and depression symptoms that has been used repeatedly with populations throughout the world, including refugees (Ichikawa, Nakahara, & Wakai, 2006; Mollica, Wyshak, de Marneffe, Khuon, & Lavelle, 1987) and was rated by Hollifield and colleagues (2002) in their review of mental health measures for refugees as one of only two instruments to meet all five of their established criteria. Response choices for each item are on a Likert-type scale ranging from 1 (not at all) to 4 (extremely). The HSC-25 produces three scores: total (mean of all 25 items), depression (mean of the 15 depression items), and anxiety (mean of the 10 anxiety items). It has been consistently shown in multiple populations that the total score is highly correlated with severe emotional distress of unspecified diagnosis, and that the depression score is correlated with major depression as defined by the Diagnostic and Statistical Manual of the American Psychiatric Association, IV Version (DSM-IV). We removed one item from the depression scale (“loss of sexual interest or pleasure”) because bicultural team members found this question to be culturally inappropriate and too intrusive. We used the total score (mean of all 24 items) and the two subscales. Participants’ total scores at the pre-interview ranged from 1.00 to 3.67, with M = 1.50, SD = 0.60. A score above 1.75 suggests clinically significant distress; 22.1% of participants had scores above this cutoff at the pre timepoint. Cronbach’s alphas ranged from .96–.97.
Pre-intervention household-level means and standard deviations for all outcome measures are summarized in Table 2 by nationality and condition. Because emotional distress outcomes had substantial positive skew, log-transformations of these variables were used for analysis. Both original and transformed variables are presented. Although there were no significant condition differences at baseline or Nationality × Condition interactions, households from different nationalities varied significantly on nearly all measures at baseline. Two exceptions were social support from family, which was uniformly high, and social support from the non-ethnic community, which was generally low. Ethnic community social support was significantly higher among Afghans, compared with both Iraqis and Africans. American acculturation was higher for Africans than for Iraqis, while Afghans had the highest home acculturation. English proficiency was higher for Iraqis than for Africans. Emotional distress symptoms were significantly higher for Iraqis in comparison with both Afghans and Africans. Table 3 contains pre-intervention correlations among the outcome variables. Correlations were generally low, except for those among the three emotional distress symptom measures. There were also substantial correlations among home acculturation and social support from both family and ethnic community.
Table 2.
Pre-intervention Household Means on Outcome Measures (M, SD), by Nationality and by Condition
| Nationality | Condition | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Iraqi | Afghan | African | Statistical comparison | RWP | Cntrl | Statistical comparison | |||
| Outcome variables | n = 51 | n = 53 | n = 39 | F(2, 137) | p | n= 64 | n=79 | F(1, 137) | p |
| American acculturation | 10.82a | 11.88 | 13.94b | 6.52 | 0.002 | 12.39 | 11.8 | 0.63 | 0.43 |
| 3.87 | 4.24 | 3.24 | 3.91 | 4.12 | |||||
| Home acculturation | 18.74a | 20.08b | 17.67a | 136.02 | 0.002 | 18.82 | 19.05 | 0.26 | 0.61 |
| 3.38 | 2.55 | 3.79 | 3.77 | 2.98 | |||||
| Perceived English proficiency | 1.23a | 1.02 | 0.93b | 3.76 | 0.03 | 1.04 | 1.1 | 0.75 | 0.39 |
| 0.58 | 0.61 | 0.46 | 0.57 | 0.57 | |||||
| Social support from family | 2.89 | 3.01 | 2.76 | 1.18 | 0.31 | 2.86 | 2.93 | 0.39 | 0.53 |
| 0.74 | 0.78 | 0.81 | 0.83 | 0.73 | |||||
| Social support from ethnic | 1.56a | 1.99b | 1.57a | 4.27 | 0.02 | 1.65 | 1.78 | 0.82 | 0.37 |
| 0.8 | 0.92 | 0.72 | 0.88 | 0.82 | |||||
| Social support from non-ethnic | 1.09 | 0.99 | 1.16 | 0.46 | 0.63 | 1.07 | 1.07 | 0.02 | 0.90 |
| 0.71 | 0.69 | 0.63 | 0.65 | 0.71 | |||||
| cEmotional distress (raw score) | 1.83 | 1.45 | 1.39 | ---- | ---- | 1.67 | 1.49 | ---- | ---- |
| 0.63 | 0.46 | 0.46 | 0.62 | 0.49 | |||||
| cEmotional distress (natural log) | 0.54a | 0.32b | 0.28b | 10.21 | <.001 | 0.44 | 0.34 | 3.23 | 0.07 |
| 0.33 | 0.27 | 0.26 | 0.34 | 0.27 | |||||
| cAnxiety subscale (raw score) | 1.76 | 1.41 | 1.35 | ---- | ---- | 1.63 | 1.43 | ---- | ---- |
| 0.63 | 0.48 | 0.47 | 0.64 | 0.48 | |||||
| cAnxiety subscale (natural log) | 0.49a | 0.29b | 0.24b | 8.62 | <.001 | 0.41 | 0.3 | 3.77 | 0.06 |
| 0.34 | 0.27 | 0.26 | 0.35 | 0.27 | |||||
| cDepression subscale (raw score) | 1.89 | 1.49 | 1.42 | ---- | ---- | 1.71 | 1.54 | ---- | ---- |
| 0.64 | 0.47 | 0.46 | 0.61 | 0.53 | |||||
| cDepression subscale (natural log) | 0.56a | 0.35b | 0.30b | 10.16 | <.001 | 0.47 | 0.37 | 3.43 | 0.07 |
| 0.33 | 0.26 | 0.26 | 0.33 | 0.29 | |||||
Note: RWP = Refugee Well-being Project intervention condition; Cntrl = Control condition. Nationality × Condition interactions were not significant for any outcome variable and are therefore not presented.
Cell means with different letter subscripts are significantly different at p < .05 according to Tukey post hoc tests.
Emotional distress symptom scores were log-transformed to reduce positive skew; raw score means are presented to aid interpretation and are not used in comparative analyses.
Table 3.
Correlations Among Outcome Variables at Pre-Intervention (N = 143 Household Means)
| American acculturation | Home acculturation | English proficiency | Social support -family | Social support -ethnic | Social support non-ethnic | Emotional distress | Anxiety | Depression | |
|---|---|---|---|---|---|---|---|---|---|
| American acculturation | 1.00 | ||||||||
| Home acculturation | −0.28 | 1.00 | |||||||
| English proficiency | 0.27 | −0.16 | 1.00 | ||||||
| Social support - family | −0.13 | 0.31 | 0.10 | 1.00 | |||||
| Social support - ethnic | −0.14 | 0.59 | −0.12 | 0.42 | 1.00 | ||||
| Social support - non-ethnic | 0.37 | −0.03 | 0.21 | 0.12 | 0.18 | 1.00 | |||
| Emotional distress (natural log) | −0.19 | −0.03 | −0.03 | −0.18 | −0.04 | 0.05 | 1.00 | ||
| Anxiety (natural log) | −0.18 | −0.02 | −0.01 | −0.14 | −0.01 | 0.10 | 0.96 | 1.00 | |
| Depression (natural log) | −0.18 | −0.03 | −0.03 | −0.20 | −0.06 | 0.04 | 0.98 | 0.88 | 1.00 |
Note: Correlations larger than .17 are significant at p < .05.
Data Analytic Strategy
Multilevel growth modeling (Hedeker & Gibbons, 2006; S Raudenbush, Bryk, & Congdon, 2002) was the primary analytic approach used to examine effects of the intervention on changes in outcomes over time through 6-month follow-up. Because all individuals in a household were randomly assigned as a unit to either the RWP or control conditions, household was specified at level 3, adults nested within households were at level 2, and time of assessment (pre, mid, post, 6-month follow-up) was nested within each adult at level 1. Most households (98 of 143) had multiple adults, providing sufficient variance for estimation of within-household variance across the sample. As household was the level of randomization, intervention condition (RWP vs control) was entered as a dichotomous variable at level 3. Because households were blocked on nationality prior to randomization, nationality was included in all analyses at level 3.
The significance of the interaction between nationality and condition was tested for each model and retained if it improved model fit. Time was centered at 6-month follow-up, to provide a straightforward estimate of effects at the final assessment point; secondary analyses centered time at post-intervention to estimate condition differences at this point (Singer & Willett, 2003). To optimize precision, all models included the baseline observation of the dependent variable for each individual at level 2. Each model contained up to four random effects, allowing (a) intercept or level of outcome to vary among adults within each household, (b) average intercepts (levels) to vary among households, (c) time slopes to vary among adults within households, and (d) average time slopes to vary among households; effects showing no significant random variance in nonconditional null models were fixed in subsequent analyses. All other parameters were estimated as fixed effects. HLM7 software (Raudenbush et al., 2002) was used for the analysis, with full information maximum likelihood (FIML) estimation of parameters, to allow for testing of nested models. Robust standard errors were used to compute p values and confidence intervals, optimizing accuracy for moderate nonnormality. Effect sizes (d) were computed for each effect, using pre-intervention pooled standard deviations in the denominator for intercept effects and null longitudinal model time variances for slope effects (Feingold, 2009; Raudenbush & Liu, 2001). Effect sizes were referred to by the standard benchmarks of “small (d = .20),” “medium (d = .50),” and “large (d = .80)” proposed by Cohen (1988). Confidence intervals around each d were computed using methods developed by Feingold (2015). The significance of interaction effects was tested using likelihood ratio chi square tests to compare nested models. For interaction effects found to significantly improve model fit, simple slopes were computed using methods developed by Preacher, Curran, and Bauer (2006).
All analyses were on the full intent-to-treat sample. Of the total possible 1,160 interviews across four timepoints, 32 (2.8%) could not be conducted. Including data missing due to missed interviews and skipped items, 2.0% of the data matrix was missing, apparently completely at random (Little’s MCAR χ2 (df = 67378) = 37630.71, p = 1.00). For outcome analyses, missing values were handled in two ways, through expectation maximization (EM) and FIML estimation (Enders, 2010); results were virtually identical, and EM estimated results are reported.
Results
Intervention Participation
Of the 119 individuals in households randomly assigned to the RWP, all but 3 attended at least one Learning Circle and all but 2 had at least 2 hours of face-to-face contact with their advocate. Across individuals, mean hours of face-to-face contact with advocates was 72.11 (SD = 48.63; Mdn = 66.00); mean number of Learning Circles attended was 12.00 (SD = 5.88; Mdn = 12.00). Most participants (79.1%) attended at least 9 Learning Circles (half of those scheduled). See Table 4 for additional details of RWP participation.
Table 4.
RWP Participation – Learning Circles Attended and Contact with Advocates
| Individual participants (N = 119) | Household average (N = 64) | |||||
|---|---|---|---|---|---|---|
| Number of Learning Circles attended | Number of Participants | Cumulative % | Number of Households | Cumulative % | ||
| % | % | |||||
| 0 | 3 | 2.5 | 2.5 | 0 | 0 | 0.0 |
| 1 – 4 | 14 | 11.7 | 14.3 | 7 | 10.9 | 10.9 |
| 5 – 9 | 21 | 17.6 | 31.9 | 10 | 15.6 | 28.1 |
| 10 – 13 | 27 | 22.7 | 54.6 | 22 | 34.4 | 60.9 |
| 14 – 17 | 31 | 26.1 | 80.7 | 18 | 28.1 | 89.1 |
| 18 – 23 | 23 | 19.3 | 100.0 | 7 | 10.9 | 100 |
| Hours face-to-face with advocate | ||||||
| 0 | 2 | 1.7 | 1.7 | 0 | 0.0 | 0.0 |
| 1 – 18 | 14 | 11.8 | 13.5 | 6 | 7.8 | 7.8 |
| 19 – 54 | 26 | 21.8 | 35.3 | 14 | 21.9 | 29.7 |
| 55 – 72 | 26 | 21.8 | 57.1 | 18 | 28.1 | 53.1 |
| 73 – 90 | 22 | 18.5 | 75.6 | 12 | 18.8 | 76.6 |
| 91 – 144 | 20 | 16.8 | 92.4 | 10 | 15.6 | 92.2 |
| 145 – 242 | 9 | 7.6 | 100.0 | 5 | 7.8 | 100.0 |
Intervention Outcomes
Table 5 presents results of 3-level multilevel models examining comparisons between the RWP and control groups to which households were randomly assigned. The first set of columns contains the gamma coefficients and associated p values, effect sizes, and 95% confidence intervals for RWP effects at 6-month follow-up, which was defined as the intercept. The second set of columns contains the coefficients for the RWP effects on the linear time slopes. Figures 3 through 7 contain model plots that illustrate the effects of RWP within each nationality group.
Table 5.
3-level Multilevel Models of Outcomes Regressed on Time, RWP Intervention, and Nationality
| RWP effect at 6-month follow-up | RWP effect on linear slope | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | |||||||||
| Outcome variables | gamma | p | d | LCL | UCL | gamma | p | d | LCL | UCL |
| American acculturation | 1.09 | 0.07 | 0.27 | −0.02 | 0.57 | 0.154 | 0.02 | 1.03 | 0.19 | 1.86 |
| Home acculturation | 1.04 | 0.05 | 0.31 | 0.01 | 0.62 | 0.148 | 0.03 | 0.55 | 0.07 | 1.03 |
| aPerceived English proficiency | 0.11 | 0.03 | 0.19 | 0.02 | 0.53 | 0.001 | 0.95 | 0.04 | −0.90 | 1.00 |
| Social support from family | 0.09 | 0.33 | 0.11 | −0.13 | 0.36 | 0.011 | 0.37 | 0.28 | −0.31 | 0.86 |
| Social support from ethnic community | 0.01 | 0.90 | 0.01 | −0.27 | 0.29 | 0.017 | 0.28 | 0.43 | −0.36 | 1.21 |
| bSocial support from non-ethnic community | 0.06 | 0.57 | 0.09 | −0.22 | 0.39 | −0.141 | 0.01 | ----- | ----- | ----- |
| cEmotional distress symptoms (simple effects of RWP within each nationality due to significant RWP × Nationality interactions) | ||||||||||
| Emotional distress -- Iraqi | −0.12 | 0.01 | −0.39 | −0.70 | −0.09 | −0.004 | 0.48 | −0.20 | −0.80 | 0.40 |
| Emotional distress -- Afghan | −0.05 | 0.33 | −0.16 | −0.86 | 0.16 | −0.013 | 0.05 | −0.65 | −1.25 | −0.05 |
| Emotional distress -- African | −0.02 | 0.84 | −0.05 | −0.55 | 0.45 | −0.003 | 0.77 | −0.15 | −1.05 | 0.60 |
| Anxiety subscale -- Iraqi | −0.11 | 0.04 | −0.34 | −1.01 | −0.02 | −0.003 | 0.66 | −0.15 | −0.85 | 0.55 |
| Anxiety subscale -- Afghan | −0.08 | 0.14 | −0.25 | −0.59 | 0.08 | −0.016 | 0.01 | −0.80 | −1.50 | −0.20 |
| Anxiety subscale -- African | 0.00 | 0.97 | −0.01 | −0.52 | 0.50 | −0.007 | 0.50 | −0.35 | −1.35 | 0.65 |
| Depression subscale -- Iraqi | −0.14 | 0.01 | −0.45 | −0.76 | −0.14 | −0.006 | 0.33 | −0.30 | −0.90 | 0.30 |
| Depression subscale -- Afghan | −0.03 | 0.55 | −0.11 | −0.46 | 0.25 | −0.008 | 0.20 | −0.40 | −1.00 | 0.20 |
| Depression subscale -- African | −0.04 | 0.63 | −0.11 | −0.34 | 0.11 | −0.001 | 0.89 | −0.05 | −0.10 | 0.85 |
Note. N = 290 adult participants in 143 households. All models controlled for nationality (Iraqi vs. Afghan and African vs. Afghan) and the pre-intervention level of the dependent variable. Intervention effects significant at p < .05 are bolded.
For perceived English proficiency, RWP effects were also significant at post-intervention, gamma = .11, p = .004, d = .18, CI = .06, .31.
For support from non-ethnic community, RWP effects were significant at post-intervention, gamma = .41, p < .001, d = .60, CI = .27, .92. RWP effects were also significant on the quadratic slope, gamma = −.01, p = .01. No overall effect size can be computed for a nonlinear slope.
For emotional distress symptoms, model fit comparison with and without RWP × Nationality interactions: Emotional Distress, LR chi square(df = 4) = 9.49, p < .05; Anxiety, LR chi square(df = 4) = 9.69, p < .05; Depression, LR chi square(df = 4) = 8.33, p = .08.
Figure 3.

American acculturation over time, by condition and nationality
Figure 7.
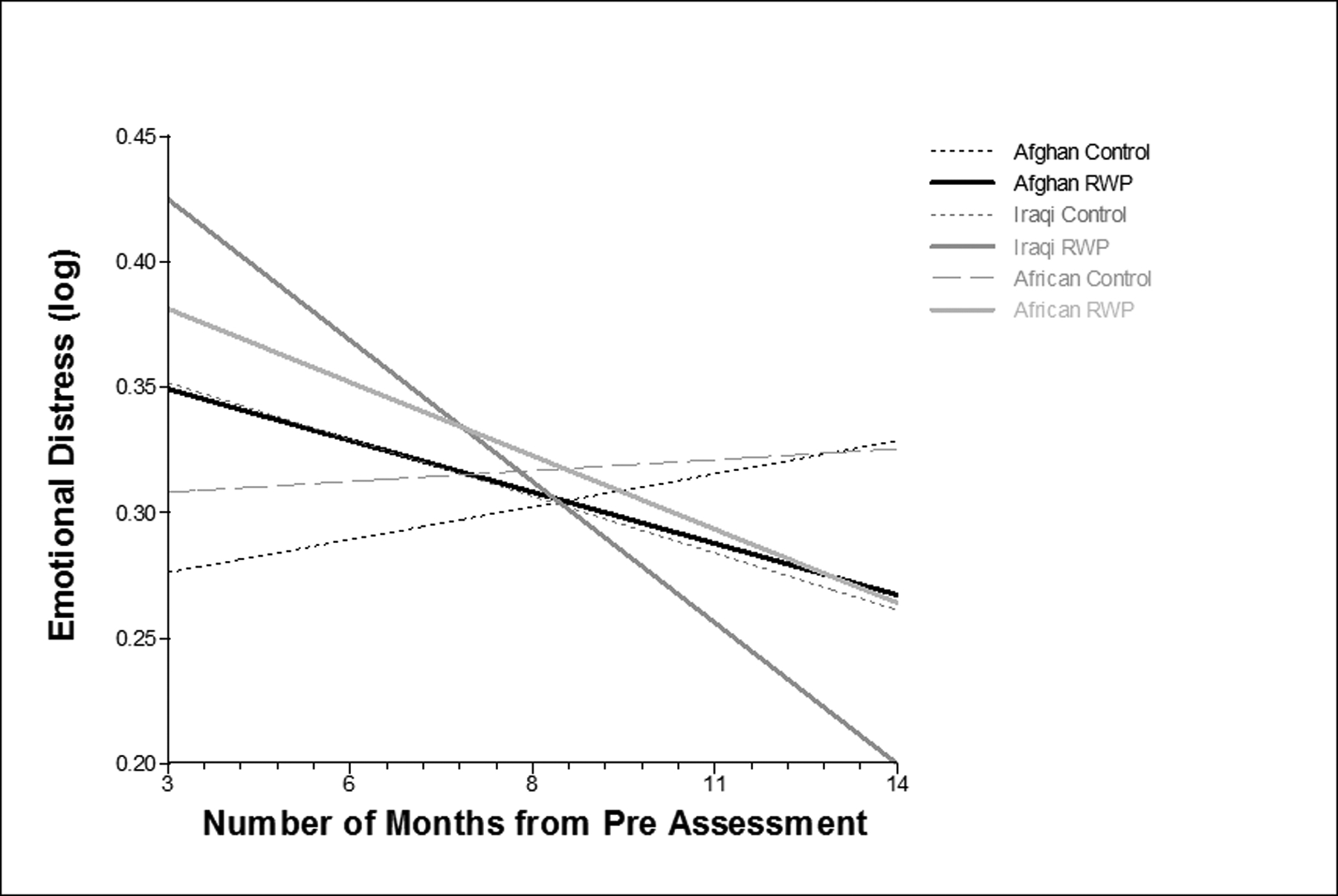
Emotional distress over time, by condition and nationality
Acculturation.
For acculturation to American culture, the RWP condition increased .15 points per month more than the control group during the period from mid-intervention to 6-month follow-up; this increase was statistically significant and reflected a large effect size (d = .88). At 6-months follow-up, the RWP group was 1.09 points higher (d = .27) than the control group, although at p < .07, this difference did not meet conventional criteria for significance. Figure 3 shows that, across all three nationality groups, American acculturation increased for those in RWP, while it declined for those in the control group. Results for acculturation to refugees’ home cultures were similar, with the RWP condition increasing .15 point per month more in comparison with the control group; this was significant and reflected a medium-to-large effect size of d = .67. At 6-months follow-up, the RWP group was 1.04 points higher (d = .31), which was significant at p < .05. Figure 4 shows a pattern similar to that for American acculturation, with acculturation to refugees’ home cultures increasing for those in the RWP condition and declining for those in the control.
Figure 4.

Home acculturation over time, by condition and nationality
English proficiency.
Refugees’ perceived English proficiency was significantly higher at 6-months follow-up for those in RWP in comparison to those in the control group, although the effect was small (d = .19), and the two groups did not differ significantly in their linear change slopes. Figure 5 shows the trajectories for RWP vs control in each of the three nationality groups. English proficiency remained stable over time for Iraqis (who started out significantly higher at the pre-intervention assessment) and improved for Afghans and Africans in both RWP and control. Higher proficiency scores for those in the RWP condition emerged by the mid-intervention assessment and continued through the follow-up period.
Figure 5.
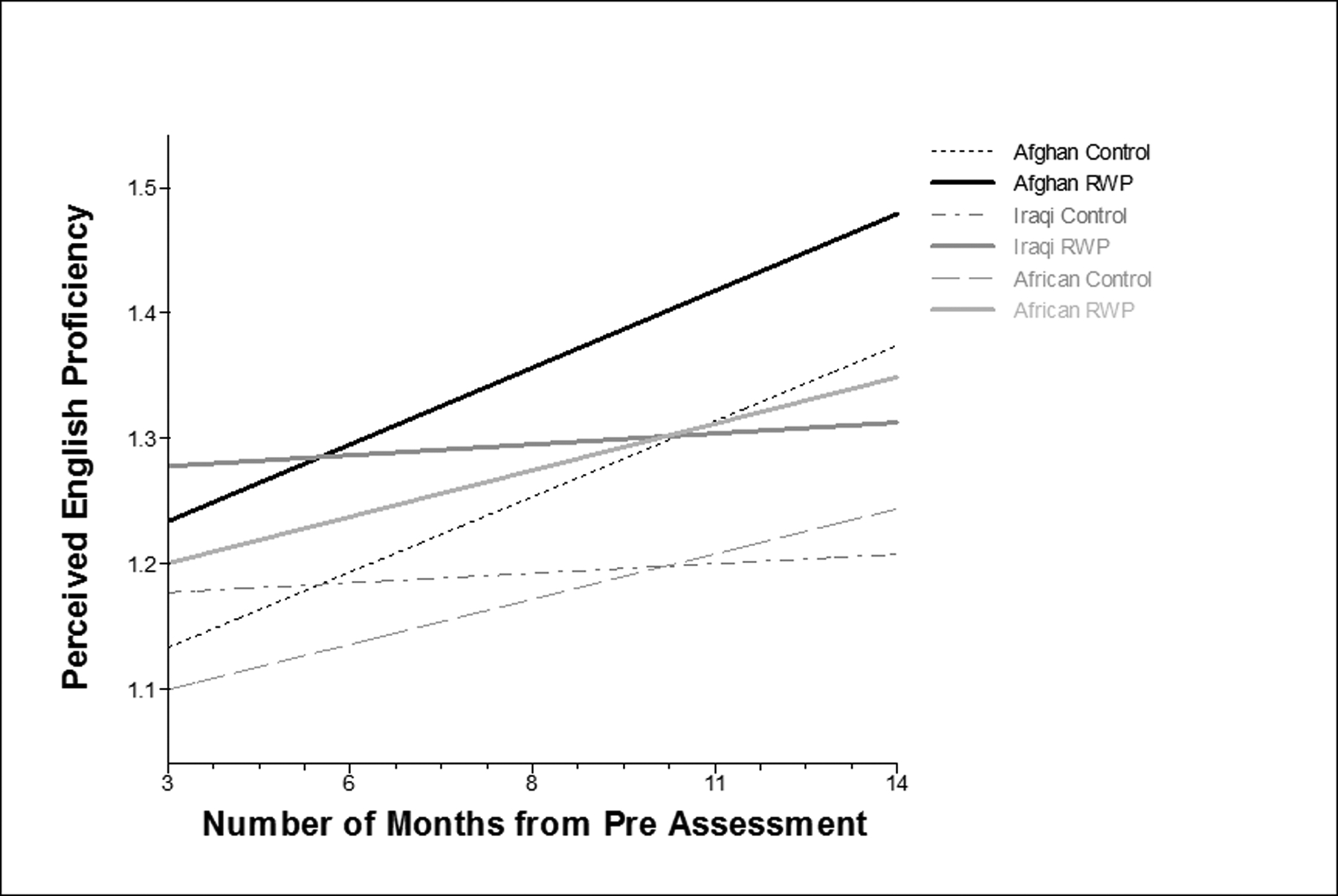
Perceived English proficiency over time, by condition and nationality
Social support.
As expected, there were no condition differences on social support from family or from members of refugees’ own ethnic communities – neither in change over time nor in level at 6-month follow-up. However, there were significant differences in the change trajectories of social support from non-ethnic community members. Change was significantly nonlinear, with a random quadratic term significantly improving model fit (LR X2 (df = 4) = 14.2, p < .01). Intervention effects were significant for both the linear and quadratic elements of the time slope, showing substantially different trajectories for those in the RWP and control groups. At post-intervention, levels of support from non-ethnic community were significantly higher for RWP – .41 points higher than those in the control, p < .001, d = .60, a medium-to-large effect. However, by 6-month follow-up, the difference had declined and was no longer significant. Figure 6 shows the trajectories of support from non-ethnic community members by condition and nationality. Trajectories for those in RWP showed initial increases from mid- to post-intervention assessments, followed by sharp declines from post-intervention to 6-month follow-up. For those in the control condition, support from non-ethnic community declined steadily or remained at very low levels across the time period.
Figure 6.
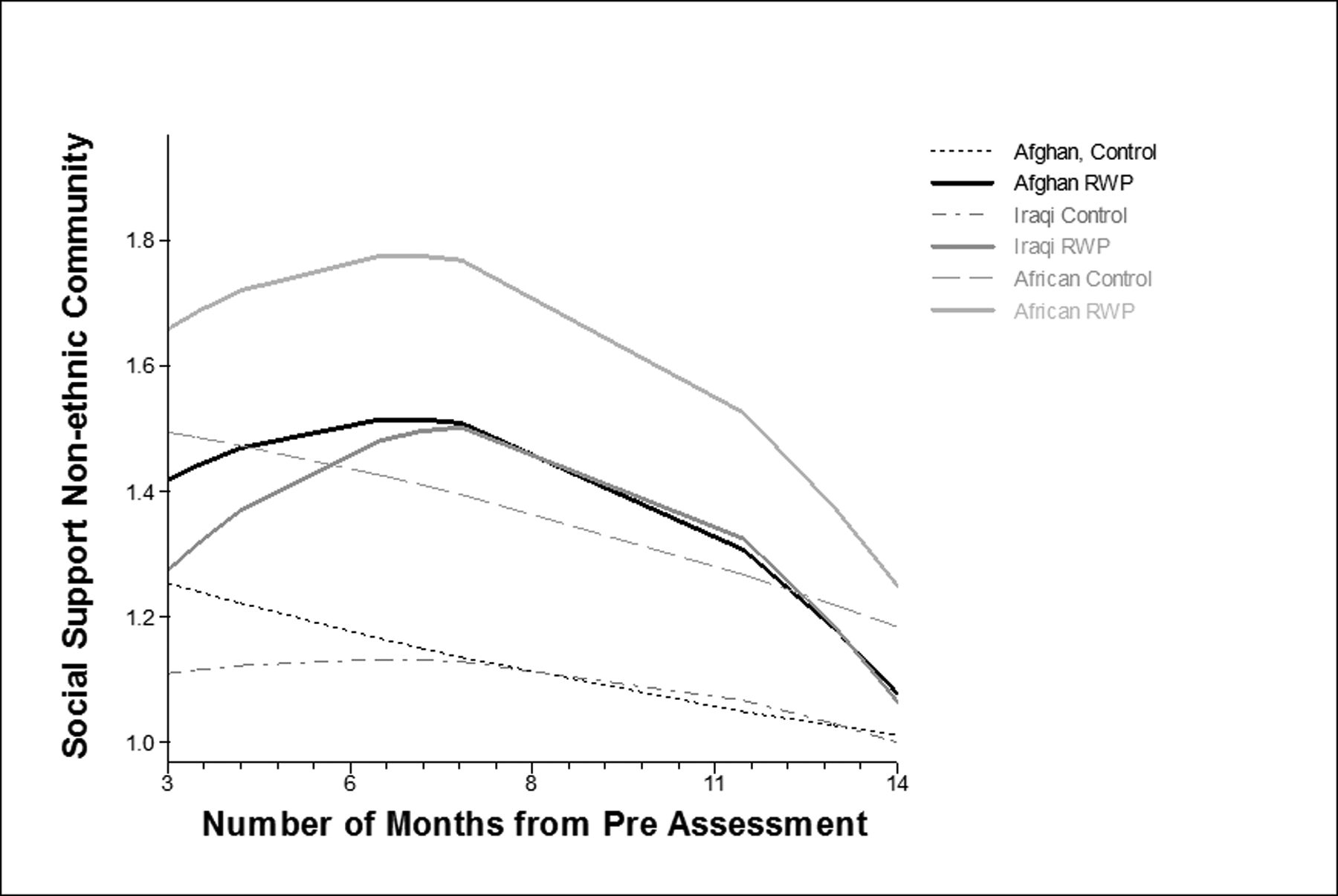
Social support from non-ethnic community over time, by condition and nationality
Emotional distress.
The effect of RWP on emotional distress differed by nationality; the addition of the RWP × nationality interaction significantly improved model fit (LR chi square (df = 4) = 9.49, p < .05). For Iraqis, who started out with significantly higher levels of baseline emotional distress, distress was significantly lower at 6-month follow-up for those assigned to RWP compared with controls (.12 points lower on the log-transformed scale, equivalent to 1.13 points on the original 4-point scale). This reflects a medium effect size of d = −.39. However, the linear slope coefficient was not significant for Iraqis. For Afghans, emotional distress declined more rapidly for those in RWP compared with controls (−.013 points per month on the log-transformed scale, equivalent to −1.01 on the original scale). This reflects a medium-to-large effect of d = −.65). Despite the significant difference in slopes, at 6-months follow-up, the difference between RWP and control among Afghans was not significant. For Africans, both the slope and level coefficients at 6-month follow-up were negative, suggesting lower scores for RWP, but effect sizes were very small and neither coefficient was significant. Figure 7 shows the trajectories of emotional distress by condition and nationality: for all three nationalities, those in RWP appeared to decline more quickly and had lower scores at 6-month follow-up than controls.
Patterns of change for the anxiety subscale of the emotional distress measure showed very similar patterns, with RWP significantly lower than control at 6-month follow-up for Iraqis and significantly greater declines in distress among Afghans and no significant differences among Africans. For the depression subscale, the only significant difference was at 6-month follow-up for Iraqis assigned to RWP compared with controls; although the effect size for the slope comparison among Afghans was medium in size (d = −.40), it was not significant (p = .20).
Discussion
This study makes important contributions to our understanding of the social determinants of mental health for the growing number of refugees resettling outside their countries of origin and the effectiveness of multilevel, social justice approaches to reducing high rates of emotional distress they experience. Although research has documented the impact of post-migration stressors (poverty, lack of access to resources, loss of social support and valued social roles, discrimination/marginalization, limited English proficiency) on refugees’ persisting mental health problems, few studies have rigorously tested interventions that aim to ameliorate these stressors and create change at multiple levels. This paper presents results of an effort to address this gap, and includes promising initial findings from an RCT of the RWP model.
First developed in 2000, the RWP has a long history of community-university partnership and an ongoing CBPR process that has guided the development, adaptations, and implementation of the intervention and the design and conduct of multiple research efforts to explore RWP’s impacts on refugees, university students, and community and system-level change. After many successful years of implementation and positive results from mixed method within-group longitudinal studies, university and community partners decided that an RCT was an important next step to demonstrate the effectiveness of the RWP and to facilitate its dissemination to many other communities and universities who continue to request it. Importantly, this study provides promising evidence that addressing social determinants of mental health from a strengths-based, holistic approach that aims for multilevel change is effective at promoting the well-being of resettled refugees, including increasing protective factors and reducing emotional distress.
Multilevel modeling of data collected at four time points over 12 months from 290 refugee adults nested within 143 households revealed significant intervention effects across multiple domains. Participants in the intervention experienced significantly greater increases in connection to American culture (acculturation) than the control group. This finding suggests that RWP participants felt more identified with American culture, engaged in more behaviors that demonstrate connection to their new country, and felt more comfortable with understanding and using the English language and interacting with Americans, which are key protective factors for refugee mental health in the long-term (Beiser & Hou, 2001). Research has also documented the protective value of maintaining connection to one’s home culture. Thus, it is important that RWP participants experienced significantly larger increases in connection to their home cultures than the control group and maintained significantly higher levels six months after RWP ended. In fact, refugees in the control group experienced decreased connection to American and home cultures over time. Disconnection to both home and new cultures is described as marginalization (Berry, 1997), and has been shown to be related to lower levels of mental health (Berry & Hou, 2016).
Participants in the RWP also reported significantly higher levels of English proficiency than control group participants. These differences were observed starting at the mid-intervention time point and were maintained at the post-intervention and 6-month follow-up time points. This finding is important, because numerous studies have documented limited English proficiency as one of the primary stressors reported by refugees, a major barrier to satisfactory employment, and a key predictor of mental health problems among refugees resettled in the U.S. (Alemi, James, Cruz, Zepeda, & Racadio, 2014; Brown, Schale, & Nilsson, 2010; Kirmayer et al., 2011).
Social support is another key predictor of refugee mental health and well-being (Alemi, James, & Montgomery, 2015; Isakson & Jurkovic, 2013; Soller, Goodkind, Greene, Browning, & Shantzek, 2018). RWP and control group participants experienced similar levels of social support from family members and members of their own ethnic/nationality community, but RWP participants reported significantly greater increases in social support from non-ethnic community members (their broader local community) during the intervention time period. Although the difference in levels of social support was not maintained at 6-month follow-up, this finding provides evidence that during the intervention period, refugees’ social support and connection with Americans increased. This suggests that RWP was effective at increasing this important protective factor, but that ways to make this change sustainable over time need to be explored.
The final intervention effects we found relate to refugees’ emotional distress, as measured by levels of depression and anxiety symptoms. Although these findings were not consistent across all regional/nationality groups of refugees, Iraqis and Syrians in the RWP group had significantly lower levels of overall emotional distress than their counterparts in the control group 6-months post-intervention, and Afghans in the RWP group experienced significantly greater decreases in emotional distress over time than those in the control group. No significant differences in emotional distress were detected between African participants in the RWP and control groups. However, our qualitative outcome data and tracking of achievements among African households who participated in the RWP suggest that African participants experienced equal or greater impacts on their mental health as Afghan, Iraqi and Syrian participants. For example, in the words of a participant from the DRC:
It [RWP] has changed my life completely. Before I met these guys [undergraduate advocates], I was suicidal. I felt like I just wanna die, I wanted to kill myself. When my daughter passed back home [in a refugee camp], between her and the pregnancy, it was six months…Then I got here with hope and everything, and then she dies [participant had a miscarriage]. I didn’t have nobody to talk to…My blood pressure was going so high. They even took me to the hospital, and they would just have me tied. They thought I was gonna kill myself in the hospital because I was going mad….The program changed my life. We have learned so many things. The program helped, before the program began, I was feeling sad and I feel like I wanted to finish my life and not only myself, the whole family was going through hard times. My husband needed some kind of certificate education. We didn’t have anything. We were struggling financially, emotionally, you know, everything. But when we begin the program, the program helped us, especially Katy [undergraduate advocate]. She helped my husband to go to school and he was able to get his certificate [Certified Nursing Assistant] which helped him to get the job that he’s working now and it changed the whole family. So it’s just a lot of things.
Extensive discussion among research team members from the Great Lakes Region of Africa suggests several explanations for the lack of significant differences on the measures of emotional distress between African RWP and control participants. In part, these findings may be because the African group was the smallest (with only 39 households). Because patterns of mental health effects differed across the three nationalities, effects had to be examined separately through Nationality × Condition interactions, which resulted in lower power for these analyses: Afghan (59 households), Iraqi/Syrian (53 households), and Great Lakes African (39 households), with minimum detectable effect sizes of .45, .47, and .55, respectively. In addition, African households started out with the lowest mean scores on all three emotional distress scales. We do not know whether these lower levels of emotional distress reflect actual experiences of less distress among African participants or if cultural norms around trust and expressions of distress may have affected participants’ responses. One of the strengths of the CBPR approach guiding this study is the ability to discuss these issues in-depth with research team and community advisory council members who came to the U.S. as refugees from the countries represented in the study. Insights from these discussions suggest that Great Lakes Africans: 1) may be less likely to report emotional distress in interviews due to lack of trust/comfort whereas Afghans, Iraqis and Syrians may feel more comfortable expressing their distress with interviewers from the same backgrounds as them; 2) may be more likely to report emotional distress only to religious/spiritual leaders rather than to family, friends, other community members, or health professionals; 3) may have experienced more deprivation related to basic needs than Afghans, Iraqis, and Syrians and therefore not be as focused on emotional distress during their initial resettlement; and 4) may use coping strategies that emphasize the positive and involve shifting focus away from feelings of distress. Future research efforts should address these concerns through further exploration of these measurement issues.
Taken together, the significant intervention effects across multiple domains of refugee mental health and well-being provide promising support for the multilevel, social justice approach of the RWP intervention. This is particularly important given that research studies have shown that Afghan, Great Lakes African, Iraqi, and Syrian refugees have high levels of emotional distress following resettlement (Taylor et al., 2014; Vukovich, 2016), which often persist for many years (Alemi et al., 2015; Lamkaddem et al., 2014; Slewa-Younan, Uribe Guajardo, Heriseanu, & Hasan, 2015), and that refugees from these populations have low rates of usage of mental health services (Lamkaddem et al., 2014; Slewa-Younan et al., 2015).
Future analyses to investigate mechanisms of change through mediating effects will be an informative next step in these complex efforts to implement and study social change processes and their impact on refugees’ mental health. In addition, the extensive qualitative data collected from refugee and student participants, which is beyond the scope of this paper, provides important support for our quantitative findings, further explores participants’ experiences in RWP, and documents outcomes not measured quantitatively or experienced uniformly.
Limitations
It is important to note that implementing a community-based RCT of RWP raised methodological, theoretical, and ethical challenges that required consideration, discussion, and adjustments. Our research team developed several innovations to address these challenges, which are beyond the scope of this paper (see Goodkind et al., 2017 for an in-depth discussion of challenges and associated innovations). However, we want to highlight here that we share concerns and reservations about the utility, appropriateness, and validity of RCTs (Bonell, Melendez-Torres, & Quilley, 2018), while also recognizing the critical insight they can provide. The multiple languages and cultures represented in this study raise concerns related to measurement validity. Despite intensive efforts to ensure accurate cultural and linguistic translation of measures, it is possible that we did not measure emotional distress in the ways that were most relevant to participants. However, another strength of this study is its demonstration of the feasibility and acceptability of implementing a culturally appropriate mental health intervention with multiple nationality, ethnic and linguistic groups within a unified group model. For further discussion of lessons learned from this multicultural yet culturally grounded intervention, see Hess and Goodkind (under review). Finally, although the sample size of 290 refugee adults is relatively large for a community-based mental health intervention study, power to detect intervention effects was limited by having to account for individuals nested within households and the need to attend to interaction effects. However, the numerous significant intervention effects we found in spite of these power limitations are encouraging.
Practice Implications
Despite clear evidence that refugee mental health is strongly related to post-migration stressors, few interventions beyond individual clinical approaches have been developed or tested to reduce the high rates of emotional distress among refugees. Thus, the RWP is innovative in its focus on addressing many of the social determinants of refugee mental health from a holistic, strengths-based perspective. In addition to the promising effectiveness of this approach, the RWP model is particularly appealing because most refugees (89%) were interested and willing to participate and intervention retention of households was extremely high (100%). This type of universal, non-stigmatizing approach is essential in order to reach many refugees experiencing emotional distress who are less likely to access formal mental health services because of stigma, lack of trust, lack of understanding of the role of mental health professionals, lack of care coordination, and limited culturally appropriateness of interventions and culturally-sensitive providers (Colucci, Minas, Szwarc, Guerra, & Paxton, 2015; Piwowarczyk, Bishop, Yusuf, Mudymba, & Raj, 2014; Shannon, Wieling, Simmelink-McCleary, & Becher, 2015). In addition, the RWP is relatively low in cost to implement, replicable, and sustainable. The intervention manual is available at rwp.unm.edu for mental health professionals, community organizations, and university faculty, students, staff who would like to implement it in their communities.
Conclusions
Given the current sociopolitical context of migration, including increasing uncertainty, discrimination, stigma, lack of access to resources, family separation, and fear of deportation based on policy changes and public perception of refugees/immigrants as a threat, interventions that build relationships between Americans and newcomers, create safe welcoming spaces, and emphasize collective social change to make communities and systems more responsive to needs, goals, and rights of newcomers are even more essential. Building evidence that this type of multilevel approach increases refugees’ social support, English proficiency, and cultural connections and decreases their emotional distress is an important step in these efforts.
Highlights.
Multilevel strengths-based intervention decreases refugee distress and improves protective factors
Holistic focus on psychological, material, social, educational, and cultural needs is effective
High recruitment/retention rates support importance of non-stigmatizing universal interventions
RWP intervention reaches refugees unlikely to access formal mental health services
RWP circumvents typical barriers to services (stigma, trust, linguistic/cultural appropriateness)
Footnotes
Afghanistan has experienced ongoing violence and conflict for the past 100 years. It has been estimated that one out of every four Afghans lives as a refugee. Most Afghan refugees in the United States are Muslim but represent multiple different ethnic groups. Educational and socioeconomic backgrounds vary, but many women have not had the opportunity to attend school previously to their displacement.
Many of the Iraqi refugees currently in the United States were selected for resettlement because their relationship with U.S. operations in Iraq made them targets for killings, torture, and/or discrimination. Other Iraqi refugees are members of religious minority groups who were persecuted heavily after U.S. intervention in Iraq; thus, Iraqi refugees include people who are Muslim, Christian, and several other religions. Many Iraqi refugees have high levels of education and most come from urban settings. Since 2011, more than 60% of Syrians (over 13.5 million of the country’s total population of 22 million) have been forcibly displaced from their country due to civil war. Most Syrian refugees are Muslim, but some are members of ethnic and religious minorities, such as Kurds, Druze, and Christians. Syrian refugees have diverse educational and socioeconomic backgrounds.
The Great Lakes region of Africa refers to several eastern/central African countries that surround a series of lakes including Lake Kivu, Lake Tanganyika and Lake Victoria. A majority of the refugees from this region who have resettled in the United States are from Burundi, Rwanda and eastern Democratic Republic of Congo (DRC). Between 1993 and 2008, the Great Lakes Region faced the deadliest conflict the world had seen since World War II. In this period, an estimated 300,000 Burundians were killed in civil war, and an estimated 800,000 Rwandans were killed in a genocide, which in turn sparked conflict in eastern DRC, killing an estimated 5.4 million people. Most refugees from this region are Christian, although some are Muslim. They come from multiple ethnic groups, and there is extensive diversity in terms of their educational and socioeconomic backgrounds.
Contributor Information
Jessica R. Goodkind, Department of Sociology, University of New Mexico, MSC05 3080, Albuquerque, NM 87131.
Deborah Bybee, Michigan State University Department of Psychology
Julia Meredith Hess, University of New Mexico Department of Pediatrics
Suha Amer, University of New Mexico Center for Social Policy
Martin Ndayisenga, University of New Mexico Center for Social Policy
R. Neil Greene, University of New Mexico Department of Sociology
Ryeora Choe, University of New Mexico Department of Sociology
Brian Isakson, University of New Mexico Department of Psychiatry
Brandon Baca, University of New Mexico Center for Social Policy
Mahbooba Pannah, University of New Mexico Center for Social Policy.
References
- Alemi Q, James S, Cruz R, Zepeda V, & Racadio M (2014). Psychological Distress in Afghan Refugees: A Mixed-Method Systematic Review. Journal of Immigrant and Minority Health, 16(6), 1247–1261. 10.1007/s10903-013-9861-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alemi Q, James S, & Montgomery S (2015). Correlates and Predictors of Psychological Distress among Afghan Refugees in San Diego County HHS Public Access. International Journal of Culture and Mental Health, 1(83), 274–288. 10.1080/17542863.2015.1006647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alemi Q, & Stempel C (2018). Discrimination and distress among Afghan refugees in northern California: The moderating role of pre- and post-migration factors. PLoS ONE, 13(5), e0196822 10.1371/journal.pone.0196822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annan J, Green EP, & Brier M (2013). Promoting recovery after war in Northern Uganda: Reducing daily stressors by alleviating poverty. Journal of Aggression, Maltreatment and Trauma, 22(8), 849–868. 10.1080/10926771.2013.823636 [DOI] [Google Scholar]
- Behnia B (2003). Survivors of War and Torture. International Journal of Mental Health, 32(4), 3–18. [Google Scholar]
- Beiser M, & Hou F (2001). Language acquisition, unemployment and depressive disorder among Southeast Asian refugees: a 10-year study. Social Science & Medicine, 53(10), 1321–1334. [DOI] [PubMed] [Google Scholar]
- Beiser M, & Hou F (2017). Predictors of positive mental health among refugees: Results from Canada’s General Social Survey. Transcultural Psychiatry, 54(5–6), 675–695. 10.1177/1363461517724985 [DOI] [PubMed] [Google Scholar]
- Berry JW (1997). Immigration, Acculturation and Adaptation. Acculturation Model, 46(1). 10.1111/j.1464-0597.1997.tb01087.x [DOI] [Google Scholar]
- Berry JW, & Hou F (2016). Immigrant acculturation and wellbeing in Canada. Canadian Psychology, 57(4), 254–264. 10.1037/cap0000064 [DOI] [Google Scholar]
- Birman D, & Tran N (2008). Psychological distress and adjustment of Vietnamese refugees in the United States: Association with pre- and postmigration factors. American Journal of Orthopsychiatry, 78(1), 109–120. 10.1037/0002-9432.78.1.109 [DOI] [PubMed] [Google Scholar]
- Birman D, Trickett EJ, & Vinokurov A (2002). Acculturation and Adaptation of Soviet Jewish Refugee Adolescents: Predictors of Adjustment Across Life Domains. American Journal of Community Psychology, 30(5), 585–607. 10.1023/A:1016323213871 [DOI] [PubMed] [Google Scholar]
- Bonell C, Melendez-Torres GJ, & Quilley S (2018). The potential role for sociologists in designing RCTs and of RCTs in refining sociological theory: A commentary on Deaton and Cartwright. Social Science and Medicine, 210(2018), 29–31. 10.1016/j.socscimed.2018.04.045 [DOI] [PubMed] [Google Scholar]
- Brown C, Schale CL, & Nilsson JE (2010). Vietnamese immigrant and refugee women’s mental health: An examination of age of arrival, length of stay, income, and English language proficiency. Journal of Multicultural Counseling and Development, 38(2), 66–76. 10.1002/j.2161-1912.2010.tb00115.x [DOI] [Google Scholar]
- Carlsson JM, Mortensen EL, & Kastrup M (2006). Predictors of mental health and quality of life in male tortured refugees. Nordic Journal of Psychiatry, 60(1), 51–57. 10.1080/08039480500504982 [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. Hillsdale, N.J.: Erlbaum. [Google Scholar]
- Colucci E, Minas H, Szwarc J, Guerra C, & Paxton G (2015). In or out? Barriers and facilitators to refugee-background young people accessing mental health services. Transcultural Psychiatry, 52(6), 766–790. 10.1177/1363461515571624 [DOI] [PubMed] [Google Scholar]
- Edge S, & Newbold B (2013). Discrimination and the health of immigrants and refugees: Exploring Canada’s evidence base and directions for future research in newcomer receiving countries. Journal of Immigrant and Minority Health, 15, 141–148. 10.1007/s10903-012-9640-4 [DOI] [PubMed] [Google Scholar]
- Enders C (2010). Applied missing data analysis. New York: Guilford Press. [Google Scholar]
- Fazel M, Wheeler J, & Danesh J (2005). Prevalence of serious mental disorder in 7000 refugees resettled in western countries: A systematic review. Lancet, 365, 1309–1314. 10.1016/S0140-6736(05)61027-6 [DOI] [PubMed] [Google Scholar]
- Feingold A (2009). Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods, 14(1), 43–53. 10.1037/a0014699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold A (2015). Confidence interval estimation for standardized effect sizes in multilevel and latent growth modeling. Journal of Consulting and Clinical Psychology, 83(1), 157–168. 10.1037/a0037721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodkind J (2005). Effectiveness of a community-based advocacy and learning program for Hmong refugees. American Journal of Community Psychology, 36(3/4), 387–408. doi: 10.1007/s10464-005-8633-z. [DOI] [PubMed] [Google Scholar]
- Goodkind J (2006). Promoting Hmong refugee’s well-being through mutual learning: Valuing knowledge, culture, and experience. American Journal of Community Psychology, 37(1/2), 77–93. doi: 10.1007/s10464-005-9003-6. [DOI] [PubMed] [Google Scholar]
- Goodkind J, Amer S, Christian C, Hess JM, Bybee D, Isakson B,… Shantzek C (2017). Challenges and innovations in a community-based participatory randomized controlled trial. Health Education & Behavior, 44(1), 123–130. doi: 10.1177/1090198116639243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodkind J, Githinji A, & Isakson B (2011). Reducing health disparities experienced by refugees resettled in urban areas: A community-based transdisciplinary intervention model (pp. 41–55) In Kirst M, Schaefer-McDaniel N, Hwang S, & O’Campo P (Eds.). Converging disciplines: A transdisciplinary research approach to urban health problems. New York, NY: Springer. [Google Scholar]
- Goodkind J, Hang P, & Yang M (2004). Hmong refugees in the United States: A community-based advocacy and learning intervention In Miller K & Rasco L (Eds.) The mental health of refugees: Ecological approaches to healing and adaptation. Mahwah, NJ: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Goodkind J, Hess JM, Isakson B, LaNoue M, Githinji A, Roche N, Vadnais K, & Parker DP (2014). Reducing refugee mental health disparities: A community-based intervention to address post-migration stressors with African adults. Psychological Services, 11(3), 333–346. doi: 10.1037/a0035081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorst-Unsworth C, & Goldenberg E (1998). Psychological sequelae of torture and organised violence suffered by refugees from Iraq. Trauma-related factors compared with social factors in exile. British Journal of Psychiatry : The Journal of Mental Science, 172, 90–94. [DOI] [PubMed] [Google Scholar]
- Haines DW (2010). Safe haven?: A history of refugees in America. Sterling: Kumarian Press. [Google Scholar]
- Hedeker DR, & Gibbons RD (2006). Longitudinal data analysis. Hoboken, NJ: Wiley-Interscience. [Google Scholar]
- Hess JM, Isakson B, Roche N, Vadnais K, Parker DP, & Goodkind J (i2014). Reducing mental health disparities through transformative learning: A social change model with refugees and students. Psychological Services, 11(3), 347–356. doi: 10.1037/a0035334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinton DE, Chhean D, Pich V, Safren SA, Hofmann SG, & Pollack MH (2005). A randomized controlled trial of cognitive-behavior therapy for Cambodian refugees with treatment-resistant PTSD and panic attacks: A cross-over design. Journal of Traumatic Stress, 18(6), 617–629. 10.1002/jts.20070 [DOI] [PubMed] [Google Scholar]
- Hollifield M, Warner TD, Lian N, Krakow B, Jenkins JH, Kesler J, … Westermeyer J (2002). Measuring trauma and health status in refugees: a critical review. JAMA, 288(5), 611–621. [DOI] [PubMed] [Google Scholar]
- Ichikawa M, Nakahara S, & Wakai S (2006). Effect of Post-Migration Detention on Mental Health Among Afghan Asylum Seekers in Japan. Australian & New Zealand Journal of Psychiatry, 40(4), 341–346. 10.1080/j.1440-1614.2006.01800.x [DOI] [PubMed] [Google Scholar]
- Isakson BL, & Jurkovic GJ (2013). Healing after torture: The role of moving on. Qualitative Health Research, 23(6), 749–761. 10.1177/1049732313482048 [DOI] [PubMed] [Google Scholar]
- Kim I (2016). Beyond Trauma: Post-resettlement Factors and Mental Health Outcomes Among Latino and Asian Refugees in the United States. Journal of Immigrant and Minority Health, 18, 740–748. 10.1007/s10903-015-0251-8 [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder a. G., Guzder J, … Pottie K (2011). Common mental health problems in immigrants and refugees: general approach in primary care. Canadian Medical Association Journal, 183, E959–E967. 10.1503/cmaj.090292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamkaddem M, Stronks K, Devillé WD, Olff M, Gerritsen AA, & Essink-Bot M-L (2014). Course of post-traumatic stress disorder and health care utilisation among resettled refugees in the Netherlands. BMC Psychiatry, 14(1), 90 10.1186/1471-244X-14-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layne C, Warren J, Hilton S, Pasalic A, Katalkinski R, & Pynoos R (2009). Measuring Adolescent Perceived Support Amidst War and Disaster In Barber B (Ed.), Adolescents and war: How youth deal with political violence (pp. 135–176). New York, NY: Oxford University Press. [Google Scholar]
- Miller KE, & Rasmussen A (2010). War exposure, daily stressors, and mental health in conflict and post-conflict settings: Bridging the divide between trauma-focused and psychosocial frameworks. Social Science and Medicine, 70(1), 7–16. 10.1016/j.socscimed.2009.09.029 [DOI] [PubMed] [Google Scholar]
- Miller KE, & Rasmussen A (2014). War experiences, daily stressors and mental health five years on : Elaborations and future directions. Intervention, 12(1), 33–42. 10.1097/WTF.0000000000000066 [DOI] [Google Scholar]
- Miller KE, Weine SM, Ramic A, Brkic N, Bjedic ZD, Smajkic A, … Worthington G (2002). The relative contribution of war experiences and exile-related stressors to levels of psychological distress among Bosnian refugees. Journal of Traumatic Stress, 15(5), 337–287. 10.1023/A:1020181124118 [DOI] [PubMed] [Google Scholar]
- Mollica RF, Wyshak G, de Marneffe D, Khuon F, & Lavelle J (1987). Indochinese versions of the Hopkins Symptom Checklist-25: a screening instrument for the psychiatric care of refugees. American Journal of Psychiatry, 144(4), 497–500. 10.1176/ajp.144.4.497 [DOI] [PubMed] [Google Scholar]
- Nakash O, Nagar M, Shoshani A, Zubida H, & Harper RA (2012). The effect of acculturation and discrimination on mental health symptoms and risk behaviors among adolescent migrants in Israel. Cultural Diversity and Ethnic Minority Psychology, 18(3), 228–238. 10.1037/a0027659 [DOI] [PubMed] [Google Scholar]
- Neuner F, Schauer M, Klaschik C, Karunakara U, & Elbert T (2004). A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an african refugee settlement. Journal of Consulting and Clinical Psychology, 72(4), 579–587. 10.1037/0022-006X.72.4.579 [DOI] [PubMed] [Google Scholar]
- Office of Refugee Resettlement. (2008). Report to Congress - FY 2008.
- Pham PN, Vinck P, & Stover E (2009). Returning home: Forced conscription, reintegration, and mental health status of former abductees of the Lord’s Resistance Army in northern Uganda. BMC Psychiatry. 10.1186/1471-244X-9-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piwowarczyk L, Bishop H, Yusuf A, Mudymba F, & Raj A (2014). Congolese and Somali Beliefs About Mental Health Services. The Journal of Nervous and Mental Disease, 202(3), 209–216. 10.1097/NMD.0000000000000087 [DOI] [PubMed] [Google Scholar]
- Porter M, & Haslam N (2005). Predisplacement and Postdisplacement Factors Associated With Mental Health of Refugees and Internally Displaced Persons A Meta-analysis. JAMA, 294(5), 602–612. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational Tools for Probing Interactions in Multiple Linear Regression, Multilevel Modeling, and Latent Curve Analysis. Journal of Educational and Behavioral Statistics, 31(4), 437–448. 10.3102/10769986031004437 [DOI] [Google Scholar]
- Rasmussen A, Nguyen L, Wilkinson J, Vundla S, Raghavan S, Miller KE, & Keller AS (2010). Rates and Impact of Trauma and Current Stressors Among Darfuri Refugees in Eastern Chad. American Journal of Orthopsychiatry, 80(2), 227–236. 10.1111/j.1939-0025.2010.01026.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush S, Bryk AS, & Congdon R (2002). Hierarchical linear models : applications and data analysis methods. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Raudenbush S, & Liu X-F (2001). Effects of Study Duration, Frequency of Observation, and Sample Size on power in studies of group differences in polynomial change. Psychological Methods, 6, 387–401. [PubMed] [Google Scholar]
- Rumbaut RG (1989). The Structure of Refuge: Southeast Asian Refugees in the United States, 1975–1985, 1, 97–129. [Google Scholar]
- Shannon PJ, Wieling E, Simmelink-McCleary J, & Becher E (2015). Beyond Stigma: Barriers to Discussing Mental Health in Refugee Populations. Journal of Loss and Trauma, 20(3), 281–296. 10.1080/15325024.2014.934629 [DOI] [Google Scholar]
- Slewa-Younan S, Uribe Guajardo MG, Heriseanu A, & Hasan T (2015). A Systematic Review of Post-traumatic Stress Disorder and Depression Amongst Iraqi Refugees Located in Western Countries. Journal of Immigrant and Minority Health, 17(4), 1231–1239. 10.1007/s10903-014-0046-3 [DOI] [PubMed] [Google Scholar]
- Soller B, Goodkind JR, Greene RN, Browning CR, & Shantzek C (2018). Ecological Networks and Community Attachment and Support Among Recently Resettled Refugees. American Journal of Community Psychology, 61(3–4), 332–343. 10.1002/ajcp.12240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spybrook J; Bloom H; Congon R; Hill C; Martinez A & Raudenbush S (2011). Optimal Design Plus Version 3.0. Retrieved from www.wtgrantfoundation.org
- Steel Z, Chey T, Silove D, Marnane C, Bryant R a, & van Ommeren M (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA : The Journal of the American Medical Association, 302, 537–549. 10.1001/jama.2009.1132 [DOI] [PubMed] [Google Scholar]
- Stepakoff S, Hubbard J, Katoh M, Falk E, Mikulu J-B, Nkhoma P, & Omagwa Y (2006). Trauma healing in refugee camps in guinea: A psychosocial program for Liberian and Sierra Leonean survivors of torture and war. American Psychologist, 61(8), 921–932. 10.1037/0003-066X.61.8.921 [DOI] [PubMed] [Google Scholar]
- Survey Research Center. (2016). Guidelines for Best Practice in Cross-Cultural Surveys. Ann Arbor, MI: Retrieved from http://www.ccsg.isr.umich.edu/ [Google Scholar]
- Taylor EM, Yanni EA, Pezzi C, Guterbock M, Rothney E, Harton E, … Burke H (2014). Physical and Mental Health Status of Iraqi Refugees Resettled in the United States. Journal of Immigrant and Minority Health, 16(6), 1130–1137. 10.1007/s10903-013-9893-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Homeland Security. (2018). Yearbook of Immigration Statistics: 2004. Director. Retrieved from https://www.dhs.gov/immigration-statistics/yearbook
- UNHCR. (2018). UNHCR Global Trends - Forced Displacement in 2017. Retrieved February 18, 2019, from https://www.unhcr.org/globaltrends2017/
- Vukovich MM (2016). Exploring Ethnocultural Differences in Distress of Newly Arrived Refugees During Early Resettlement: A Mixed Methods Dissertation. Retrieved from https://digitalcommons.du.edu/etd/1196
- Weine SM, Razzano L, Brkic N, Ramic A, Miller K, Smajkic A, … Pavkovic I (2000). Profiling the trauma related symptoms of Bosnian refugees who have not sought mental health services. The Journal of Nervous and Mental Disease, 188(7), 416–421. [DOI] [PubMed] [Google Scholar]


