Graphical abstract
Keywords: Cardiac hemangioma, Echocardiography, Cardiac magnetic resonance imaging
Highlights
-
•
Cardiac hemangiomas constitute <10% of all pediatric cardiac tumors.
-
•
More than two thirds of patients with cardiac masses may present with symptoms.
-
•
Association between congenital heart disease and heart tumors is very uncommon.
-
•
Echocardiography is the first-line imaging modality for identifying cardiac masses.
-
•
CMR is an excellent imaging technique for cardiac tumor characterization.
Introduction
Primary cardiac tumors in the pediatric population are extremely rare. An incidence of 0.14%1 has been reported during fetal life and 0.17% in childhood, on the basis of echocardiographic reports.2 Cardiac hemangiomas constitute <10% of cases of primary pediatric cardiac tumors.3 Hemangiomas are benign tumors that are typically diagnosed in symptomatic patients. Although echocardiography is the first-line imaging modality for identifying cardiac masses, cardiac magnetic resonance imaging (CMR) has an increasingly important role in the localization and differentiation of cardiac masses. We present the case of an asymptomatic patient who presented to his cardiologist for his annual follow-up visit for repaired congenital heart disease and was found to have a new mass in his heart.
Case Presentation
A 14-year-old male patient with a history of complete atrioventricular canal defect repaired in infancy (one-patch technique for atrial septal defect and primary closure for ventricular septal defect) presented for routine annual follow-up. He was clinically well and denied symptoms of chest pain, palpitations, or exertional fatigue. Results of physical examination were unremarkable, and electrocardiographic findings were unchanged, demonstrating sinus rhythm with left-axis deviation and right bundle branch block.
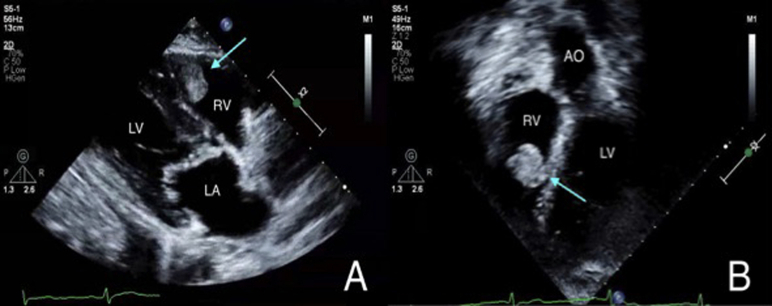
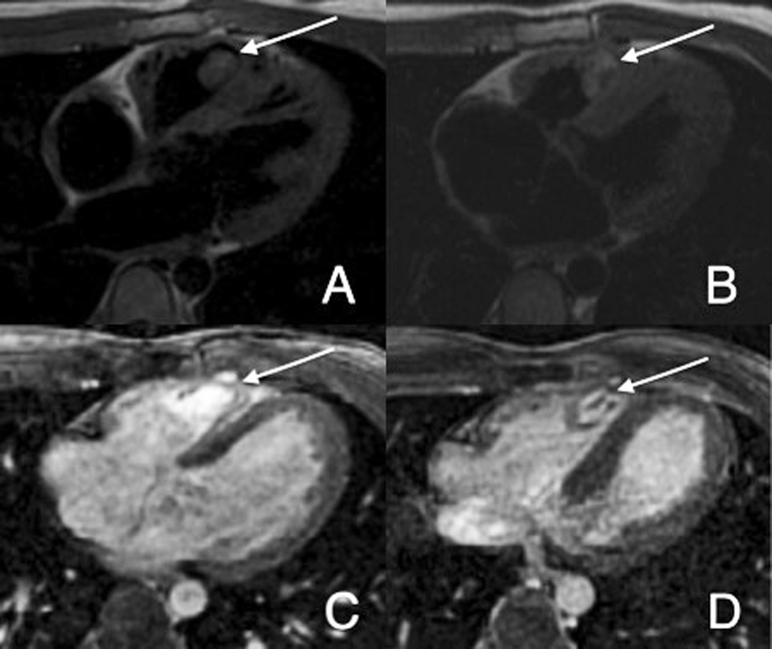
On transthoracic echocardiography, a large, homogenous, slightly mobile, nonobstructive echogenicity was seen in the body of the right ventricle that appeared to be related to the moderator band (Figures 1A and 1B). This mass was not present on the previous echocardiogram, obtained 1 year prior. The echocardiogram was also notable for normal biventricular systolic function and a tiny residual ventricular septal defect, which was unchanged compared with previous echocardiograms. CMR was performed, showing a mobile mass in the right ventricle adjacent to the moderator band measuring 1.2 × 1.8 cm in the axial plane and 1.2 × 2.2 cm in the short-axis plane. On tissue characterization imaging, the mass was isointense on T1 imaging (Figure 2A), hyperintense on T2 imaging with a small area of isointensity representing the moderator band (Figure 2B), and hyperintense on first-pass perfusion (FPP) imaging (Figure 2C). Hyperintensity was noted on myocardial delayed enhancement imaging (Figure 2D). On the basis of these findings, a benign vascular tumor was considered the most likely diagnosis, although malignancy could not be excluded. To determine its etiology, surgical resection was planned after review with the oncology and cardiothoracic surgery teams.
Figure 1.
Transthoracic echocardiography with a large homogeneous echogenicity (arrow) in the body of the right ventricle (RV) seen on (A) parasternal long-axis and (B) four-chamber view tilting anteriorly into the left ventricular outflow tract. AO, Aorta; LA, left atrium; LV, left ventricle.
Figure 2.
CMR axial view showing a mass (arrow) in the right ventricle. (A) Isointense signal on T1 imaging. (B) Hyperintense signal on T2 imaging with a small area of isointensity, likely representing the moderator band. (C) On FPP imaging, the mass becomes hyperintense. (D) On myocardial delayed enhancement imaging, the mass is hyperintense and homogeneous without evidence of dark core.
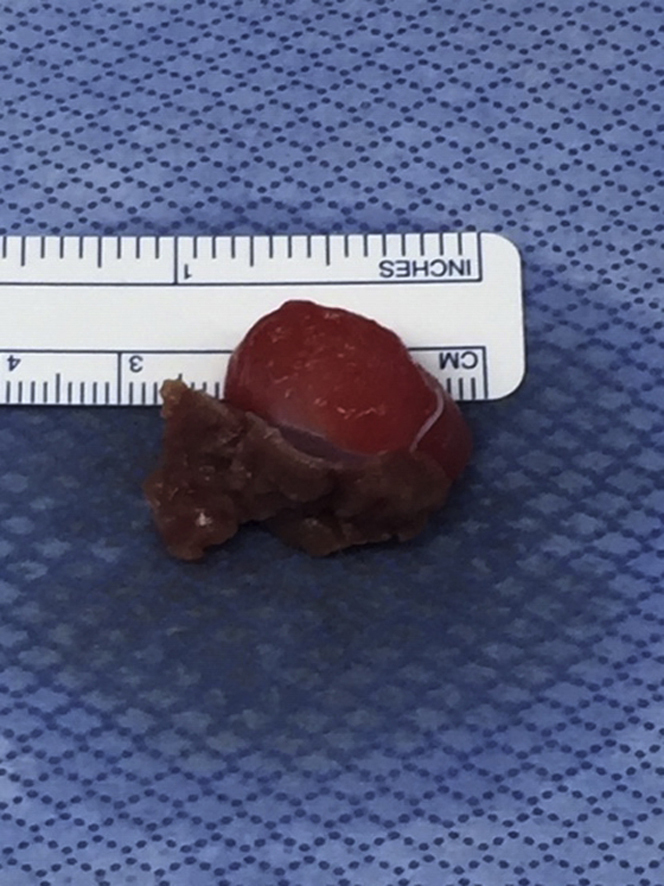
The right ventricular mass was surgically removed. The tumor was located at the angle between the interventricular septum and the free wall of the right ventricle, at the level of the moderator band (Figure 3), close but not adherent to the tricuspid valve subapparatus. The histopathologic diagnosis was consistent with mixed-type cavernous-capillary hemangioma without evidence of malignancy. After an uneventful postoperative course, the patient was discharged home and showed no evidence of recurrence on echocardiography at 2-month follow-up.
Figure 3.
Gross pathology of the mass surgically resected from the right ventricle.
Discussion
Association between congenital heart disease and heart tumors is very uncommon. Only a few reports have described patients with cardiac hemangiomas and congenital heart disease. A case report described an association between a duct-dependent congenital heart disease and hemangioma in a newborn.4 Also, a tricuspid valve hemangioma was found in a newborn with hypoplastic left heart syndrome.5
The presence of cardiac tumors in asymptomatic pediatric patients is rare. More than two thirds of patients (68.5%) with cardiac tumors may present with symptoms of congestive heart failure, arrhythmias, chest pain, palpitations, respiratory distress, and neurologic symptoms (syncope and stroke).3
Hemangiomas can be localized anywhere within the heart but most commonly in the right atrium and right ventricle.6 Right-heart hemangiomas can cause systemic venous congestion, outflow tract obstruction, elevated right ventricular end-diastolic pressures, right ventricular hypertrophy, and irreversible right ventricular dysfunction. On electrocardiography, ST-segment abnormalities, signs of ventricular hypertrophy, preexcitation, strain, and dysrhythmia are seen as early signs of tumor involvement.7
Macroscopically, cardiac hemangiomas are typically localized single masses measuring no more than 4 cm. They may be sessile or polypoid with purple or red color.8 Mixed-type capillary-cavernous hemangiomas are considered vascular malformations according to the latest International Society for the Study of Vascular Anomalies classification.9
Echocardiography plays a crucial role as the primary imaging modality in the identification of cardiac masses. Echocardiography is readily available, is radiation free, and provides real-time images with good resolution. It can detect a cardiac mass location and provide information on the morphology, mobility, attachment, and size of the tumor. Its limitations are suboptimal evaluation of extracardiac structures, poor soft tissue characterization to classify the type of tumor,10 and operator dependency. When a cardiac mass is found on echocardiography, the diagnostic approach should focus on location, imaging characteristics, and clinical correlation of the tumor.
Cardiac hemangiomas are located frequently in the right ventricle but constitute only a few cases in the wide spectrum of ventricular cardiac tumors. They are masses made with dilated vascular channels, and their appearance on echocardiography is as echogenic masses with echolucency.11 The most common ventricular tumors are rhabdomyomas, which are also the most common cardiac tumors in children. On echocardiography, they appear as hyperechoic solid masses and are associated with tuberous sclerosis.10 Fibromas are the second most common cardiac tumors. On echocardiography, fibromas are large, noncontractile, heterogeneous solid masses on the ventricular septum or ventricular free wall.10 These diagnoses cannot be ruled out through their imaging characteristics alone, given that echography has poor ability to characterize soft tissue masses.
CMR is an excellent imaging technique for tumor characterization and for evaluating tumor effects on surrounding structures. One of the advantages of CMR is that it does not require the use of ionizing radiation. CMR with contrast can differentiate a tumor mass from a thrombus and distinguish between benign and malignant tumors.10 In a previous review, 97% of pediatric cardiac tumors were correctly diagnosed on the basis of size, location, presence of pleural or pericardial effusion, hemodynamic impact, and signal characteristics with a set of predefined CMR diagnostic criteria.6 Tumors more frequently found, such as rhabdomyomas or fibromas, have particular features on CMR. Rhabdomyomas are isointense to myocardium on T1 imaging, hyperintense on T2 imaging, and hypointense on FPP imaging, while fibromas are hypo- or hyperintense on T1 and T2 imaging and hypointense on FPP imaging.12 The characteristic features of hemangioma include intermediate signal on T1 imaging, hyperintense signal on T2 sequences, and avid enhancement on FPP imaging, given the increased vascularity of hemangioma.12 Myocardial delayed enhancement shows variable, often weak (isointense or hypointense) enhancement.6 None of the other benign cardiac tumors are clearly positive on FPP imaging, making this the most important CMR signal characteristic to diagnose a cardiac hemangioma. However, currently available CMR sequences may not allow differentiation between benign hemangiomas and malignant vascular tumors, unless frank signs of invasion or metastasis are seen.12 Surgical resection is required for histopathologic diagnosis to rule out malignancy.
The progression of cardiac hemangiomas is uncertain; some instances of spontaneous resolution have been described, along with enlargement of the tumors on follow-up after their first detection.13 The present case report is an example of how large cardiac hemangiomas can grow in a short period of time. Regular follow-up care after cardiac surgery prevented the development of the symptoms previously described.
Conclusion
Cardiac hemangiomas are extremely rare tumors among all cardiac neoplasms, and there is significant value in the use of CMR in addition to echocardiography in the diagnosis of hemangiomas. We describe an unusual clinical presentation of a cardiac hemangioma in an asymptomatic patient with a history of congenital heart disease and discuss the effectiveness of advanced imaging techniques in diagnosis and management.
To our knowledge, this is the first report of a cardiac hemangioma in a pediatric patient with a history of repaired complete atrioventricular canal defect.
Footnotes
Conflicts of interest: The authors reported no actual or potential conflicts of interest relative to this document.
References
- 1.Holley D.G., Martin G.R., Brenner J.I., Fyfe D.A., Huhta J.C., Kleinman C.S. Diagnosis and management of fetal cardiac tumors: a multicenter experience and review of published reports. J Am Coll Cardiol. 1995;26:516–520. doi: 10.1016/0735-1097(95)80031-b. [DOI] [PubMed] [Google Scholar]
- 2.Marx G.A., Moran A.M., Allen H.D., Adams F.H., Moss A.J. Lippincott Williams & Wilkins; Philadelphia, PA: 2001. Heart disease in infants, children and adolescents, including the fetus and young adult; pp. 1432–1445. [Google Scholar]
- 3.Padalino M.A., Vida V.L., Boccuzzo G., Tonello M., Sarris G.E., Berggren H. Surgery for primary cardiac tumors in children. Circulation. 2012;126:22–30. doi: 10.1161/CIRCULATIONAHA.111.037226. [DOI] [PubMed] [Google Scholar]
- 4.Djordjevic S.A., Glumac S., Kalanj J. Cardiac haemangioma associated with a duct-dependent congenital heart disease in a newborn infant. Cardiol Young. 2017;27:990–992. doi: 10.1017/S1047951116002699. [DOI] [PubMed] [Google Scholar]
- 5.Gupta B., Ghosh S., Kujur M., Khetan K., Khumar T. Tricuspid valve hemangioma associated with hypoplastic left heart syndrome presenting as sudden infant death syndrome. Turk Patoloji Dergisi. 2019;35:55–57. doi: 10.5146/tjpath.2015.01362. [DOI] [PubMed] [Google Scholar]
- 6.Beroukhim R.S., Prakash A., Vaslsangiacomo Buechel E.R., Cava J.R., Dorfman A., Festa P. Characterization of cardiac tumors in children by cardiovascular magnetic resonance imaging. J Am Coll Cardiol. 2011;58:1044–1054. doi: 10.1016/j.jacc.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 7.Shaner M.L., Pauliks L.B., Leach D., Myers J.L., Chang D. An adolescent with chest pain and cardiac hemangioma. J Am Acad Phys Assist. 2017;30:25–28. doi: 10.1097/01.JAA.0000513348.07406.4e. [DOI] [PubMed] [Google Scholar]
- 8.Tazelaar H.D., Maleszewski J.J. Tumors of the heart and pericardium. In: Fletcher C.D., editor. Diagnostic Histopathology of Tumors. 5th ed. Elsevier; Philadelphia PA: 2021. pp. 7–42. [Google Scholar]
- 9.Wassef M., Blei F., Adams D., Alomari A., Baselga E., Berestein A. Vascular anomalies classification: recommendations from the International Society for the Study of Vascular Anomalies. Pediatrics. 2015;136:e203–e214. doi: 10.1542/peds.2014-3673. [DOI] [PubMed] [Google Scholar]
- 10.Tao T.Y., Yahyavi-Firouz-Abadi N., Singh G.K., Bhalla S. Pediatric cardiac tumors: clinical and imaging features. Radiographics. 2014;34:1031–1046. doi: 10.1148/rg.344135163. [DOI] [PubMed] [Google Scholar]
- 11.Mankad R., Herrmann J. Cardiac tumors: echo assessment. Echo Res Pract. 2016;3:R65–R77. doi: 10.1530/ERP-16-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahani M.G., Lu J.C., Rigsby C.K., Krishnamurthy R., Dorfman A.L., Agarwal P.P. MRI of pediatric cardiac masses. AJR Am J Roentgenol. 2014;202:971–981. doi: 10.2214/AJR.13.10680. [DOI] [PubMed] [Google Scholar]
- 13.Fan C., Tan C., Kong D., Yang J., Yuan S., Wu S. A giant cavernous hemangioma of the left atrioventricular groove. Case Rep Pediatr. 2017;2017:1–3. doi: 10.1155/2017/6898629. [DOI] [PMC free article] [PubMed] [Google Scholar]