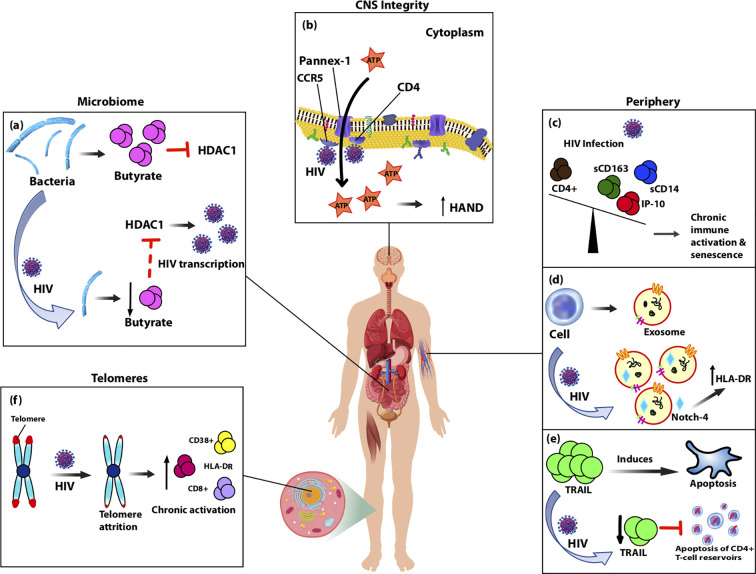
Figure 1.
Diagram showing biomarkers isolated from various anatomical sites of the body that are altered by HIV-infection and likely contribute to accelerated aging observed in people living with HIV (PLWH) on cART through chronic immune activation and inflammation. (A) Typically, gut-associated bacteria, Firmicutes, produces butyrate which inhibits HDAC1. With normal aging or HIV-infection, Firmicutes is replaced causing reduced production of butyrate and consequently increased expression of HDAC1, which acts to increase HIV transcription. (B) Pannex-1 channels, usually closed, open upon binding of HIV to receptors CD4 and co-receptor CCR5, which causes release of ATP, an inflammatory signal. Increased levels of ATP in circulation were correlated with cognitive impairment and thus predictive of CNS compromise. (C) During HIV-infection plasma levels of monocyte activation markers sCD163 and sCD14, as well as pro-inflammatory marker IP-10 are elevated and inversely related with CD4+ T-cell depletion. Over-expression of these markers in the periphery leads to accelerated aging of T cells and senescence. (D) Upon HIV-infection, secretion of exosomes increases along with oxidative stress markers, and HIV-induced chronic activation alters the contents of exosomes. Notch-4 exosomal levels are elevated and correlated with other activation markers, HLA-DR. (E) HIV-infection reduces expression of circulating TRAIL, an apoptosis-inducing protein, which theoretically in turn limits apoptosis of CD4+ T-cell reservoirs allowing for persistent immune activation and inflammation. (F) Telomeres undergo attrition after HIV-infection due to reduced T-cell proliferation and this is associated with cellular senescence markers CD8+, HLA-DR, and CD38+.