Abstract
In February 2020, the exponential growth of COVID-19 cases in Wuhan city posed a huge economic burden to local medical systems. Consequently, Wuhan established Fangcang Shelter hospitals as a One Health approach for responding to and containing the COVID-19 outbreak by isolating and caring for mild-to-moderate cases. However, it is unclear to what degree the hospitals contained COVID-19. This study performed an interrupted time series analysis to compare the number of new confirmed cases of COVID-19 before and after the operation of Fangcang Shelter hospitals. The initial number of confirmed cases in Wuhan increased significantly by 68.54 cases per day prior to February 4, 2020. Compared with the number of cases noted 20 days before the use of Fangcang Shelter hospitals, a sustained reduction in the number of confirmed cases (trend change, −125.57; P < 0.0001) was noted 41 days after the use of the hospitals. Immediate-level changes were observed for confirmed cases (level change, 725.97; P = 0.025). These changes led to an estimated 5148 fewer confirmed cases (P < 0.0001). According to the mean confirmed cases of 395.71 per day before the intervention, we estimated that Wuhan had advanced the terminal phase of COVID-19 by 13 days. Furthermore, immediately after introduction of Fangcang Shelter Hospitals on February 5, the reproduction number dropped rapidly, from a pre-introduction rate of 4.0 to 2.0. The Fangcang Shelter hospitals most likely to reversed the epidemic trend of COVID-19 while a containment strategy was implemented in Wuhan. In a One Health perspective, Fangcang Shelter hospitals, with their functions of isolation and treatment of confirmed COVID-19 patients, engaging professionals from many disciplines, such as medicine, engineering, architecture, psychology, environmental health, and social sciences. The results of this study provide a valuable reference for health policy makers in other countries.
Keywords: COVID-19, SARS-CoV-2, Epidemiology, Wuhan, Fangcang
Abbreviations: COVID-19, coronavirus disease 2019; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2; RT-PCR, Real-time fluorescent reverse transcription polymerase chain reaction; R(t), real-time effective production number; CI, credible intervals; SARS, Severe acute respiratory syndrome; MERS, Middle east respiratory syndrome
Highlights
-
•
A sustained reduction and immediate increase in the number of cases were observed in Wuhan city after Fangcang Shelter hospitals were established.
-
•
The above changes resulted in an estimated 5148 fewer confirmed cases in Wuhan.
-
•
According to the mean confirmed cases of 395.71 per day before the intervention, we estimated that Wuhan had advanced the terminal phase of COVID-19 by 13 days.
-
•
Compared to the approximate real-time effective reproduction number [R(t)] of 4.0 in the pre-operation periods of Fangcang Shelter hospitals, the R(t) was less than 2.0 in the post-operation periods.
1. Introduction
In December 2019, coronavirus disease 2019 (COVID-19), which was caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was reported in Wuhan, Hubei Province, China [1,2]. The emerging disease broke out in Wuhan and quickly spread to other provinces. As of September 4, 2020, China had 89,963 confirmed cases of COVID-19 in 31 provinces (autonomous regions and municipalities directly under the central government) [3].
SARS-CoV-2 belongs to the subfamily Coronavirinae, a taxon that includes other agents of disease such as the Severe Acute Respiratory Syndrome (SARS) in 2003 and the Middle East Respiratory Syndrome (MERS) in 2012 [[4], [5], [6]]. The association of the early stage of the COVID-19 epidemic with the wildlife trade in Wuhan's Southern Seafood Market has been confirmed; specifically, SARS-CoV-2 was discovered to infect mainly wildlife but could be transmitted to humans [1,7]. One Health is an approach that realises human health is closely related to animal health and our common environment [8,9], and it recognises SARS-CoV-2 as a zoonotic virus. Given this perspective, there is a great need to be entirely clear on how SARS-CoV-2 is transmitted between animals and people as well as between people and whether changing the environment can halt the spread of SARS-CoV-2.
Person-to-person transmission of SARS-CoV-2 easily occurs through respiratory droplets and close-contact transmission [1,2]. A containment strategy for COVID-19 based on an interdisciplinary One Health approach, including professionals from many disciplines, such as human, veterinary and environmental health and social sciences, played an important role in stopping the spread of SARS-CoV-2 and successfully fighting against the epidemic [10,11]. The containment strategy for COVID-19 involved putting cities in lockdown, traffic controls, controlling transportation capacity, cancelled or suspended activities, mandatory wearing of face mask in public, immediate case detection and isolation, rigorous close-contact tracing and monitoring/quarantine, staggered return-to-work policies for enterprises and institutions, instituted temperature checks, health care declarations and quarantine against COVID-19 at transportation depots [12]. After approximately 30 days since the implementation of the containment strategy, most of the provinces with primarily imported cases outside Hubei Province reported zero new cases [13].
In the early stages of the epidemic, a serious shortage of medical resources and hospital beds for admitted confirmed patients led to a large number of confirmed patients unable to receive timely isolation and treatment in time, which aggravated cross-infection in the community and the spread of SARS-CoV-2 [14]. Understandably, the early isolation and treatment of confirmed COVID-19 patients were of utmost importance. To minimise the impact of this rapidly spreading virus, on February 3, 2020, Wuhan decided to separate and treat patients on the basis of their condition. With this perspective, Fangcang Shelter hospitals were used to treat COVID-19 cases with mild-to-moderate symptoms, while designated hospitals were used to treat COVID-19 cases with severe and critical conditions [15,16]. In total, 14 gymnasiums and convention and exhibition centres located in Wuchang, Jianghan, Hongshan and Dongxihu districts were transformed into Fangcang Shelter hospitals with a total of 12,365 beds. As of March 10, 2020, approximately 12,000 patients with mild COVID-19 have been admitted to Fangcang Shelter hospitals in Wuhan, China. In a One Health perspective, the isolation and treatment of confirmed COVID-19 patients implemented in Fangcang Shelter hospitals engaged professionals from many disciplines, such as medicine, engineering, architecture, psychology, environmental health, and social sciences.
Theoretically, COVID-19 cases should be admitted to Fangcang Shelter hospitals over a short period of time, which should sufficient to control infection sources and treat patients at low cost but high efficiency [17,18]. However, the effects of Fangcang Shelter hospitals on the control of the COVID-19 outbreak during the implementation of the containment strategy in China have not yet been well evaluated. Therefore, to provide a reference for COVID-19 control in other countries, this study aimed to evaluate the effects of Fangcang Shelter hospitals on the epidemic trend of COVID-19 by using an interrupted time series analysis.
2. Methods
2.1. Materials and methods
Wuhan, the capital city of Hubei Province and the traffic hub of central China, has a population of 9,083,500. The containment strategy for COVID-19 in Wuhan was implemented from January 24, 2020 to March 16, 2020 and did not change except for the use of Fangcang Shelter hospitals on February 5, 2020.
3. Fangcang shelter hospitals
The Fangcang Shelter hospitals operated in Wuhan were designed according to the cabins used to carry out emergency medical care after the Wenchuan earthquake in 2008 and the Yushu earthquake in 2010 [19]. These hospitals serve as temporary quarantine hospital facilities.
Fangcang Shelter hospitals are temporary quarantine houses with healthcare facilities that take the Fangcang cabin as the carrier and integrate medical treatment and clinical technology functions [15,20]. Composed of medical treatment units, ward units and technical support units, Fangcang Shelter hospitals are mainly used in major disaster rescue, emergency support, interim medical services and other tasks [15,19]. With features such as good mobility, fast deployment and strong environmental adaptability, these improvised facilities are capable of undertaking emergency medical rescue tasks and are therefore valued by many countries [20].
In February 2020, to stop the spread of COVID-19, Wuhan converted several gymnasiums, convention and exhibition centres, sports centres, training centres, industrial park factories, vocational high schools and other venues into special quarantine facilities for patients with clinically mild-to-moderate symptoms of COVID-19 infection. Named Fangcang Shelter hospitals, these temporary quarantine hospital facilities have complete medical functions and can carry out basic medical treatment, disease monitoring, diagnosis and other clinical tasks. They also have a team of psychologists to provide counselling services to patients. Fangcang Shelter hospitals were established to reduce patient density in traditional hospitals, expand treatment capacity and control the community spread of the virus.
4. Datasets
The time series of observations of confirmed COVID-19 cases from January 16, 2020 to March 16, 2020 was obtained from the websites of the Bureau of Health (http://www.nhc.gov.cn/) and the Chinese Center for Disease Control and Prevention (http://2019ncov.chinacdc.cn/2019-nCoV/). The information collected included the number of confirmed cases in Wuhan, China.
Suspected cases were defined as people who had any of the epidemiological history criteria plus any two clinical manifestations or had all three clinical manifestations if there is no clear epidemiological history [21].
History of epidemiology:
-
1.
History of travel to or residence in Wuhan and its surrounding areas, travel to other communities in China where cases have been reported or travel to other countries/regions with severe outbreaks outside China within 14 days prior to the onset of the disease.
-
2.
Contact with an individual infected with SARS-CoV-2 (who tested positive with a nucleic acid test) within 14 days prior to the onset of the disease.
-
3.
Contact with patients with fever or respiratory symptoms from Wuhan, its surrounding areas, communities where confirmed COVID-19 cases have been reported or other countries/regions with severe outbreaks outside China within 14 days before the onset of the disease.
-
4.
Clustered cases (two or more cases with fever and/or respiratory symptoms in a small area, such as in families, offices, schools, workplaces and other gatherings within 14 days).
Clinical manifestations:
-
1.
Fever and/or respiratory symptoms.
-
2.
Radiographic imaging consistent with COVID-19 pneumonia.
-
3.
Normal or decreased White Blood Cell (WBC) count, or normal or decreased lymphocyte count in the early stages of illness.
A confirmed case was defined as a suspected case with one of the following etiological or serological pieces of evidence [21]:
-
1.
Real-time fluorescent reverse transcription polymerase chain reaction positive result for SARS-CoV-2 nucleic acid.
-
2.
Viral genetic sequence that is highly homologous to SARS-CoV-2.
-
3.
2019-nCoV virus-specific IgM and IgG detectable in serum, detectable SARS-CoV-2 virus-specific IgG or a fourfold increase in IgG between paired acute and convalescent sera.
Asymptomatic individuals were defined as those with etiological detection of SARS-CoV-2 in respiratory specimens or specific IgM detected in serum.
4.1. Statistical analysis
In our study, intervention was defined as the use of Fangcang Shelter hospitals. The effect of the intervention on new confirmed cases was analysed using interrupted time series analysis of the data collected between January 16, 2020 and February 4, 2020 as the pre-intervention and between February 5, 2020 and March 16, 2020 as the post-intervention. The intervention led to a level or slope change that could be explained by the interrupted time series analysis. In this study, the model of interrupted time series analysis was calculated using the following formula [22,23]:
where Yt represents the outcome variable over time point t, x1 represents the elapsed time since the start of the study, x2 is a dummy variable representing the intervention period (pre-intervention period = 0, post-intervention period = 1) and x3indicates an interaction term. β0 is the baseline level of the outcome variable, β1 indicates the slope of the outcome variable before the intervention, β2 represents the immediate-level change following the intervention and β3 indicates the slope change following the intervention.
The interrupted time series analysis was carried out using Stata 16 (StataCorp, College Station, TX, USA). Interrupted time series analysis was achieved by linear regression with Newey–West standard errors with a maximum lag of 1, which was then considered in the autocorrelation structure or the linear regressions with Prais using the generalised least-squares method to estimate the parameters. Errors were assumed to follow a first-order autoregressive process. All tests were two-sided, and a P value less than 0.05 was considered statistically significant.
The real-time reproduction number [R(t)] was the expected number of secondary cases that each infected individual would infect if the conditions remained as they were at time t. A Bayesian statistical framework was used to calculate R(t) based on the number of COVID-19 cases, the number of secondary cases, the serial interval and the five-day moving average [7,10,24]. R(t) and its 95% credible interval (CI) for the whole period were calculated using R version 3.6.2.
5. Results
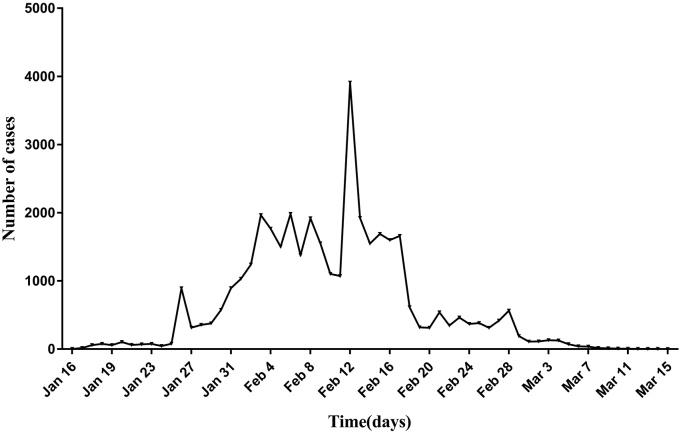
The number of new confirmed cases in Wuhan gradually increased to 3910 cases on February 13 and then slowly decreased (Fig. 1). In the first nine days after the implementation of Fangcang Shelter hospitals, the temporal number of confirmed cases significantly increased in Wuhan. On March 16, approximately 54 days from the start of the implementation of containment strategies, the terminal phase of COVID-19 was declared in Wuhan.
Fig. 1.
Numbers of new confirmed cases over time in Wuhan, China.
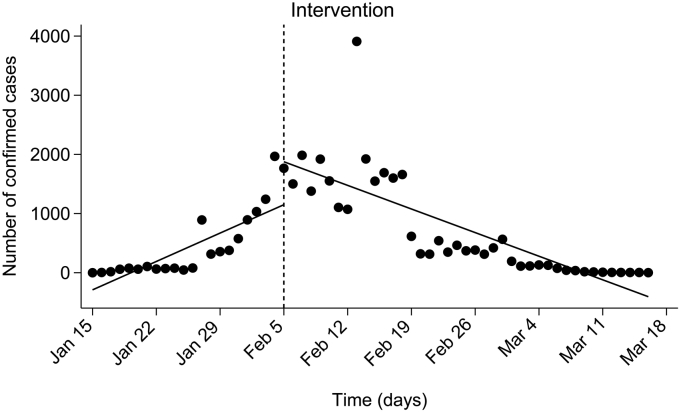
As shown in Fig. 2 and Table 1, the initial number of confirmed cases in Wuhan increased significantly by 68.54 cases per day (P < 0.0001; CI, 36.42–100.67) prior to February 4, 2020. In the first day of the intervention (February 5, 2020), a significant increase of 725.97 (P = 0.025; CI, 93.34–1358.59) in confirmed cases followed by a significant decrease in the daily trend of 125.57 cases (relative to the pre-intervention trend; P < 0.0001; CI, −160.44 to −90.69) were noted. Post-trend analysis demonstrated that the number of cases per day decreased annually in confirmed cases by 57.02 cases (P < 0.0001; CI, −71.28 to −42.77) after the operation of the Fangcang Shelter hospitals. It was estimated that the operation of the hospitals led to the prevention of 5148 cases (P < 0.0001; CI, −6578.04 to −3718.29). Furthermore, according to the mean confirmed cases of 395.71 per day before the intervention, we estimated that Wuhan had advanced the terminal phase of COVID-19 by 13 days.
Fig. 2.
Number of confirmed cases from January 16, 2020 to March 16, 2020 in Wuhan. The vertical dashed line indicates the time of the operation of Fangcang Shelter hospitals.
Table 1.
Interrupted time-series analysis of confirmed cases in Wuhan, China.a
| β | t | P | 95% CI | ||
|---|---|---|---|---|---|
| Pre-interventional trend | 68.54 | 4.28 | <0.0001 | 36.42 | 100.67 |
| level change | 725.97 | 2.30 | 0.025 | 93.34 | 1358.59 |
| Post-interventional trend change | −125.57 | −7.21 | <0.0001 | −160.44 | −90.69 |
| Baseline level | −289.73 | −2.11 | 0.039 | −564.09 | −15.36 |
| Treatedb | −57.02 | −8.01 | <0.0001 | −71.28 | −42.77 |
Regression with Newey-West standard errors.
Postintervention Linear Trend.
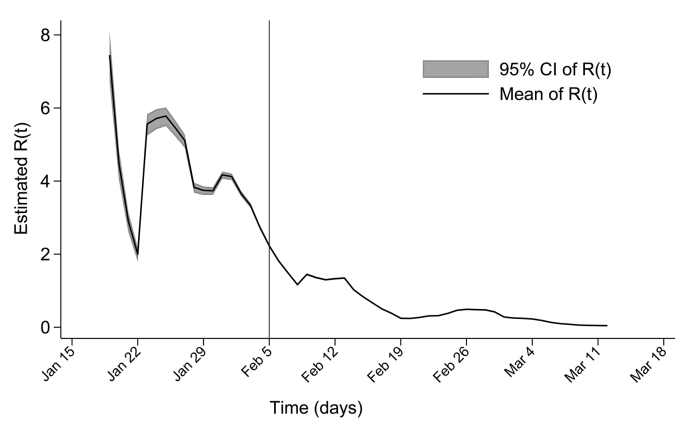
The mean real-time effective production number R(t) had the highest value at 7.45 (95%CI, 6.71–8.22) on January 19, 2020 and then decreased to 2.23 (95%CI, 2.18–2.28) on February 5, 2020. After February 6, 2020, R(t) was less than 2 and gradually decreased to less than 1 on February 15, 2020 (Fig. 3).
Fig. 3.
The mean real-time effective production number R(t) with 95% CI based on confirmed COVID-19 cases in Wuhan, China. The R(t) is defined as the mean number of secondary cases generated by a typical primary case at time t in a population, calculated for the whole period over a 5-day moving average. The horizontal line indicates R(t) = 1, below which sustained transmission is unlikely so long as antitransmission measures are sustained, indicating that the outbreak is under control. The gray area means the 95%CI of the mean real-time effective production number.
6. Discussion
Given the range of basic reproduction number of SARS-CoV-2, which lies between 1.50 and 6.68, person-to-person transmission of the disease can occur through respiratory droplets and close contact [6,24]. To reduce the risk of transmission and infection and the social impact of the epidemic, a containment strategy was implemented in Hubei Province, China. A containment strategy involves the use of medical and non-medical (lockdown, closures, suspensions, closures, etc.) intervention strategies and measures within a limited geographical area in the early stages of an emerging infectious disease epidemic [13]. Fangcang Shelter hospitals were a One Health approach for responding to the COVID-19 outbreak in Wuhan, China, and provided isolation, triage, basic medical care, frequent monitoring, rapid referral and essential living and social engagement for mild-to-moderate COVID-19 patients [15]. Although R(t) fluctuated from 2.00 to 7.45 in the pre-operation periods of Fangcang Shelter hospitals, it decreased gradually to less than 1 along with the implementation of the hospitals. This shift might be due to the use of Fangcang Shelter hospitals to control the infection sources of COVID-19.
In this study, we estimated the immediate and sustained change in the number of confirmed cases of COVID-19 over the pre- and post-operation periods of Fangcang Shelter hospitals in Wuhan. A sustained reduction and immediate increase in the number of cases were observed in Wuhan city after the Fangcang Shelter hospitals were established. These changes resulted in an estimated 5148 fewer confirmed cases in Wuhan. In this study, an initial evaluation of the effects of Fangcang Shelter hospitals on the control of COVID-19 was conducted using an interrupted time series analysis. According to the mean confirmed cases of 395.71 per day before the intervention, we estimated that Wuhan had advanced the terminal phase of COVID-19 by 13 days.
Among COVID-19 cases, 80% are mild, 20% may develop severe cases and a small percentage (5%) may become critically ill [25,26]. The exponential growth of COVID-19 cases in Wuhan posed a huge economic burden to local medical systems. If all COVID-19 cases were cared for in designated hospitals, then the shortage of medical resources would have collapsed the medical system in China. From a One Health perspective, China needed a novel approach to control the COVID-19 outbreak in Wuhan. The Fangcang Shelter hospitals rapidly established by converting low-cost stadiums and exhibition centres to isolate and care for COVID-19 cases with mild-to-moderate symptoms avoided the costly construction of new traditional hospitals for the admission and treatment of COVID-19 cases. Once the epidemic has been curbed, these public buildings can be restored to their original use, and the long-term and inefficient use of space is avoided. Compared to traditional hospitals, the Fangcang Shelter hospitals, with their centralised treatment of COVID-19 cases with mild-to-moderate symptoms, also required fewer doctors and nurses [27]. A key role of disease monitoring provided by Fangcang Shelter hospitals was to ensure that patients were timely transferred to designated hospitals if their conditions worsen. The hospitals also helped ensure that scarce medical resources, such as inpatient units providing respiratory support and intensive care centralised and supplied only in designated hospitals, could meet the demands of caring for severely ill patients and thus avoid wastage of medical resources.
Isolating COVID-19 cases is one of the most important measures of prevention and control strategies for COVID-19. It is almost impossible for COVID-19 cases to stay at home without having any close contact with their family members and other people in the community. Compared to isolation in Fangcang Shelter hospitals, home isolation is likely to lead to a rapid increase in the number of second- and third-generation cases and some community and family clustering of COVID-19 [28]. The sharply increasing number of COVID-19 may arouse much fear in the community and even be a direct challenge to the prevention and control strategies for COVID-19. In a One Health perspective, the Fangcang Shelter hospitals are more a community of patients than they are medical institutions; besides basic medical care, they provide shelter, accommodation, food, sanitation, hygiene and social engagement for individuals with COVID-19 [15]. In Fangcang Shelter hospitals, patients' recovery could be promoted and the anxiety from a COVID-19 diagnosis and isolation could be alleviated by the patients supporting one another and engaging in social activities. Of note, community activities such as eating together, reading, dancing, watching television and celebrating birthdays, all of which were supplied in Fangcang Shelter hospitals, may alleviate the anxiety from a COVID-19 diagnosis and isolation to some degree [29,30]. In addition, the involvement of psychiatrists makes it convenient for COVID-19 cases to obtain emotional support.
In the early period of the COVID-19 outbreak in Wuhan, many hospitals were not prepared for the tremendous treatment needs of patients. On February 5, 2020, the number of confirmed patients gradually decreased in Wuhan after the operation of Fangcang Shelter hospitals [15]. These findings suggest that the increased number of beds used in Fangcang Shelter hospitals may be beneficial for undiagnosed patients in the early stage of the disease. The linear fitting model also demonstrated that the downward trend of new confirmed cases in Wuhan after the operation of Fangcang Shelter hospitals is statistically significant. This change in trend reveals that the use of Fangcang Shelter hospitals played a crucial role in the control of COVID-19.
At present, the COVID-19 outbreak is sweeping through Italy (272,912 confirmed cases with 35,507 deaths), Spain (488,513 confirmed cases with 29,234 deaths), the USA (6,148,875 confirmed cases with 186,754 deaths) and Brazil (4,041,638 confirmed cases with 124,614 deaths) [3]. These countries are facing an exponential increase in the number of COVID-19 cases because of community outbreaks and the massive shortage of medical resources, both of which appeared in the early stage of the COVID-19 epidemic in Wuhan. However, approximately 41 days from the first use of Fangcang Shelter hospitals to March 16, the terminal phase of COVID-19 was declared in Wuhan. In China, most provinces outside of Hubei reported confirmed cases that were mostly imported cases from Wuhan, which spent about 30 days ending the COVID-19 epidemic. Therefore, besides a containment strategy, Fangcang Shelter hospitals are an available option to control the disease spread for countries with local epidemics.
This study presents several limitations. First, considering the lack of a randomised control in other areas that did not implement Fangcang Shelter hospitals, we could not estimate the parallel reduction in the number of patients and days in these areas before the end of the epidemic. However, from the macroscopic view, we estimate that the number of patients will decrease after the use of Fangcang Shelter hospitals during the implementation of the containment strategy in Wuhan. Second, in the early stage of the epidemic, the difference between the reported and real data could have influenced the parameter estimations in the models. The effects of Fangcang Shelter hospitals on preventing the spread of COVID-19 was only observed in Wuhan, although the containment strategy alone also resulted in dramatic reductions in COVID-19 cases in other provinces. Finally, considering the lack of data on suspected cases in Wuhan, estimating the effects of the Fangcang Shelter hospitals on limiting the number of suspected cases was not possible.
Fangcang Shelter hospitals are a One Health approach for responding to the COVID-19 outbreak in Wuhan, China, and have basic functions such as isolation, triage, medical care, disease monitoring and referral. In a One Health perspective, the Fangcang Shelter hospitals are more a community of patients than they are medical institutions, providing shelter, accommodation, food, sanitation, hygiene and social engagement for individuals with COVID-19. Interrupted time series analysis revealed that Fangcang Shelter hospitals were likely to reverse the epidemic trend of COVID-19 while the containment strategy was implemented in Wuhan. Therefore, these hospitals could be a key component of national responses to future epidemics and public health emergencies. The results of this study provide a valuable reference for health policy makers in countries where the COVID-19 outbreak has also spread.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Not applicable.
Funding
This work was supported by The National Natural Science Foundation of China (81871681), The National First-class Discipline Programme of Food Science and Technology (JUFSTR20180101), The Fundamental Research Funds for the Central Universities funded by the Ministry of Education of China (JUSRP51710A), and project of Wuxi Science and Technology Supporting Plan (N2020X004), The reserve top-notch talents project of "Double hundred" medical and health young and middle-aged in Wuxi in 2020, Mega-project of Wuxi Commission of Health (No. Z202007), The project of Bayesian statistical methods in the processing of complex vertical spatial-temporal big data funded by Yunnan Provincial Department of science and Technology Kunming Medical University (2018fe001 (-183)).
Author statement
YC had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. KW, JG, FC, YC conceived the study. KW, XS, HW, XZ, DH, QY, XW, and JH, FC designed the model, and JL made the figures. XL, and YC wrote the first draft of the manuscript. All authors interpreted the results, and approved the final version for submission.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgements
Not applicable.
Contributor Information
Feng Cheng, Email: fcheng@mail.tsinghua.edu.cn.
Yang Cheng, Email: woerseng@126.com.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU), https://coronavirus.jhu.edu/map.html, Accessed September 4 2020, 2020.
- 4.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fang Y., Nie Y., Penny M. Transmission dynamics of the COVID-19 outbreak and effectiveness of government interventions: a data-driven analysis. J. Med. Virol. 2020;92(6):645–659. doi: 10.1002/jmv.25750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu Y., Gayle A.A., Wilder-Smith A., Rocklov J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J. Travel Med. 2020;27(2) doi: 10.1093/jtm/taaa021. (taaa021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sahu K.K., Mishra A.K., Lal A. Comprehensive update on current outbreak of novel coronavirus infection (2019-nCoV) Ann. Transl. Med. 2020;8(6):393. doi: 10.21037/atm.2020.02.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelly T.R., Karesh W.B., Johnson C.K., Gilardi K.V.K., Anthony S.J., Goldstein T. One Health proof of concept: bringing a transdisciplinary approach to surveillance for zoonotic viruses at the human-wild animal interface. Prev. Vet. Med. 2017:112–118. doi: 10.1016/j.prevetmed.2016.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sikakulya F.K., Mulisya O., Munyambalu D.K., Bunduki G.K. Ebola in the eastern Democratic Republic of Congo: one health approach to infectious disease control. One Health. 2020;9 doi: 10.1016/j.onehlt.2019.100117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan A., Liu L., Wang C., Guo H., Hao X., Wang Q. Association of Public Health Interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1–9. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El Z.M., Jarhult J.D. From SARS to COVID-19: a previously unknown SARS- related coronavirus (SARS-CoV-2) of pandemic potential infecting humans - Call for a One Health approach. One Health. 2020;9 doi: 10.1016/j.onehlt.2020.100124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lancet The. COVID-19: fighting panic with information. Lancet. 2020;395(10224):537. doi: 10.1016/S0140-6736(20)30379-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lai S., Ruktanonchai N.W., Zhou L., Prosper O., Luo W., Floyd J.R. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020 doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shang L., Xu J., Cao B. Fangcang shelter hospitals in COVID-19 pandemic: the practice and its significance. Clin. Microbiol. Infect. 2020;26(8):976–978. doi: 10.1016/j.cmi.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen S., Zhang Z., Yang J., Wang J., Zhai X., Bärnighausen T. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305–1314. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fang D., Pan S., Li Z., Yuan T., Jiang B., Gan D. Large-scale public venues as medical emergency sites in disasters: lessons from COVID-19 and the use of Fangcang shelter hospitals in Wuhan, China. BMJ Glob. Health. 2020;5(6) doi: 10.1136/bmjgh-2020-002815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hellewell J., Abbott S., Gimma A., Bosse N.I., Jarvis C.I., Russell T.W. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob. Health. 2020;8(4):e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Travel Med. 2020;27(2) doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Medical Administration and Administration, Medical Management and Service Guidance Center, National Health Commission of The People’s Republic of China . Third edition. 2020. The Working Manual of Medical Cabins. (On February 22) [Google Scholar]
- 20.Martin-Gill C., Doyle T.J., Yealy D.M. In-flight medical emergencies: a review. JAMA. 2018;320(24):2580–2590. doi: 10.1001/jama.2018.19842. [DOI] [PubMed] [Google Scholar]
- 21.Chinese Centre for Disease Control and Prevention Diagnosis and Treatment, COVID-19 Prevention and Control. February 17, 2020. http://www.chinacdc.cn/en/COVID19/202002/P020200310326343385431.pdf Accessed March 22, 2020.
- 22.Linden A. Challenges to validity in single-group interrupted time series analysis. J. Eval. Clin. Pract. 2017;23(2):413–418. doi: 10.1111/jep.12638. [DOI] [PubMed] [Google Scholar]
- 23.Bernal J.L., Cummins S., Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int. J. Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tang B., Bragazzi N.L., Li Q., Tang S., Xiao Y., Wu J. An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov) Infect. Dis. Model. 2020;5:248–255. doi: 10.1016/j.idm.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.WHO Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) Feb 28, 2020;2020 https://www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19) [Google Scholar]
- 26.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 27.China Daily Medical Teams Sent to Wuhan Play Key Role. Feb 21, 2020. http://epaper.chinadaily.com.cn/a/202002/21/WS5e4f0f6ca310a2fabb7a256f.html
- 28.Li C., Li H., Li Q., Li D., Guan X., Wu J.T. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.China News Wuhan's Coronavirus Patients Dance Away Pains in Makeshift Hospital. Feb 11, 2020. http://www.ecns.cn/news/society/2020-02-11/detail-ifztmcih6521787.shtml
- 30.Beijing Daily A Patient From Fangcang Shelter Hospital has Recorded her Life in Fangcang (in Chinese) Feb 23, 2020. http://www.bjd.com.cn/a/202002/23/WS5e526c63e4b05998c6eb7747.html (accessed August 2, 2020)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.