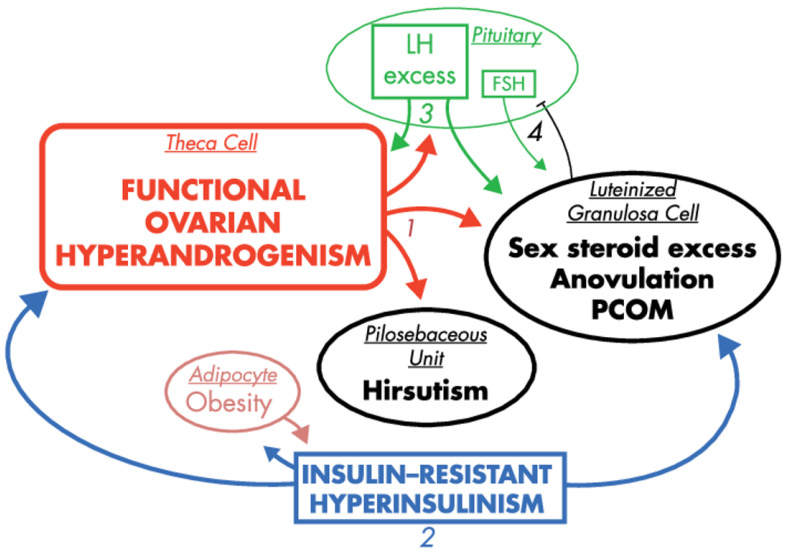
Figure 3.
The effects of hyperinsulinemia in the context of PCOS pathogenesis, reprinted and captioned from [42] with permission of the Oxford University Press. Ovarian hyperandrogenism is nearly universal in PCOS and can account for all the cardinal clinical features of the syndrome: hyperandrogenemia, oligo-anovulation and polycystic ovaries (1). About half of patients with functional ovarian hyperandrogenism have insulin-resistant hyperinsulinism (2). Insulin-resistant hyperinsulinism acts on theca cells to aggravate hyperandrogenism, synergizes with androgen to prematurely luteinize granulosa cells and stimulates adipogenesis. The increased hyperandrogenemia provokes LH excess (3), which then acts on both theca and luteinized granulosa cells to worsen hyperandrogenism. LH also stimulates luteinized granulosa cells to secrete estradiol (4), which suppresses FSH secretion. These hyperinsulinism-initiated changes in granulosa cell function further exacerbate PCOS and further hinder ovulation. Obesity increases insulin resistance, and the resultantly increased hyperinsulinism further aggravates hyperandrogenism. Heaviness of lines and fonts represents severity. Both functional ovarian hyperandrogenism and insulin resistance typically have an intrinsic basis. This model does not exclude the possibility that the unknown intrinsic ovarian defects that underpin the ovarian steroidogenic dysfunction also involve granulosa cell folliculogenesis. The figure also does not depict other associated defects, such as the functional adrenal hyperandrogenism that often accompanies the ovarian hyperandrogenism and the contribution of excess adiposity to peripheral androgen production and gonadotropin suppression.