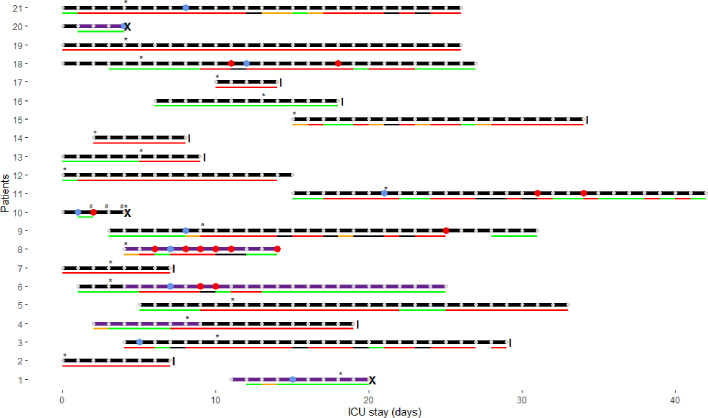
Fig. 1.
Clinical characteristics of study patients. Horizontal lines with dots represent the follow-up period for each patient; those lines end with a vertical line when the patient was discharged from the ICU and with a cross when he died (from a suspected massive pulmonary embolism (PE), from an ischemic stroke and from bleeding and thrombotic complications in the setting of overt disseminated intravascular coagulopathy (DIC)). Blue dots indicate thrombosis diagnosis (five deep vein thrombosis (DVT), two PE – or thrombosis within pulmonary arteries, one DVT + PE, two ischemic strokes) and red dots represent major bleeding events (i.e. gluteal hematoma requiring two embolizations, intracranial bleeding secondary to thrombolysis, subacute cerebral hematoma, diffuse multiple bleeding requiring blood transfusions and two iatrogenic bleeds – due to an ECMO cannula and to a rectal cannula). Bottom lines represent the degree of anticoagulation actually achieved according to anti-Xa plasma levels measured daily (IU/mL - heparin anti-Xa activity; STA-Liquid anti-Xa; does not contain dextran): excessive in black (i.e. >0.7 for UFH or >1.4 for enoxaparin); increased doses in red (i.e. 0.3–0.7 for UFH or 0.5–1.4 for enoxaparin); prophylactic doses in green (i.e. 0.1–0.3 for UFH or 0.1–0.5 for enoxaparin); orange if unknown (LMWH without peak measurement). The implementation of GIHP guidance [3] is marked with an asterisk: patients deemed at high thrombotic risk were anticoagulated using intermediate doses of heparins (i.e. enoxaparin 1 mg/kg/day; or unfractionated heparin (UFH) for an anti-Xa target between 0.3 and 0.5 IU/mL), and patients at very high risk were anticoagulated with therapeutic doses (i.e. enoxaparin 1 mg/kg twice daily; or UFH for an anti-Xa target between 0.5 and 0.7 IU/mL). The LMWH enoxaparin was preferentially used; UFH was administered if renal failure, extracorporeal oxygen membrane oxygenation (ECMO), or high bleeding risk (e.g. after recent invasive procedure). Overt DIC was present in one patient, represented on the figure by a hash. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)