INTRODUCTION
Nurses play a central role in delivering palliative care, given their influence on the quality of care provided (Montgomery, Sawin, & Hendricks-Ferguson, 2016). They are professionals of choice when it comes to assessing disease symptoms or psychological distress, ensuring symptoms are managed effectively, as well as accompanying patients and families through the decision-making process regarding both adult and pediatric care (Contro, Larson, Scofield, Sourkes, & Cohen, 2004). Optimal palliative care practices can prevent or alleviate the suffering of patients of all ages at the end of life, particularly if the care includes the assessment of symptoms and provides the patient and his or her family with psychological and social support (Qaseem et al., 2008). Although the majority of patients receiving palliative care are adults, more than 4,000 children in Canada have an incurable disease for which they will require quality palliative care (Widger, Cadell, Davies, Siden, & Steele, 2012). However, a number of studies carried out with nurses have revealed that they experience anxiety with regard to the pediatric palliative care (PPC) they deliver (Mullen, Reynolds, & Larson, 2015) and difficulties communicating with families of patients (Montgomery et al., 2017), as well as managing their emotions when they attend to a child who is at the end of life (Roberts & Boyle, 2005). Based on the first hypothesis suggested by Contro et al. (2004), such behaviour can be explained by a lack of knowledge regarding PPC.
Furthermore, the literature shows that the tools used to synthesize and transfer knowledge concerning PPC do not allow nurses to learn quickly and efficiently (Arenella, Yox, Eckstein, & Ousley, 2010; Contro et al., 2004; Morgan, 2009; Wiener et al., 2015). The impression of not being properly equipped results in feelings of anxiety and inadequacy among nurses (Contro et al., 2004; Kenny, Cargil, Hamilton, & Sales, 2016; Mullen et al., 2015; Smith & Gordon, 2009). This leads to staff nurses losing confidence in their ability to provide PPC, which can affect the quality of care offered (Montgomery et al., 2016). Giving access to training and clinical tools can increase their confidence in this regard (Contro et al., 2004), but professional training is generally geared towards adult at the end of life and not children (Canadian Hospice Palliative Care Association, 2006). Having access to a knowledge transfer (KT) strategy adapted to the context of PPC could allow nurses to build the confidence necessary to provide high-quality palliative care. One strategy is web-based healthcare training, as it appears flexible, accessible and an appropriate method for transferring information to nurses. The meta-analysis by Arenella, Yox, Eckstein, and Ousley (2010) showed that the use of information technologies (e.g., videos, webinars, online learning) is a very efficient strategy for improving the knowledge, competence, and behaviour of health professionals. No study on that strategy has been carried out with PPC nurses specifically, but the work of Morgan (2009) shows that 66% of nurses working in hospitals prefer to learn through videos. As such, Ruiz, Michael, and Leipzig (2006) and Wiener, Weaver, Bell, and Samson-Daly (2015) add that the advantage in using information technologies is that the learning process can be personalized and offer a flexible learning formula, thus allowing nurses to learn at their own pace and make connections to their own experiences. Wiener et al. (2015) suggest to make the knowledge easily accessible, for example, by sharing it on a web platform. Video training makes it possible to translate knowledge into practice by showing how to apply it. Another advantage of video training is its accessibility over a hospital’s intranet.
During an internship under the Master’s of Science in Nursing program, we developed a web-based training program using a knowledge transfer approach. This article presents the development and pilot test of the web-based PPC training developed for staff nurses working in a pediatric oncology unit.
FRAMEWORK: INTEGRATED KNOWLEDGE TRANSFER (KT) APPROACH
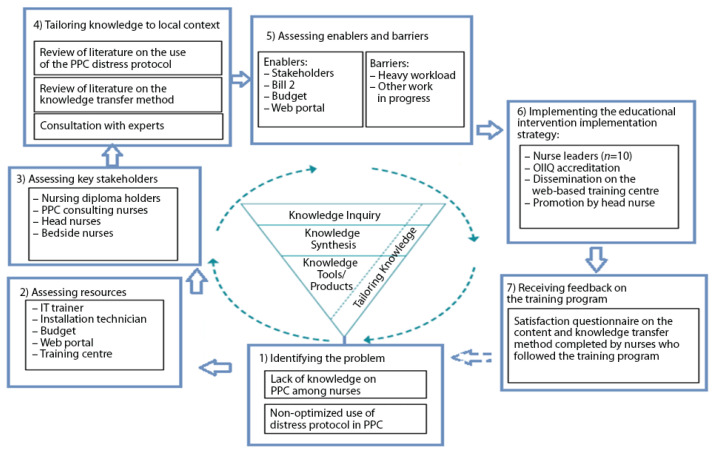
To create quality, evidence-based training, we used a knowledge transfer approach (Figure 1) derived from the KT model developed by the Registered Nurses’ Association of Ontario (RNAO) in 2012 and inspired by the work of Graham et al. (2006). The model, which supports an organized intervention (i.e., the web-based training), stresses the importance of synthesizing and adapting knowledge to develop an efficient KT strategy, while taking into account the resources available in the care setting, as well as the positive and negative factors of using that knowledge. The triangle at the centre of the model emphasizes the importance of the input of nurses in the creation of tailored training. In their study, Grimshaw et al. (2001) corroborate the importance of nurse participation, specifying that the more learners are involved in a project, the more their interest increases. Several activities based on the model were carried out in order to complete the project: (1) identifying the problem, (2) assessing the available resources, (3) assessing the key stakeholders, (4) tailoring knowledge to local context, (5) assessing enablers and barriers to knowledge use, (6) implementing a knowledge transfer strategy, and (7) receiving feedback on the strategy (web-based training).
Figure 1.
Knowledge Transfer Approach applied to the development of a web-based training
METHODOLOGY
Care settings, participants and recruitment
The internship project was developed in collaboration with the pediatric palliative care unit at Centre hospitalier universitaire (CHU) Sainte-Justine, in Montreal (Quebec, Canada). As nurses in the oncology sector provide more PPC than in other units, the program targeted that specific sector. The nurses participated in the project voluntarily, according to their availability (n = 30). The partners involved in the development and testing of the web-based training project were pediatric palliative care nurses (n = 2), head oncology nurses (n = 2), palliative care specialists (n = 2), head palliative care nurses (n = 1), and an executive oncology consultant, as well as the hospital’s nursing directorate.
Development of the online training program using a KT approach
Step 1) Identifying the problem
First, as suggested in the RNAO model of 2012, with the help of a number of nurses in the field, a more specific problem with regard to a lack of knowledge in PPC among nurses was ascertained. To come to that realization, two steps were carried out: explore the training required and target what is needed as a priority.
Exploring training needs
First, consultations with nurses (e.g., consulting nurses, unit heads) were held in order to explore PPC training needs. Shadowing was also part of the procedure, which made it possible to meet with various professionals and observe interactions with pediatric patients. These exchanges were key in bringing to light topics pertaining to PPC, such as respiratory distress management, the use of distress protocol, end-of-life signs and symptoms, introducing families to palliative care, the coexistence of curative and palliative care and the transition from curative to palliative care. These themes are consistent with the evidence available on the knowledge of PPC to be developed (see Table 1).
Table 1.
Content of the web-based training program on PPC-related distress
| Themes | Content | Strategies | Evidence |
|---|---|---|---|
| 1) Protocol relevancy |
|
|
Bidet et al. (2016), NICE (2017) |
| 2) Identifying pediatric distress | Various forms of distress:
|
|
Bidet et al. (2016), Pickstock (2017), Brennan & Mazanec (2011), INESSS (2017) |
| 3) Medication used |
|
|
Brennan et al. (2011), Wilson et al. (2015), Smothers & Beck (2012), NICE (2017) |
| 4) Route of administration |
|
|
INESSS (2017) |
| 5) Nurse’s roles |
|
|
Bidet et al. (2016), Bloomer et al. (2015), Bobb (2016), INESSS (2017) |
Determining priorities regarding training needs
A survey was later emailed to nurses working in the oncology unit of hospitals. The survey, which concerned all three nursing work shifts as well as oncology outpatient care, asked them to rate on a five-point Likert scale, the training needs previously established, with 1 representing “high priority” and 5 “low priority.” Of the 32 nurses who participated in the survey, 67% agreed that the application of a PPC distress protocol was of high priority, with 64% agreeing that patients and their families should be followed up closely. More than 67% of the nurses who completed the survey had more than five years of experience.
Steps 2) and 3) Assessing resources and key stakeholders
An assessment of the various resources available in the field of caregiving was carried out. One of the facility’s IT trainers participated in the project by adding an interactive component to the web-based training program, i.e., sound effects, images and video demonstrations. In addition, the hospital’s nursing directorate and the PPC unit allotted a budget for the project.
Step 4) Tailoring knowledge to local context
The use of the PPC distress protocol was reviewed in order to design an evidence-based training scenario. To make that possible, a literature review strategy was developed in collaboration with health science librarians, head oncology and clinical PPC nurses in order to pinpoint the most pertinent elements to the practice. The searches were mainly done on CINAHL, with an additional search on Google Scholar and Pubmed using the following search words: nursing, best practices, distress protocol, palliative care, pediatrics. The evidence review was used to create the web-based training program and organize it under five key themes (see Table 1). Furthermore, the content was approved by three expert professionals in the field of PPC (material available in the field, consistency with existing practices, feasibility). The web-based training program also integrates pedagogical strategies such as the use of images, sound effects, video demonstrations and real-life professional situations. Based on Mayer’s study (2003), learners are better able to remember messages when words are supported by pictures. In addition, Tomey (2003) suggests that students learn better through activities that require active participation, such as real-life situations, reflection or problemsolving.
Step 5) Assessing enablers and barriers
Several enablers helped to deliver the educational intervention. First, the collaboration of several important stakeholders in the project, such as head nurses, bedside nurses, and the nursing directorate, as well as a team of PPC consultants, helped in developing and promoting a valid and reliable product adapted to care setting. Furthermore, the budget the institution allotted for the intervention ensured the creation of a quality product. Since the Act respecting end-of-life care came into force, healthcare institutions have been required to implement measures offering optimal palliative care. Last, a web portal equipped with an online training centre was already accessible to nurses. Given that the main barrier was the heavy workload of staff nurses, the training program had to be short. A tab entitled “Palliative Care” was created in the hospital’s intranet, which allowed nurses to find the training program easily during any work shift.
Step 6) Implementing the knowledge transfer strategy
Head oncology nurses were asked to watch the training, so they could promote the program to nurses in their respective departments. Nurse managers can positively influence individuals and their organization by using the results derived from the research (Rycroft-Malone et al., 2002). In addition, 10 nurse leaders, known as “champions” in the hospitalization and oncology outpatient care units, were selected to participate in the training program. The purpose of the strategy was to foster the transmission of the knowledge acquired to their co-workers and promote the web-based training program. Note that a final strategy contributed to the KT: the accreditation of the training program by the Ordre des infirmières et infirmiers du Québec (OIIQ) for one hour of continuing education credits. Straus, Tetroe, and Graham (2013) support the strategy, stating that accreditation is a positive factor in the KT process.
Step 7) Receiving feedback on the web-based training program
A short feedback questionnaire was integrated into the end of the training (see Table 2). The questionnaire, specifically designed for the project, has not been validated, is made up of closed questions (yes or no answers) and has a box after each point for comments or suggestions. The results will be used to determine whether the web-based training program is an efficient way to transfer knowledge for future projects related to palliative and oncology care.
Table 2.
Feedback Questionnaire (n = 5)
| Questions | Number of participants who answered “Yes” | Example of comments |
|---|---|---|
| Do you feel that this training program will help you to adequately inform parents about the distress protocol guidelines? | 4 | “I would have liked more information on the protocol for families.” |
| Do you feel that this training program will help you to adequately identify pediatric distress? | 5 | “It gave me a better understanding of various situations and showed me how to apply the distress protocol.” |
| Do you feel that this training program will help you to know when you should implement the distress protocol? | 5 | “This is a good review of the distress protocol for experienced nurses and a good training for new nurses.” |
| Do you feel that this training program will help you to know better the different routes of the distress protocol? | 5 | “I didn’t know all the routes for the distress protocol.” |
| Which aspect(s) of the training program struck you the most? | N/A | “The protocol requires very good clinical judgment on the part of nurses.” “Assessing distress symptoms and implementing the protocol.” “How important it is to document properly.” “That one should not hesitate to provide quick relief.” |
| Do you feel that the format of the training program was conducive to learning? | 5 | “A few technical issues, but very enjoyable overall.” |
| Other comments/suggestions | N/A | “I liked how quizzes were used to assess comprehension during the training program.” |
Legend: N/A=not applicable
RESULTS
In total, 10 nurses working in the hospitalization and oncology outpatient care departments followed the web-based training program. However, only five of those nurses completed the questionnaire on their satisfaction. After viewing the program, all of them said they felt more prepared to inform parents of the distress protocol and able to recognize distress and apply the protocol in a timely and correct manner. Regarding the training format, the five nurses confirmed that the method used was appropriate for learning about PPC. Three participants said that they were particularly struck by the part on applying the distress protocol in the event of death rattles from a child, a stressful situation for the child, his or her family as well as for health professionals. Most of the nurses also appreciated that myths were debunked regarding injecting a child in distress with morphine. The comments showed that several of the myths surrounding PPC were debunked in the video and that the majority of nurses would like more information on PPC.
DISCUSSION
Changes in practices
After the pilot test of the training program, whose purpose was to transfer knowledge on PPC to nurses, the participating nurses said they felt better prepared to recognize distress and determine when and how to apply the protocol. It is noteworthy that roughly one in every three children in palliative care will experience episodes of dyspnea and intense pain, which places those symptoms among the most common in pediatrics palliative care (Vollenbroich et al., 2016). Those symptoms cause suffering for the child and have a long-lasting impact on the child’s family (Lützau et al., 2012; Vollenbroich et al., 2016). Episodes of distress tend to accentuate a nurse’s feeling of helplessness and anxiety about the conditions of a sick child, in particular when the nurse is unsure about the care to be provided (Deffner & Bell, 2005). This knowledge directly influences the quality of care offered; it has been shown that more anxious nurses limit contact with patients and families, which detrimentally affects the assessment and management of distress symptoms (Mullen et al., 2015). Acquiring knowledge on the subject could, therefore, alleviate feelings of anxiety and incompetence regarding PPC and, consequently, optimize the quality of care provided. It is important for nurses to be aware of their roles in accompanying families when the distress protocol is applied, hence the importance of their acquiring more knowledge on the subject. This knowledge represents only a small part of what is required for nurses to be confident in delivering PPC; the training program aims to be a trigger in this regard.
Comments were then provided on the various myths presented in the training program. The majority of nurses confirmed that the training program allowed them to demystify the belief that the distress protocol accelerated death. Based on the study by Bidet et al. (2016), 54% of respondents of a survey on the use of distress protocols believe that current protocols are not optimal, as they, at times, precipitate death. In addition, according to the nurses in that same study, the three main barriers to the protocol are the fear of going against the patient’s or family’s will, precipitating death, and poorly assessing the patient’s distress. The web-based training program addresses the two latter barriers for no other reason than to ensure children and families receive the best quality palliative care.
Nurses satisfaction regarding the training program
The improvement of PPC nursing practices through the appropriate use of the distress protocol can be explained by the fact that the nurses acquired knowledge through the various pedagogical methods used in the training program. According to the answers from participants, the web-based training program is a useful learning tool and a flexible method for transferring knowledge, which allowed them to make concrete links with their clinical practice. They also added that they appreciated the program’s accessibility, since it was available at any time during any work shift, as well as its 35-minute duration. Given the time constraints inherent to their work, it was even more important to find a training format optimized to their work environment. Generally speaking, the participants seem satisfied with the knowledge they acquired through KT.
Even though 10 participants followed the training program, only five of them took the time to answer the feedback questionnaire, which is likely due to an excessive workload and lack of time. The training program was done during work hours.
Strengths of the web-based training program
The program was found to have many strengths. With regard to the co-creation process and program pilot testing, the use of the RNAO’s KT model (2012) helped to organize the educational intervention and develop a product tailored to the needs of caregivers. The various steps outlined in the model helped to define the overarching issue, which is a lack of knowledge on PPC among nurses. In addition, the collaborative work with nurses led to a training program tailored to a specific care setting. A similar project was carried out at Stanford Hospital in California, fostering the enhancement of nurses’ knowledge and an improvement of their attitude and overall competence regarding the delivery of palliative care. The impacts noted included an increase in the quality of care and a decrease in the feeling of helplessness among parents (Petersen et al., 2016).
The selected video format is also positive: the use of information and communication technologies improves learning environments by creating a link between theory and practice, even in cases of distance learning (Dunn, 2000; Hall, 2009; Laferrière & Gervais, 2008). For nurses, it is a good way to learn at their pace (Wiener et al., 2015), is considered more flexible and accessible, and fosters the integration of information and communication technologies in learning and teaching (Brown, Kirkpatrick, Mangum, & Avery, 2008).
Finally, among the strengths is the training program’s interactive dimension. In the field of teaching, all educative strategies other than lectures are often considered innovative. However, innovation is also mentioned where the teaching strategy is based on interactivity between the user and an information system in situations whose purpose is to improve the learner’s learning experience (Dubois & Giroux, 2012). In the context of interactive educational interventions, authentic content is presented, thus encouraging the learner to listen and engage in the learning process (Tinio, 2002). According to Cabana et al. (1999), lack of motivation is an obstacle when it comes to changing behaviour regarding healthcare. Professionals need to be informed, motivated and trained to use evidence in their daily work (Grol & Wensing, 2004). Web-based training programs must include various strategies (e.g., assertions to rectify, real-life situations, video demonstrations) to create interactivity and allow for a connection between learning and practice (Arenella et al., 2010).
The limits of web-based training
First, although data records have been validated with various experts in the field of PPC, no such action has been taken with staff nurses. Consulting staff nurses would have been an asset in the development of the educational intervention and would likely have encouraged more nurses to participate. Since this study was an internship project, the timeline and program objectives restricted evaluation and, thus, only a few nurses were surveyed about their satisfaction with the training program. It would be relevant to conduct a formal assessment of the training program’s effects on nurses’ learning and on their practice in the field of PPC.
The use of only one KT method (not combined with another method) may hinder KT. The combination of several KT interventions may cover a wider spectrum of learning styles, which is a practice more likely to be efficient than isolated interventions (Bastable, 2014; Sinclair, Kable, & Levett-Jones, 2015). According to the results of the systematic review by Sinclair et al. (2015), a multimodal intervention may be necessary in KT, and preferable to a sole invention, in order to reduce the rate at which professionals require reminders. In addition, although useful through its flexibility and accessibility, a web-based training program is not the best strategy for including reflections and coaching. Personal reflections and team debriefings would ensure professional attendance and emotional coping (Anneser, Kunath, Krautheim, & Borasio, 2014). For example, the learning process could have been reinforced had the program been accompanied by a follow-up with nurses in the form of reflection on the subject presented. Discussion with other professionals, which at times brings about the realization that some perceptions, feelings or experiences are actually shared, helps change behaviour or attitudes, fostering a feeling of cohesion and reduced isolation (Bastable, 2014).
IMPLICATIONS FOR NURSING PRACTICES AND TRAINING
This web-based PPC training program could affect nursing practices and training at the institution in several ways. In addition to meeting training needs, the project could reduce anxiety related to PPC (Mullen et al., 2015), facilitate communication in palliative care (Montgomery et al., 2017), and contribute to emotional management (Roberts & Boyle, 2005) while ensuring quality palliative care. Web-based training seems to be a concrete tool for ensuring the transfer of theoretical knowledge to clinical practice (Sinclair et al., 2015) while allowing for the development of an evidence-based professional practice. Although this project represents only a part of the required training in PPC, it allows staff nurses to acquire independence and confidence when confronted by an episode of distress in a child at the end of his or her life. It can render it easier to provide care to a patient and his or her family and offer a better quality of nursing care.
CONCLUSION
This study highlights how research-based knowledge can be used to advance nursing care. Web-based training is a flexible and accessible means of informing oneself on a sensitive subject such as PPC. Nurses, who play a vital role in providing pediatric palliative care, appear to experience anxiety when it comes to delivering that type of care. To be recognized, nurses are required to update their knowledge on the proven practices in pediatric palliative care. They can, as such, promote those practices, thus ensuring patients and patients’ families are receiving the best possible care.
ACKNOWLEDGMENTS
We would like to thank all individuals at CHU Sainte-Justine who took part in the project. We would also like to acknowledge the financial support received in bursaries awarded to the MCN by the Ordre régional des infirmières et infirmiers de la Montérégie (ORIIM) and the Nursing Faculty at the Université de Montréal.
REFERENCES
- Anneser J, Kunath N, Krautheim V, Borasio GD. Needs, expectations, and concerns of medical students regarding end-of-life issues before the introduction of a mandatory undergraduate palliative care curriculum. Journal of Palliative Medicine. 2014;17(11):1201–1205. doi: 10.1089/jpm.2013.0614. [DOI] [PubMed] [Google Scholar]
- Arenella C, Yox S, Eckstein DS, Ousley A. Expanding the reach of a cancer palliative care curriculum through web-based dissemination: A public–private collaboration. Journal of Cancer Education. 2010;25(3):418–421. doi: 10.1007/s13187-010-0066-1. [DOI] [PubMed] [Google Scholar]
- Bastable SB. Nurse as educator: Principles of teaching and learning for nursing practice. 4th ed. Burlington: MA: Jones & Bartlett Learning; 2014. [Google Scholar]
- Bidet G, Daoust L, Duval M, Ducruet T, Toledano B, Humbert N, Gauvin F. An order protocol for respiratory distress/acute pain crisis in pediatric palliative care patients: medical and nursing staff perceptions. Journal of Palliative Medicine. 2016;19(3):306–313. doi: 10.1089/jpm.2015.0100. [DOI] [PubMed] [Google Scholar]
- Bloomer M, O’Connor M, Copnell B, Endacott R. Nursing care for the families of the dying child/infant in paediatric and neonatal ICU: Nurses’ emotional talk and sources of discomfort. A mixed methods study. Australian Critical Care. 2015;28:87–92. doi: 10.1016/j.aucc.2015.01.002. [DOI] [PubMed] [Google Scholar]
- Bobb B. Dyspnea and delirium at the end of life. Clinical Journal of oncology Nursing. 2016;20(3):244–246. doi: 10.1188/16.CJON.244-246. [DOI] [PubMed] [Google Scholar]
- Brennan C, Mazanec P. Dyspnea management across the palliative care continuum. Journal of Hospice and Palliative Nursing. 2011;13(3):130–139. doi: 10.1097/NJH.0b013e3182148314. [DOI] [Google Scholar]
- Brown ST, Kirkpatrick MK, Mangum D, Avery J. A review of narrative pedagogy strategies to transform traditional nursing education. Journal of Nursing Education. 2008;47(6):283–286. doi: 10.3928/01484834-20080601-01. [DOI] [PubMed] [Google Scholar]
- Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR. Why don’t physicians follow clinical practice guidelines? A framework for improvement. Journal of American Medical Association. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- Canadian Hospice Palliative Care Association. Pediatric Hospice Palliative Care. 2006. https://www.chpca.net/media/7841/Pediatric_Norms_of_Practice_March_31_2006_English.pdf.
- Contro NA, Larson J, Scofield S, Sourkes B, Cohen HJ. Hospital staff and family perspectives regarding quality of pediatric palliative care. American Academy of Pediatrics. 2004;114(5):1248–1252. doi: 10.1542/peds.2003-0857-L. [DOI] [PubMed] [Google Scholar]
- Deffner J, Bell S. Nurses’ death anxiety, comfort level during communication with patients and families regarding death, and exposure to communication education: A quantitative study. Journal for Nurses in Professional Development. 2005;21:19–23. doi: 10.1097/00124645-200501000-00005. [DOI] [PubMed] [Google Scholar]
- Dubois S, Giroux M-N. L’innovation pédagogique chez les infirmières dans un contexte de début d’expérience professionnelle. Recherche en soins infirmiers. 2012;111:71–80. doi: 10.3917/rsi.111.0071. [DOI] [PubMed] [Google Scholar]
- Dunn N. L’innovation par la technologie et l’apprentissage : le défi d’un programme d’études à forte composante technologique : Réseau des Écoles Innovatrices (REI) du programme canadien Rescol 2000 [Google Scholar]
- Government of Canada. Advance Care Planning: the Glossary Project - Final Report. 2006. https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/palliative-care/advance-care-planning-glossary-project-final-report.html.
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, Robinson N. Lost in knowledge translation: Time for a map? Journal of Continuing Education in the Health Professions. 2006;26(1):13–24. doi: 10.1002/chp.47. [DOI] [PubMed] [Google Scholar]
- Grimshaw JM, Shirran L, Thomas R, Mowatt G, Fraser C, Bero L, Grilli R, Harvey E, Oxman A, O’Brien MA. Changing provider behavior: An overview of systematic reviews of interventions. Medical Care. 2001;39(8):112–145. [PubMed] [Google Scholar]
- Grol R, Wensing M. What drives change? Barriers to and incentives for achieving evidence-based practice. Medical Journal of Australia. 2004;180:57–60. doi: 10.5694/j.1326-5377.2004.tb05948.x. [DOI] [PubMed] [Google Scholar]
- Hall WA. Whither nursing education? Possibilities, panaceas, and problems. Nurse Education Today. 2009;29:268–275. doi: 10.1016/j.nedt.2008.09.005. [DOI] [PubMed] [Google Scholar]
- Institut national d’excellence en santé et services sociaux (INESSS) Protocol medical. 2017. https://www.inesss.qc.ca/fileadmin/doc/INESSS/Ordonnances_collectives/Detresse/INESSS-Protocole-medical-Detresse.pdf.
- Kenny G, Cargil J, Hamilton C, Sales R. Improving and validating children’s nurses communication skills with standardized patients in end of life care. Journal of Child Health Care. 2016;20(2):145–152. doi: 10.1177/1367493514555588. [DOI] [PubMed] [Google Scholar]
- Laferrière T, Gervais F. Teacher education and professional development : Ten years of ICT integration and what? Revista Electronica de Investigation Educativa. 2008;10:1–24. [Google Scholar]
- LégisQuébec. Loi concernant les soins de fin de vie. 2019. Récupéré à http://legisquebec.gouv.qc.ca/en/ShowDoc/cs/S-32.0001?langCont=fr.
- Lützau P, Otto M, Hechler T, Metzing S, Wolfe J, Zernikow B. Children dying from cancer: parents’ perspectives on symptoms, quality of life, characteristics of death, and end-of-life decisions. Journal of Palliative Care. 2012;28(4):274–281. [PubMed] [Google Scholar]
- Mayer RE. The promise of multimedia learning: using the same instructional design methods across different media. Elsevier. 2003;13(2):125–139. [Google Scholar]
- Montgomery K, Sawin KJ, Hendricks-Ferguson VL. Experiences of pediatric oncology patients and their parents at end of life: A systematic review. Journal of pediatric oncology nursing. 2016;33(2):85–104. doi: 10.1177/1043454215589715. [DOI] [PubMed] [Google Scholar]
- Montgomery K, Sawin K, Hendricks-Ferguson V. Communication during palliative care and end of life. Cancer Nursing. 2017;40(2):47–57. doi: 10.1097/NCC.0000000000000363. [DOI] [PubMed] [Google Scholar]
- Morgan D. Caring for dying children: Assessing the needs of the pediatric palliative care nurse. Journal of Pediatric Nursing. 2009;35(2):86–90. [PubMed] [Google Scholar]
- Mullen JE, Reynolds MR, Larson JS. Caring for pediatric patients’ families at the child’s end of life. Journal of Pediatric Care. 2015;35(6):4655. doi: 10.4037/ccn2015614. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE) End-of-life care for people living with life-limiting condition. 2017. Retrieved from https://www.nice.org.uk/guidance/qs13.
- Petersen C, Callahan MF, McCarthy DO, Hughes RG, White-Traut R, Bansal NK. An online educational program improves pediatric oncology nurses’ knowledge, attitudes, and spiritual care competence. Journal of Pediatric Oncology Nursing. 2016;34(2):130–139. doi: 10.1177/1043454216646542. [DOI] [PubMed] [Google Scholar]
- Pickstock S. Breathlessness at end of life: What community nurses should know. Journal of Cancer Nursing. 2017;31(5):74–77. [Google Scholar]
- Qaseem A, Snow V, Shekelle P, Casey DE, Cross JT, Owens DK, et al. Evidence-based interventions to improve the palliative care of pain, dyspnea, and depression at the end of life: A clinical practice guideline from the American College of Physicians. Annals Intern Medicine. 2008;148(2):141–146. doi: 10.7326/0003-4819-148-2-200801150-00009. [DOI] [PubMed] [Google Scholar]
- Registered Nurses Association of Ontario (RNAO) Toolkit: Implementation of best practice guidelines. 2nd ed. Toronto: Registered Nurses’ Association of Ontario; 2012. [Google Scholar]
- Roberts KE, Boyle LA. End-of-life education in the pediatric intensive care unit. Critical Care Nurse. 2005;25:51–57. [PubMed] [Google Scholar]
- Ruiz J, Michael J, Leipzig R. The impact of e-learning in medical education academic medicine. Journal of Cancer Education. 2006;81(3):207–212. doi: 10.1097/00001888-200603000-00002. [DOI] [PubMed] [Google Scholar]
- Rycroft-Malone J, Kitson A, Harvey G, McCormack B, Seers K, Titchen A, Estabrooks C. Ingredients for change: Revisiting a conceptual framework. Quality and Safety in Health Care. 2002;11(2):174–180. doi: 10.1136/qhc.11.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair P, Kable A, Levett-Jones T. The effectiveness of internet-based e-learning on clinician behavior and patient outcomes: A systematic review protocol. Journal of Continuing Education in the Health Professions. 2015;13(1):52–64. doi: 10.11124/jbisrir-2015-1919. [DOI] [PubMed] [Google Scholar]
- Smothers A, Buck J. An evaluation of a practice change to increase understanding of the use of nonpharmacological interventions for the treatment of dyspnea in hospice patients. Journal of Hospice and Palliative Nursing. 2012;14(8):524–532. doi: 10.1097/NJH.0b013e31825c7b2a. [DOI] [Google Scholar]
- Straus S, Tetroe J, Graham ID, editors. Knowledge translation in health care: moving from evidence to practice. Toronto, ON: John Wiley & Sons; 2013. [Google Scholar]
- Tinio V. ICT in education. 2002. Retrieved from http://wikieducator.org/images/f/ff/Eprimer-edu_ICT_in_Education.pdf.
- Tomey AM. Learning with cases. Journal of Continuing Education in Nursing. 2003;34:34–38. doi: 10.3928/0022-0124-20030101-07. [DOI] [PubMed] [Google Scholar]
- Vollenbroich R, Borasio GD, Duroux A, Grasser M, Brandstätter M, Führer M. Listening to parents: The role of symptom perception in pediatric palliative home care. Palliative Support Care. 2016;14:13–19. doi: 10.1017/S1478951515000462. [DOI] [PubMed] [Google Scholar]
- Widger K, Cadell S, Davies B, Siden H, Steele R. Pediatric Palliative Care in Canada. In: Knapp C, Madden V, Fowler-Kerry S, editors. Pediatric Palliative Care: Global Perspectives. Springer; Dordrecht: 2012. [DOI] [Google Scholar]
- Wiener L, Weaver MS, Bell C, Sansom-Daly UM. Threading the cloak: Palliative care education for care providers of adolescents and young adults with cancer. Journal of Clinical Oncology Adolescent and Young Adults. 2015;5:1–18. doi: 10.2147/COAYA.S49176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson E, Morbey H, Brown J, Payne S, Seale C, Seymour J. Administering anticipatory medications in end-of-life care: A qualitative study of nursing practice in the community and in nursing homes. Journal of Palliative Medicine. 2015;29:60–70. doi: 10.1177/0269216314543042. [DOI] [PMC free article] [PubMed] [Google Scholar]