Figure 2.
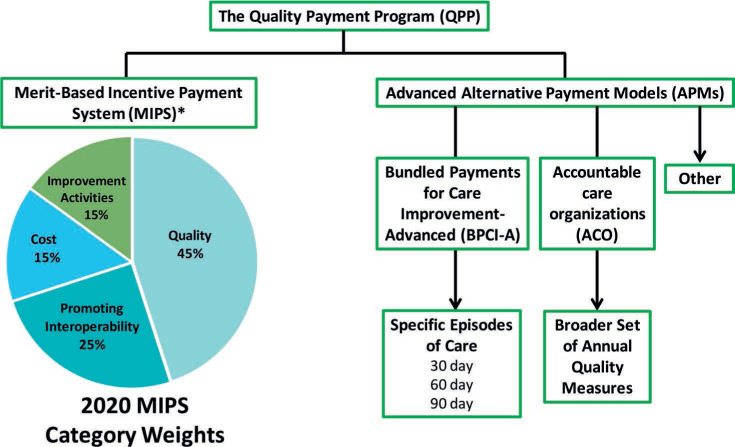
Diagram of the components within the Quality Payment Program (QPP). The QPP is composed of the Merit-Based Incentive Program (MIPS) and Alternative Payment Models (APMs). MIPS is the default program for clinicians and is composed of the following four elements (2020 weights reported): Quality 45%, Promoting Interoperability 25%, Cost 15%, Improvement Activities 15%. Clinicians can opt out of MIPs if they are enrolled in a qualifying APM; within cardiovascular care, this could mean either participating in an accountable care organization or being part of an organization that is participating in the Bundled Payments for Care Improvement-Advanced program.
