Dear Editor
World Health Organization (WHO) first declared coronavirus disease 2019 (COVID-19) as a pandemic in March 2020, and now, four months after that, the number of positive and death cases are still increasing. This global pandemic has caused a significant impact on health, social, and economic aspects around the world. Thus, identification of the risk factors that contribute to the development of severe infections is important to enabling risk stratification, optimizing the hospital resources reallocation, and guiding public health recommendations and interventions. During normal times, individuals with dementia are the most vulnerable persons as things depend on other people for their day to day survival. In a previous study, it has been shown that dementia increases the risk of morbidity and mortality among hospitalized patients, including the severity of the respiratory disease.1 Unfortunately, until now, no study provides clear evidence regarding the link between dementia and COVID-19. This article aims to explore the potential association between dementia and the severity of COVID-19 infection.
A search of the literature was conducted on PubMed and PubMed Central (PMC) using the keywords “dementia” OR “clinical characteristics” OR “comorbidities” OR “risk factors” AND “coronavirus disease 2019” OR “COVID-19”, between 2019 and present time (July 14th, 2020) with language restricted to English only. The title, abstract, and full text of all articles identified that matched the search criteria were assessed, and those reporting the rate of dementia in COVID-19 patients with a clinically validated definition of “severe disease” were included in this meta-analysis. The references of all identified studies were also analyzed (forward and backward citation tracking) to identify other potentially eligible articles.
A meta-analysis was performed using Review Manager 5.4 (Cochrane Collaboration) software. Dichotomous variables were calculated using the Mantel-Haenszel formula with random-effects models regardless of its heterogeneity. The effect estimate was reported as risk ratio (RR) along with its 95% confidence intervals (CIs) for dichotomous variables, respectively. P-value was two-tailed, and the statistical significance was set at ≤0.05.
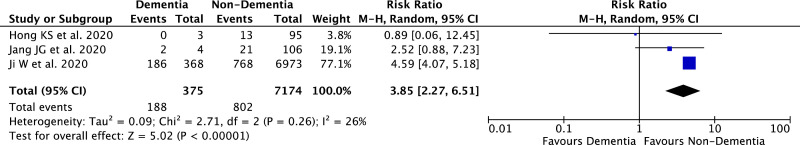
A total of 32,509 records were obtained through systematic electronic searches and other ways. After screening titles, abstracts, and full texts, 3 studies2, 3, 4 with a total of 7,549 COVID-19 patients were included in the meta-analysis (Table 1 ). The individual and pooled RRs for dementia predicting severe COVID-19 is shown in Figure 1 . Our pooled analysis showed that dementia is significantly associated with an increased risk of severe COVID-19 [RR 3.85 (95% CI 2.27–6.51), p < 0.00001, I 2 = 26%, random-effect modelling].
TABLE 1.
Characteristics of included studies
| Study | Sample size | Design | Severe patients |
Non-severe patients |
||
|---|---|---|---|---|---|---|
| n (%) | Age (years) | n (%) | Age (years) | |||
| Hong KS et al.2 2020 | 98 | Retrospective cohort | 13 (13.2%) | 63.2 ± 10.1 | 85 (86.8%) | 54.2 ± 17.7 |
| Jang JG et al.3 2020 | 110 | Retrospective cohort | 23 (25%) | 68.0 ± 11.9 | 87 (75%) | 53.9 ± 17.0 |
| Ji W et al.4 2020 | 7341 | Case control | 954 (13%) | 59.6 ± 56.2 | 6387 (87%) | 54.0 ± 60.7 |
Figure 1.
Forest plot that demonstrates the association of dementia with severe COVID-19 disease. Events mean a severe outcome of the disease.
Based on our pooled analysis of available data, dementia seems to be associated with an enhanced risk of severe COVID-19 infection. Several reasons can be proposed to explain this result. First, most of the patients with dementia were old and have other comorbid medical conditions that could increase the severity of infections. Older patients with COVID-19 infection tend to present with atypical symptoms. They may be afebrile with non-respiratory symptoms, such as delirium or isolated functional decline without any obvious physical symptoms.5 These atypical presentations of COVID-19 may impede the early recognition of the disease, increase COVID-19 spread, and mortality. Moreover, in a meta-analysis of 3027 COVID-19 patients, age over 65 years was found to be a risk factor for disease progression and the presence of underlying comorbid diseases were significantly higher in critical/mortal patients when compared to the non-critical patients.6 Second, patients with dementia were associated with the ApoE e4 genotype.7 ApoE itself has lipoprotein function and modulates the macrophage pro/anti-inflammatory phenotypes8 and is expressed by many cell types in the lung, including macrophages, type I and type II alveolar epithelial cells9, therefore it is possible that having one or two copies of ApoE4 can increase the risk of having severe COVID-19 infection by robust innate immune response and cytokine storm that results in acute respiratory distress syndrome (ARDS). A study by Kuo et al.10 has demonstrated that patients with ApoE e4e4 more likely to have severe COVID-19 infections. Hence, patients with dementia should be given extra care and monitoring to minimize exposure to the virus. Physicians and caregivers should be engaged in close monitoring of dementia patients with suspected COVID-19, for early diagnosis and treatment to avoid severe infections. Finally, dementia should be regarded as an important factor in future risk stratification models for COVID-19.
Footnotes
Funding: None.
Declaration of competing interest: None.
Acknowledgment: None.
References
- 1.Liao KM, Lin TC, Li CY. Dementia increases severe sepsis and mortality in hospitalized patients with chronic obstructive pulmonary disease. Medicine (Baltimore) 2015;94(23):e967. doi: 10.1097/MD.0000000000000967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hong KS, Lee KH, Chung JH. Clinical features and outcomes of 98 patients hospitalized with SARS-CoV-2 infection in Daegu, South Korea: a brief descriptive study. Yonsei Med J. 2020;61(5):431–437. doi: 10.3349/ymj.2020.61.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jang JG, Hur J, Choi EY. Prognostic factors for severe coronavirus disease 2019 in Daegu, Korea. J Korean Med Sci. 2020;35(23):e209. doi: 10.3346/jkms.2020.35.e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ji W, Huh K, Kang M. Effect of underlying comorbidities on the infection and severity of COVID-19 in Korea: a nationwide case-control study. J Korean Med Sci. 2020;35(25):e237. doi: 10.3346/jkms.2020.35.e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.D'Adamo H, Yoshikawa T, Ouslander J. Coronavirus disease 2019 in geriatrics and long‐term care: the ABCDs of COVID ‐19. J Am Geriatr Soc. 2020;68(5):912–917. doi: 10.1111/jgs.16445. [DOI] [PubMed] [Google Scholar]
- 6.Zheng Z, Peng F, Xu B. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020;(20):30234–30236. doi: 10.1016/j.jinf.2020.04.021. S0163-4453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuo C, Pilling LC, Atkins JL. ApoE e2 and aging-related outcomes in 379,000 UK biobank participants. Aging (Albany NY) 2020;12:12222–12233. doi: 10.18632/aging.103405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tudorache I, Trusca V, Gafencu A. Apolipoprotein E - a multifunctional protein with implications in various pathologies as a result of its structural features. Comput Struct Biotechnol J. 2017;15:359–365. doi: 10.1016/j.csbj.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gordon E, Yao X, Xu H. Apolipoprotein E is a concentration-dependent pulmonary danger signal that activates the NLRP3 inflammasome and IL-1β secretion by bronchoalveolar fluid macrophages from asthmatic subjects. J Allergy Clin Immunol. 2019;144(2):426–441. doi: 10.1016/j.jaci.2019.02.027. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuo CL, Pilling LC, Atkins JL. APOE e4 genotype predicts severe COVID-19 in the UK biobank community cohort. J Gerontol A Biol Sci Med Sci. 2020 doi: 10.1101/2020.05.07.20094409. glaa131. [DOI] [PMC free article] [PubMed] [Google Scholar]