Introduction
Treatment-resistant dermatophytosis caused by Trichophyton rubrum has emerged as a global public health threat, particularly in endemic areas like India. However, few, if any such cases, have been reported in the United States. We report a representative case and discuss our experience treating several patients with extensive T rubrum tinea corporis that persisted despite prolonged treatment with systemic and topical agents, including oral terbinafine. We have witnessed an increasing number of treatment-resistant cases in our clinic over the last 5 years, but to our knowledge, there are no reported cases in the United States.
Case report
A 45-year-old man with a history of portal vein thrombosis on apixaban anticoagulation and hereditary spherocytosis after splenectomy presented to our clinic for evaluation and management of a persistent fungal infection. The patient's symptoms started approximately 20 years before his presentation, at which time he reported disease that was initially limited to his toenails but progressed to involve his feet, thighs, groin, and buttocks. The patient had seen several dermatologists before his presentation and tried multiple therapies that failed, including transient or minimal improvement following oral terbinafine, topical naftifine, and topical steroids (last used several years prior). Given his recalcitrant dermatophytosis, the patient was referred to an immunologist and had an extensive immunodeficiency workup, which was unremarkable with the exception of low IgM antibody levels.
On initial examination in our clinic, the patient had onychomycosis of all toenails and diffuse, annular erythematous plaques with peripheral scale on his abdomen, lower back, and thighs. A potassium hydroxide test from a skin scraping found septate hyphae, and he was prescribed a 3-month course of terbinafine, 250 mg, and ciclopirox cream twice daily for tinea corporis and onychomycosis. Skin scrapings and toenail samples were collected and sent for culture and broth microdilution antifungal susceptibility testing as recommended by the Clinical and Laboratory Standards Institute, which showed T rubrum that was resistant to terbinafine (minimum inhibitory concentration [MIC] > 0.5 μg/mL) and sensitive to fluconazole (MIC < 0.03 μg/mL).1 At the patient's 3-month follow-up, he noted minimal improvement of his nail and skin disease after his course of terbinafine, and his examination findings were largely unchanged from those of his initial visit. We deferred starting itraconazole or fluconazole at this time given its contraindication (CYP3A4 inhibition) with apixaban and instead initiated griseofulvin ultramicrosized, 500 mg twice daily, with a plan for 1-month follow-up pending evaluation by his hematologist for alternative anticoagulation regimens. Upon completing 1 month of griseofulvin, the patient endorsed mild improvement, and his examination found limited clearance of the plaques on his flanks and buttocks. The patient was switched from apixaban to an alternative agent by his hematologist, and the decision was made to start treatment with itraconazole, 200 mg daily for 3 months.
Discussion
Superficial dermatophytoses are among the most common conditions prompting patients to seek dermatologic evaluation. The dermatophyte, T rubrum, is the most frequent cause of onychomycosis and cutaneous infection in the United States. Despite its prevalence, microbiologically proven drug resistance is rare and most patients improve with oral terbinafine. However, we have recently seen numerous cases of extensive tinea corporis from T rubrum that was initially resistant to terbinafine or recurred rapidly after a brief interval improvement. Although uncommon, these cases have been increasing in frequency, and we have seen several patients in our clinic with widespread cutaneous disease that persisted despite prolonged treatment with oral terbinafine or second-line systemic therapies (oral fluconazole or itraconazole). Treatment-resistant dermatophytosis has emerged as a public health threat in endemic areas like India.2, 3, 4, 5, 6 However, to the best of our knowledge, there have been no such cases of treatment-resistant dermatophytosis reported in the United States.
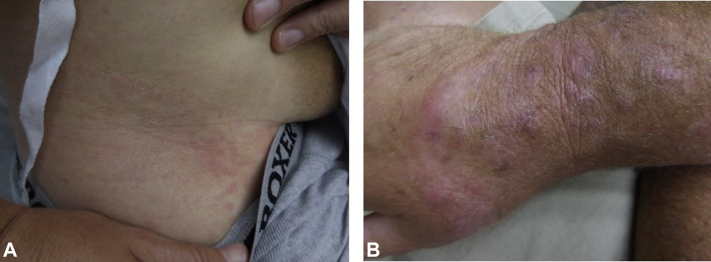
We have treated several cases of extensive and resistant T rubrum tinea corporis in otherwise healthy patients with no risk factors predisposing them to recurrent fungal infections including recent steroid use. Several patients did report a remote history of onychomycosis although most had no active nail involvement upon their initial presentation. A subset of patients initially responded to oral terbinafine and reported clearance within 2 weeks, although all noted recurrent and persistent lesions shortly after discontinuing treatment. Several patients, however, had no initial improvement with progressive disease while on therapy (Fig 1, A and B). Cultures from skin scrapings, in several cases, surprisingly resulted within a few days and showed T rubrum. Despite absence of clinical improvement, only some patients demonstrated terbinafine resistance on broth microdilution antifungal susceptibility testing (MIC > 0.5 μg/mL). Further workup including biopsies were unrevealing for inflammatory or alternative etiologies. Patients were switched to oral fluconazole or itraconazole in combination with topical agents. Most patients had partial improvement, although several had no clinical response despite continuous treatment on this alternative regimen.
Fig 1.
Persistent dermatophytosis of right thigh (A) and right dorsal hand and forearm (B).
Clinical resistance to standard antifungal therapies has been a concern, particularly in areas like India, which has observed an epidemic of terbinafine-resistant superficial mycoses caused by T rubrum and increasingly, Trichophyton mentagrophytes.7 This alarming trend has been attributed in part to the widespread availability and rampant use of over-the-counter, potent topical steroids often containing multiple antifungals and antibacterial agents, which results in a dysregulated immune response more susceptible to persistent dermatophyte infections.8 Although terbinafine-resistant strains of T rubrum secondary to genetic mutations in squalene epoxidase have been reported in the literature, microbiologically proven resistance has been uncommon in our experience, and most patients with persistent disease showed T rubrum that was sensitive to terbinafine on susceptibility testing. Indeed, studies in India have similarly found low incidence of in vitro terbinafine resistance in chronic T rubrum dermatophytosis.5,6 There are undoubtedly myriad host, pathogen, and environmental factors that contribute to the emergence of treatment resistance, and although the Indian epidemic provides some insight into this growing trend, additional research is needed to elucidate the mechanisms leading to clinical resistance in the United States and to develop effective treatments.4, 5, 6 We, therefore, report our experience with treatment-resistant dermatophytosis occurring in the United States with the aim of increasing domestic recognition of a developing global public health threat.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Clinical and Laboratory Standards Institute . 3rd ed. 2017. Reference Method for Broth Dilution Antifungal Susceptibility Testing of Filamentous Fungi. Document M38. [Google Scholar]
- 2.Majid I., Sheikh G., Kanth F., Hakak R. Relapse after oral terbinafine therapy in dermatophytosis: a clinical and mycological study. Indian J Dermatol. 2016;61(5):529–533. doi: 10.4103/0019-5154.190120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verma S., Madhu R. The great Indian epidemic of superficial dermatophytosis: an appraisal. Indian J Dermatol. 2017;62(3):227–236. doi: 10.4103/ijd.IJD_206_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma R., Adhikari L., Sharma R.L. Recurrent dermatophytosis: a rising problem in Sikkim, a Himalayan state in India. Indian J Pathol Microbiol. 2017;60(4):541–555. doi: 10.4103/IJPM.IJPM_831_16. [DOI] [PubMed] [Google Scholar]
- 5.Pathania S., Rudramurthy S.M., Narang T., Saikia U.N., Dogra S. A prospective study of the epidemiological and clinical patterns of recurrent dermatophytosis at a tertiary care hospital in India. Indian J Dermatol Venereol Leprol. 2018;84(6):678–684. doi: 10.4103/ijdvl.IJDVL_645_17. [DOI] [PubMed] [Google Scholar]
- 6.Saunte D.M.L., Hare R.K., Jørgensen K.M. Emerging terbinafine resistance in Trichophyton: clinical characteristics, squalene epoxidase gene mutations and a reliable EUCAST method for detection. Antimicrob Agents Chemother. 2019;63(10) doi: 10.1128/AAC.01126-19. e01126-e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nenoff P., Verma S.B., Vasani R. The current Indian epidemic of superficial dermatophytosis due to Trichophyton mentagrophytes—A molecular study. Mycoses. 2019;63(4):336–356. doi: 10.1111/myc.12878. [DOI] [PubMed] [Google Scholar]
- 8.Mukherjee P.K., Leidich S.D., Isham N., Leitner I., Ryder N.S., Ghannoum M.A. Clinical Trichophyton rubrum strain exhibiting primary resistance to terbinafine. Antimicrob Agents Chemother. 2003;47(1):82–86. doi: 10.1128/AAC.47.1.82-86.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]