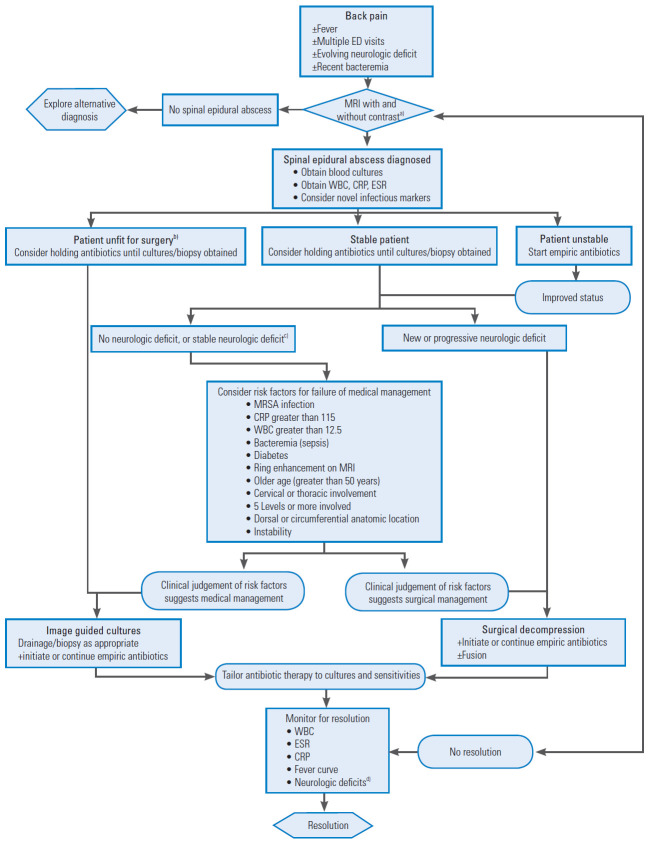
Fig. 3.
Generalized algorithm describing our preferred approach to the diagnosis and treatment of spinal epidural abscess. It is important to remember when considering this algorithm that time to diagnosis/treatment and the surgeons clinical experience weigh heavily on the optimal management of spinal epidural abscess. This algorithm represents a framework for the diagnosis and management of spinal epidural abscess not a ridged guideline. ED, emergency department; MRI, magnetic resonance imaging; WBC, white blood cell; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate. a)MRI with and without intravenous contrast of the entire spine is the authors preferred imaging modality. If a patient cannot undergo this study, an alternative study should be chosen. b)A patient may be considered unfit for surgery if he/she (1) refuses any operative intervention, (2) has considerable medical risk factors, which are determined with input from the anesthesiologists that the risks of surgical intervention outweigh the potential benefits, and (3) has a concurrent medical condition which requires urgent intervention that surpasses the spinal epidural abscess. c)Stable neurologic deficit may be any neurologic deficits that existed prior to the onset of the current disease process. Additionally, any new deficit which is stable may not necessitate operative intervention. Some surgeons may choose to treat neurologic deficits consistent with radiculopathy with initial medical management. Again, considerations of the timing of presentation, and the severity of disease are not covered in this algorithm and weigh heavily on the decision to procced. Finally, there is no substitute for a surgeon’s clinical experience in the management of spinal epidural abscess. d)New onset neurologic deficits after management is initiated or the worsening of deficits are important clinical signs that should be investigated thoroughly possibly with repeat imaging. If neurologic deficits do not resolve after treatment that is not necessarily a sign of failed management.