Abstract
Climate change has been described as the biggest global health threat of the 21st century. As a result, governments around the world are committing to legislative change in order to reduce greenhouse gas emissions (GHGEs). The healthcare sector makes a significant contribution to GHGEs and in line with national legislation in the UK, the NHS has recently committed to achieving net zero emissions by 2050. The management of asthma and COPD largely depends on the prescribing of medications that are delivered through inhalers. In the UK, the use of pressurized metered dose inhalers (pMDIs), which rely on hydrofluorocarbon (HFC) propellants accounts for 3.5% of the NHS’s total carbon footprint. In contrast, dry powder inhalers (DPIs) have a much lower carbon footprint due to the absence of a HFC propellant. Here we review evidence of the impact of inhaler choices across four domains: environmental impact, clinical effectiveness, cost effectiveness and patient preferences. We find that as well as a lower global‐warming potential, DPIs have additional benefits over pMDIs in other domains and should be considered first line where clinically appropriate.
Keywords: climate change, inhalers, sustainable prescribing
A comparison of dry powder inhalers (DPIs) and pressurised metered‐dose inhalers (pMDIs) across clinical, social and environmental domains.

1. INTRODUCTION
Climate change has been described as the “greatest threat to global public health in the 21st century”. 1 , 2 On 1 May 2019, the United Kingdom was the first country in the world to declare a “climate emergency” 3 in response to the Intergovernmental Panel on Climate Change report in 2018. The primary method for combating climate change is to reduce greenhouse gas emissions (GHGEs) 4 and the UK government has committed to achieving net zero GHGEs compared to a 1990 baseline by 2050. 5 , 6 In order to achieve this goal, a number of sectors will need to reduce their emissions. One of these sectors is the UK National Health Service (NHS), which is the UK’s largest public sector greenhouse gas emitter. 6 , 7 , 8 Importantly, around 3.5% of the NHS’s carbon footprint is derived from a single treatment ‐ pressurized metered dose inhalers (pMDIs) 8 , 9 , 10 , 11 which are used in the management of asthma and chronic obstructive pulmonary disease (COPD). The inhaler constituent responsible for 96% of pMDI’s global‐warming potential (GWP), is not the active ingredient but rather the propellant. 3 , 12 Dry powder inhalers (DPIs) which rely on a propellant‐free mechanism that significantly reduces the environmental impact of the prescription are the favored choice in a number of European countries 13 —although this is also due to nonenvironmental factors such as local manufacturing. A priority of the UK’s Sustainable Development Unit (SDU) strategy is to achieve an 80% reduction in NHS’s GHGE by 2050 and this involves switching from propellant to DPI inhalers which have a lower GWP (Figure 1). 6 , 14
Figure 1.
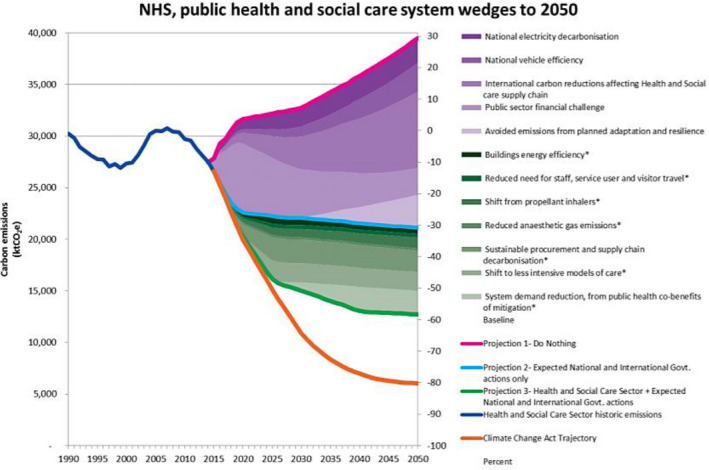
This graph shows the potential impact of a shift from propellant inhalers on carbon emissions in the context of other global, national and health sector actions 14
Climate change and its related health risks 15 is a driver for the reduction in the number of pMDIs prescribed in the UK. Here we review the evidence for the environmental impact of pMDIs, which is now well established. 6 , 16 , 17 , 18 We also consider the clinical and cost effectiveness and patient preference of DPI vs pMDI inhalers and propose that these factors are not necessarily barriers to switching to inhaler devices with lower GWP.
2. ENVIRONMENTAL IMPACT
pMDIs have a significantly higher GWP, due to their hydrofluoroalkane (HFA) propellants, which are quoted to be, gram for gram, up to 3800 times a more powerful greenhouse gas than carbon dioxide. 10 , 19 The DPI, which does not require a propellant, has a carbon footprint 18 times lower than MDIs. 18 , 19 , 20 Wilkinson et al 17 calculated that if 10% of UK pMDI inhalers were replaced with their corresponding DPI devices, more than 68.6 kilo tonnes of CO2 equivalent could be saved each year. This is equivalent to the mass of CO2 produced from 43 thousand roundtrip transatlantic flights (return economy flights from London to New York). 21
A study comparing carbon footprints of the entire life‐cycle of various inhalers including their productive and distribution found that MDI devices had up to 30 times larger carbon footprints than DPI equivalents and that these differences were mainly related to the use phase and end‐of‐life (disposal) phase. 22 It was calculated that if England applied the Swedish distribution of pMDIs and DPIs, 550 kt of CO2 would be saved annually—which corresponds to approximately 2.6% of NHS England’s total carbon footprint. 22
Furthermore, the inappropriate disposal of pMDIs contributes further to their environmental impact. 23 Although some pMDIs do have dose counter mechanisms, this is not universal (in contrast to DPIs) and means that patients may not know how many doses are left in their inhalers. This creates two problems: firstly, patients can unknowingly run out of doses which is potentially catastrophic during an acute exacerbation of asthma or COPD; and secondly, it leads to patients being more likely to request repeat prescriptions earlier than necessary. 24 The inappropriate disposal of pMDI devices with unused doses is especially concerning as not only does it increase the prescribing burden but devices no longer in use continue to release greenhouse gases into the atmosphere. 23 In a UK study, inhalers that had been disposed of incorrectly were collected over 90 days from one local district hospital and this resulted in enough pMDIs to produce an equivalent of 2.63 tonnes of CO2 emissions which would otherwise have been released into the atmosphere. 23 The recent British Thoracic society position statement on “The Environment and Lung Health” 25 highlights the importance of advising patients on avoiding disposal of inhalers in landfill sites and of supporting recycling schemes through pharmacies.
It should be noted that DPIs have limited benefit in some environmental domains not related to climate change. This is seen in Jeswani et al’s study 26 which found that although DPIs can reduce the climate change impact of inhalers by 96% if they replace pMDIs, this comes at a cost in domains such as marine eutrophication and fossil depletion, which should be acknowledged.
In view of the legal obligations to reduce GHG emissions together with the health benefits of climate change mitigation, a move away from pMDIs to DPIs seems increasingly important.
3. CLINICAL EFFECTIVENESS
Concerns about the effectiveness of each inhaler needs to be addressed. In 2005, Dolovich et al’s 20 systematic review found no significant differences in the efficacy of different inhaler types, including pMDIs and DPIs in both asthma and COPD patients in all clinical situations examined. However, the reviewed RCTs only included patients with a perfect inhaler technique. This is important, as the conclusion may not represent the “real world efficacy”, in which patients do not always use their inhalers correctly.
pMDIs deliver the drugs into the airways through a propellant mechanism. Failure in coordinating actuation of the inhaler with a long slow inspiration by the patient is the most significant problem for patients using pMDIs. 27 When using DPIs, the drug is pulled into the lungs as a result of the patients’ own inspiratory effort and therefore, when using a DPI, poor coordination becomes less of a barrier to effective therapy. 28 In fact, it has been widely reported that the proportion of patients using the correct technique with pMDIs without a spacer is low. Two separate studies reported correct technique using a pMDI as compared with DPIs to be 23%‐43% and 53%‐59% respectively. 18 , 22 Effective use of a DPI requires the patient to generate a peak inspiratory flow (PIF) that overcomes the internal resistance of the inhaler. Using a Turbohaler©, PIFs >30 L/min have been shown to be sufficient for effective administration in both adult and children populations. 29 , 30 As disorders primarily affecting expiration, both COPD and asthma do not significantly limit individual PIF rates. However, clinicians should be aware that, DPIs are not the appropriate choice of inhaler for patients who are not able to generate sufficient inspiratory flow. For example, frail, elderly patients, selected patients with COPD, very young patients or those with muscle weakness. Pederson et al 29 showed that 25% of children 3‐5 years of age were not able to, and Janssens et al 31 showed that up to 30% of elderly COPD patients were not able to achieve rates of 45 L/min via various DPI devices.
Nonetheless, when considering effectiveness of drug delivery, DPIs should be considered in clinical scenarios where both inhaler types are appropriate while recognizing that some patients will need to be provided with a pMDI in a rescue pack for use in the case of an acute exacerbation. The UK National Institute for Health and Care Excellence (NICE) has produced a patient decision aid for patients with asthma that suggests a DPI device is suitable and should be considered for asthma patients who can breathe in deeply for 2‐3 seconds independent of their coordination or ability to take a longer 4‐5 second breath. 32
4. COST EFFECTIVENESS
The apparent higher financial cost associated with DPIs compared to pMDIs has long been a barrier to their widespread use in the NHS. 17 , 27 This is because the pMDI version of the frequently prescribed short‐acting bronchodilators for asthma and COPD are less expensive than their DPI counterparts. 17 , 33 However, other medications, especially combination inhalers of Long‐Acting‐Beta‐Agonists and Inhaled Corticosteroids are cheaper in DPI formulations compared to pMDIs. 17 Interestingly, a cost analysis of community inhaler prescriptions concluded that although a widespread switch from pMDI to DPIs would result in an increase in short‐acting bronchodilator associated costs, this would be offset by the savings made with other inhaled medications. Overall, it was modeled that for every 10% of pMDIs that are replaced by cheapest DPI alternatives, more than £8.24 million could be saved annually. 17 Similarly, Korean and South Indian studies have failed to show a significant difference in overall costs between DPI and pMDI. 34 , 35 , 36 This renders the historical assumption of DPIs being more expensive than pMDIs as questionable and hence should not be seen as a barrier to DPI prescriptions. In fact, the modeled economic benefits of switching to DPIs provides a further driver to change inhaler devices prescribing practice.
5. PATIENT PREFERENCE
Unsurprisingly, ease of use has been identified as one of the most important considerations for patients and healthcare professionals in the choice of inhalers. 37 The 2017 study by Ramadan et al 38 explored the satisfaction of 246 asthma and COPD patients treated with either DPI and/or pMDI and discovered that a significantly greater percentage (73% vs 46%) of DPI users found their inhaler easy to use and were more satisfied with their care compared to pMDI users. Furthermore, a 2011 study 39 investigated the response when COPD patients previously treated with pMDI were switched to a DPI and given inhaler training during a hospital visit for an acute exacerbation of their condition. Findings indicate that 3 months after the switching intervention, the majority of switched patients remained on the DPI. This not only illustrated that some patients may have preferred using a DPI but also that it is feasible to make simple interventions to switch patients currently treated with a pMDI to a DPI successfully. It is important to note that nonconsensual switching of inhalers, without appropriate instruction regarding inhaler techniques can lead to worse clinical outcomes for COPD and asthma patients. 40 However, Price et al 41 have shown that outcomes after consensual switching of inhalers with face‐to‐face online consultations did not lead to any reduction in clinical effectiveness. In addition, a more recent study 42 attempted to address the paucity of information about patients and physician attitudes to the choice of inhalers and surveyed 50 NHS patients who were already using their inhalers. This found that 44% of those patients expressed that the carbon footprint of their inhaler is “important” or “very important” to them. We concede that this is a small sample size and that more research into this area is required. Importantly, in line with other research, it also found that 80% of those surveyed rated ease of use of inhalers as “important” or “very important”. Overall, using a patient‐centered approach to inhaler prescribing that takes into account patients’ preferences is important. Some patients will choose to use or remain on a pMDI but there is evidence that for some patients a DPI will be preferable. Device options should be discussed with patients and clinicians should feel confident to start a DPI or switch a pMDI inhaler to a DPI when clinically appropriate if patients are in agreement. Appropriate advice as well as regular technique reviews should also be offered.
6. CURRENT GUIDELINES
Currently, guidelines in the UK regarding the choice of inhalers do not make an appropriate emphasis on the potential carbon savings that could be achieved when selecting DPIs over pMDIs. In fact, the July 2019 NICE guidance for COPD diagnosis 43 and management does not offer any advice regarding deciding between pMDIs and DPIs and contains no information on the environmental impact of each device. However, in asthma management, the recent British Thoracic Society (BTS) guidance does now advise that “Prescribers, pharmacists and patients should be aware that there are significant differences in the global‐warming potential of different MDIs and that inhalers with low global‐warming potential should be used when they are likely to be equally effective”. 34 This is an encouraging development but is short of explicitly recommending the DPIs (which have a ‘lower global‐warming potential’) as the preferred choice based on similar efficacy, higher patient preference and lower climate impact. The patient decision aid on inhaler devices for asthma published by NICE also includes a discussion of the environmental impact of different inhalers. 32
Although there is a lack of research into clinician awareness of the carbon footprint of different inhaler types, there is certainly scope to increase this awareness and potentially alter prescribing decisions through a greater emphasis in clinical guidelines. For the busy clinician, guidelines should highlight boldly that DPIs are the preferred inhaler type under circumstances when both pMDIs and DPIs are appropriate for the patient.
7. CONCLUSIONS AND RECOMMENDATIONS
Climate change is an existential threat to the entire population of this planet and because of this, all societal sectors must adopt changes to reduce GHG emissions. A shift in inhaler devices prescribing practices in favor of DPIs and away from pMDIs, where clinically appropriate, has the potential to significantly reduce healthcare associated GHGEs. 6 Moreover, as well as the well‐documented environmental benefits, a switch towards DPI devices should be supported as DPIs are at least as effective, potentially cheaper and are often are preferred by patients.
In accordance with the NHS Long Term Plan to “shift to lower carbon inhalers” 44 our recommendations are that national and local guidelines are updated; guidance should consider the potential benefits of advising DPIs as the device of choice in new diagnoses of asthma and COPD as well as the benefits of switching patients currently using pMDIs to DPIs where clinically appropriate. We recognize the short‐term financial impact on the local health economy but also highlight potential long‐term cost savings.
Some concerns have been expressed in response to the proposals to reduce pMDI prescribing in the UK. 45 In line with others, 8 we are not advocating for a total switch from pMDIs to DPIs and recognize that some patients will have valid reasons to continue to use a pMDI but instead aim to explore the relative advantages and disadvantages of changing prescribing practice. It is the role of the healthcare professional to ensure that their patient’s condition is managed optimally with appropriate attention paid to their preferences and that patients are able to manage their symptoms effectively in partnership with their clinical team.
We recognize that HFCs are widely used globally across many different sectors such as air conditioning and refrigeration and their use in inhalers represents only a small proportion of this volume; the counter‐argument to this is that action is being taken to reduce this across these sectors 46 and healthcare should not be exempt from being required to take action. Equally, while pMDIs contribute only a small proportion of the carbon footprint of the NHS, if this can be reduced with no negative impacts on patients then we would argue that this should be prioritized along with other measures taken to make healthcare more sustainable. It is therefore appropriate that this is also addressed within the healthcare sector and that healthcare workers, as professionals advocating for the health of the public that they serve, would want to ensure that the contribution of healthcare to climate change is minimized as far as possible.
Future research should focus on evaluating clinician awareness of the environmental benefits of DPI inhalers and evaluating the impact of a change in guidelines on the prescribing of inhalers. Finally, timely implementation of a large number of environmental measures is essential to reverse the environmental catastrophe that is currently unfolding.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICAL STATEMENT
Ethical and legal approval was not required for this paper.
Starup‐Hansen J, Dunne H, Sadler J, Jones A, Okorie M. Climate change in healthcare: Exploring the potential role of inhaler prescribing. Pharmacol Res Perspect. 2020;8:e00675 10.1002/prp2.675
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change. Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693‐1733. 10.1016/S0140-6736(09)60935-1 [DOI] [PubMed] [Google Scholar]
- 2. WHO . WHO calls for urgent action to protect health from climate change – Sign the call. WHO. 2016. https://www.who.int/globalchange/global‐campaign/cop21/en/. Accessed September 4, 2019.
- 3. Climate change|Local Government Association . https://www.local.gov.uk/topics/environment‐and‐waste/climate‐change. Accessed February 18, 2020.
- 4.Removing F‐gases could slow global warming by 0.5 degrees ‐ News from Parliament ‐ UK Parliament. https://www.parliament.uk/business/committees/committees‐a‐z/commons‐select/environmental‐audit‐committee/news‐parliament‐2017/f‐gases‐report‐published‐17‐19/. Accessed November 16, 2019.
- 5. BEIS . UK becomes first major economy to pass net zero emissions law. Department for Business Energy & Industrial Strategy. https://www.gov.uk/government/news/uk‐becomes‐first‐major‐economy‐to‐pass‐net‐zero‐emissions‐law. Published 2019. Accessed March 2, 2020.
- 6. NHS Sustainable Development Unit . Reducing the use of natural resources in health and social care, 2018 Report. 2018;(x):1‐31.
- 7. National Health Service . Greener NHS campaign to tackle climate ‘health emergency’. National Health Service. https://www.england.nhs.uk/2020/01/greener‐nhs‐campaign‐to‐tackle‐climate‐health‐emergency/. Published 2020. Accessed March 22, 2020.
- 8. Hillman T, Mortimer F, Hopkinson NS. Inhaled drugs and global warming: time to shift to dry powder inhalers. BMJ. 2013;346:f3359 10.1136/bmj.f3359 [DOI] [PubMed] [Google Scholar]
- 9. Environmental Audit Committee . UK Progress on Reducing Nitrate Pollution Eleventh Report of Session 2017‐19 Report, Together with Formal Minutes Relating to the Report Environmental Audit Committee.; 2018. www.parliament.uk. Accessed March 2, 2020.
- 10. Naylor C, Appleby J. Sustainable health and social care Connecting environmental and financial performance. The King’s Fund. https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/sustainable‐health‐social‐care‐appleby‐naylor‐mar2012.pdf. Published 2012. Accessed September 5, 2019.
- 11. Audit Committee E . UK Progress on Reducing F‐Gas Emissions Fifth Report of Session 2017‐19 Report, Together with Formal Minutes Relating to the Report.; 2018. www.parliament.uk/. Accessed December 3, 2019.
- 12. Goulet B, Olson L, Mayer BK. A comparative life cycle assessment between a metered dose inhaler and electric nebulizer. Sustain. 2017;9:1725 10.3390/su9101725 [DOI] [Google Scholar]
- 13. Lavorini F, Corrigan CJ, Barnes PJ, et al. Retail sales of inhalation devices in European countries: so much for a global policy. Respir Med. 2011;105:1099‐1103. 10.1016/j.rmed.2011.03.012 [DOI] [PubMed] [Google Scholar]
- 14. Sustainable Development Unit . Carbon Update for the Health and Care Sector in England 2015; 2016. https://www.sduhealth.org.uk/resources/default.aspx?cat=Carbon+Footprint. Accessed March 24, 2020.
- 15. Masson‐Delmotte V, Zhai P, Pörtner HO, et al. Summary for Policymakers. In: Global Warming of 1.5°C. An IPCC Special Report on the Impacts of Global Warming of 1.5°C above Pre‐Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response To.; 2018. https://report.ipcc.ch/sr15/pdf/sr15_spm_final.pdf%0Ahttp://www.ipcc.ch/report/sr15/. Accessed December 19, 2019.
- 16. Wilkinson A, Hillman T, Hopkinson NS, Janson C, Smith J, Woodcock AA. Our patients and our planet—holistic considerations for inhaler choice. Lancet Respir Med. 2019;7:e11. http://www.ncbi.nlm.nih.gov/pubmed/30823976. Accessed September 4, 2019. [DOI] [PubMed] [Google Scholar]
- 17. Wilkinson AJK, Braggins R, Steinbach I, Smith J. Costs of switching to low global warming potential inhalers. An economic and carbon footprint analysis of NHS prescription data in England. BMJ Open. 2019;9:e028763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carbon Hotspots Update for the Health and Care Sector in England 2015; 2016. https://www.sduhealth.org.uk/documents/publications/2016/Carbon_Footprint_summary_HCS_hotspots_2015_final.pdf. Accessed February 21, 2020.
- 19. British Thoracic Society . Position statement environment and lung health 2019. 2019. https://www.brit‐thoracic.org.uk/document‐library/governance‐and‐policy‐documents/position‐statements/environment‐and‐lung‐health‐position‐statement‐2019/. Accessed January 21, 2020.
- 20. Dolovich MB, Ahrens RC, Hess DR, et al. Device selection and outcomes of aerosol therapy: evidence‐based guidelines: American College of Chest Physicians/American College of Asthma, Allergy, and Immunology. Chest. 2005;127:335‐371. 10.1378/chest.127.1.335 [DOI] [PubMed] [Google Scholar]
- 21. Wynes S, Nicholas KA. The climate mitigation gap: education and government recommendations miss the most effective individual actions. Environ Res Lett. 2017;12(7):074024. 10.1088/1748-9326/aa7541 [DOI] [Google Scholar]
- 22. Janson C, Henderson R, Löfdahl M, Hedberg M, Sharma R, Wilkinson AJK. Carbon footprint impact of the choice of inhalers for asthma and COPD. Thorax. 2020;75:82‐84. 10.1136/thoraxjnl-2019-213744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dipper A, Anning L, Zorzi A, et al. Reducing plastic waste, carbon footprint and cost: inhaler recycling at Musgrove Park Hospital. European Respiratory Society (ERS). 2018;52:PA3158 10.1183/13993003.congress-2018.pa3158 [DOI] [Google Scholar]
- 24. Sander N, Fusco‐Walker SJ, Harder JM, Chipps BE. Dose counting and the use of pressurized metered‐dose inhalers: running on empty. Ann Allergy Asthma Immunol. 10.1016/S1081-1206(10)61366-X [DOI] [PubMed] [Google Scholar]
- 25. Statement P, Environment THE . THE ENVIRONMENT AND LUNG HEALTH 2020 2. Advocacy : the lung health perspective THE ENVIRONMENT AND LUNG HEALTH 2020. 2020;(March):1‐5.
- 26. Jeswani HK, Azapagic A. Life cycle environmental impacts of inhalers. J Clean Prod. 2019;237:117733 10.1016/j.jclepro.2019.117733 [DOI] [Google Scholar]
- 27. Newman SP. Principles of metered‐dose inhaler design. Respir Care. 2005;50:1177‐1188. https://pubmed.ncbi.nlm.nih.gov/16122401/. Accessed July 16, 2020. [PubMed] [Google Scholar]
- 28. Sharma G, Mahler DA, Mayorga VM, Deering KL, Harshaw Q, Ganapathy V. Prevalence of low peak inspiratory flow rate at discharge in patients hospitalized for COPD exacerbation. Chronic Obstr Pulm Dis J COPD Found. 2017;4:217‐224. 10.15326/jcopdf.4.3.2017.0183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pedersen S, Hansen OR, Fuglsang G. Influence of inspiratory flow rate upon the effect of a Turbuhaler. Arch Dis Child. 1990;65:308‐310. 10.1136/adc.65.3.308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Engel T, Heinig J, Madsen F, Nikander K. Peak inspiratory flow and inspiratory vital capacity of patients with asthma measured with and without a new dry‐powder inhaler device (Turbuhaler). Eur Respir J. 1990;3:1037‐1041. [PubMed] [Google Scholar]
- 31. Janssens W, VandenBrande P, Hardeman E, et al. Inspiratory flow rates at different levels of resistance in elderly COPD patients. Eur Respir J. 2008;31:78‐83. 10.1183/09031936.00024807 [DOI] [PubMed] [Google Scholar]
- 32. NICE . Patient decision aid Inhalers for asthma. 2019:1‐14. https://bit.ly/inhalervids%0Ahttps://www.nice.org.uk/guidance/ng80/resources/inhalers‐for‐asthma‐patient‐decision‐aid‐pdf‐6727144573. Accessed September 4, 2019.
- 33. Shepherd J, Rogers G, Anderson R, et al. Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long‐acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over. Health Technol Assess. 2008;12:iii‐iv, 1‐360. http://www.ncbi.nlm.nih.gov/pubmed/18485271. Accessed September 4, 2019. [DOI] [PubMed] [Google Scholar]
- 34. British Thoracic Society . British Guideline on the Management of Asthma; 2019. https://www.sign.ac.uk/assets/sign158.pdf. Accessed January 25, 2020.
- 35. Rhee CK, van Boven JFM, Yau Ming SW, et al. Does changing inhaler device impact real‐life asthma outcomes? Clinical and economic evaluation. J Allergy Clin Immunol. 2019;7:934‐942. 10.1016/j.jaip.2018.09.027 [DOI] [PubMed] [Google Scholar]
- 36. Vigneshwaran E, Maddirevula MR, Dharmareddy L, et al. Cost effective analysis of dry powdered inhalers versus metered dose inhalers of salbutamol for asthma in rural secondary care hospital of South India. Value Health. 2014;17:A595‐A596. 10.1016/j.jval.2014.08.2054 [DOI] [PubMed] [Google Scholar]
- 37. Molimard M, Colthorpe P. Inhaler devices for chronic obstructive pulmonary disease: insights from patients and healthcare practitioners. J Aerosol Med Pulm Drug Deliv. 2015;28:219‐228. 10.1089/jamp.2014.1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ramadan WH, Sarkis AT. Patterns of use of dry powder inhalers versus pressurized metered‐dose inhalers devices in adult patients with chronic obstructive pulmonary disease or asthma: an observational comparative study. Chron Respir Dis. 2017;14:309‐320. 10.1177/1479972316687209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shakespeare J, Storey K, Parr D. P228 An audit of the effectiveness of competency based spirometry training. Thorax. 2011;66(Suppl 4):A161 10.1136/thoraxjnl-2011-201054c.228 [DOI] [Google Scholar]
- 40. Bjermer L. The importance of continuity in inhaler device choice for asthma and chronic obstructive pulmonary disease. Respiration. 2014;88:346‐352. 10.1159/000363771 [DOI] [PubMed] [Google Scholar]
- 41. Price D, Small I, Haughney J, et al. Clinical and cost effectiveness of switching asthma patients from fluticasone‐salmeterol to extra‐fine particle beclometasone‐formoterol: a retrospective matched observational study of real‐world patients. Prim Care Respir J. 2013;22:439‐448. 10.4104/pcrj.2013.00088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Liew K, Wilkinson A. P280 How do we choose inhalers? patient and physician perspectives on environmental, financial and ease‐of‐use factors. Thorax. 2017;72:A235‐A237. 10.1136/thoraxjnl-2017-210983.422 [DOI] [Google Scholar]
- 43. NICE . Overview|Chronic obstructive pulmonary disease in over 16s: diagnosis and management|Guidance|NICE. https://www.nice.org.uk/guidance/NG115. Published 2010. Accessed March 2, 2020.
- 44. Chapman R, Middleton J. The NHS long term plan and public health. BMJ. 2019;364:l218 10.1136/bmj.l218 [DOI] [PubMed] [Google Scholar]
- 45. Partridge MR. Green respiratory healthcare: need for proportionality. Thorax. 2020;75:369 10.1136/thoraxjnl-2019-214315 [DOI] [PubMed] [Google Scholar]
- 46. United Nations Environment Programme . The Kigali Amendment to the Montreal protocol: another global commitment to stop climate change. UN Environment. https://www.unenvironment.org/es/node/20806%0Ahttps://www.unenvironment.org/news‐and‐stories/news/kigali‐amendment‐montreal‐protocol‐another‐global‐commitment‐stop‐climate. Published 2016. Accessed August 27, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


