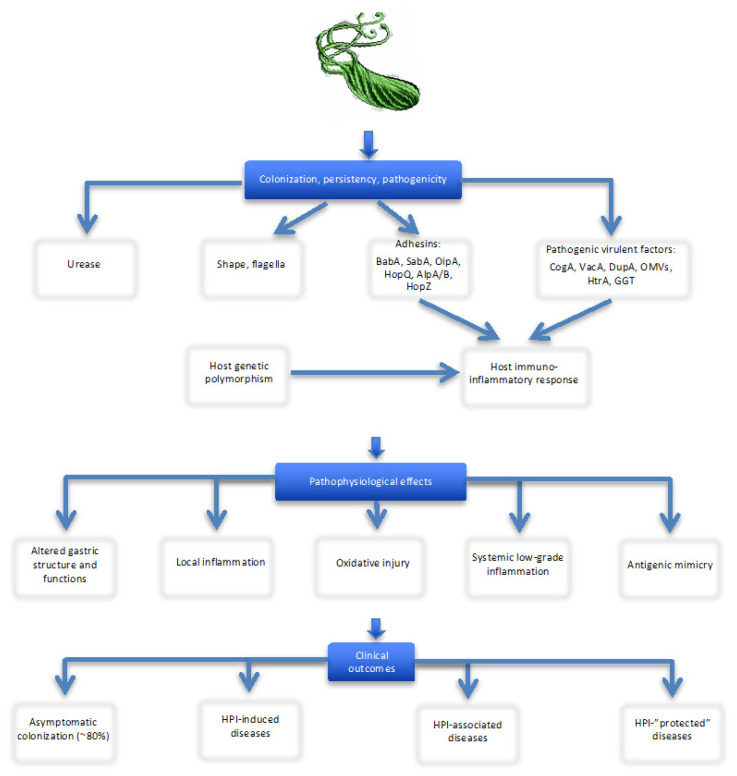
Figure 1.
Overview of Helicobacter pylori (H.p.) characteristics contributing to gastric colonization, persistence, pathogenicity and clinical outcomes. Abbreviations: AlpA/B, adherence-associated lipoprotein A and B; BabA, blood group antigen-binding adhesin; CagA, cytotoxin associated antigen A; DupA, duodenal ulcer (DU) promoting antigen; GGT, gamma-glutamyl transpeptidase; HopQ, HopZ, H. pylori outer membrane proteins; HtrA, high-temperature requiring protein; OipA, outer inflammatory protein; OMVs, outer membrane vesicles; SabA, sialic acid-binding adhesin; VacA, vacuolating cytotoxin. Notes: The outcome of H.p. is multifactorial and depends on interaction between multiple heterogenic bacterial virulence factors, host genetics, lifestyle and environmental influences. H.p. utilizes a variety of mechanisms which allow: (1) escaping high acid environment (urease, bacterial shape and flagella); (2) attaching to the gastric epithelial layer (adhesin proteins); (3) exerting epithelial cell pathogenicity and (4) affecting the host innate and adaptive immune responses. The expression of virulence factors and host’s immunologic responses (dependent of genetic predisposition/resistance, e.g., proinflammatory cytokine gene polymorphisms) are critical to host colonization, infection persistence and pathogenesis of local (gastroduodenal) and systemic (extra-digestive) diseases. The cascade of pathophysiologic events in the stomach includes acid neutralization, mucus layer destruction, immune cell activation (lymphocytes, macrophages, dendritic cells, natural killer and mast cells), upregulation of pro-inflammatory (IL-1β, IL-6, IL-8, IL-17,TNF-α, IFN-γ and CRP) and anti-inflammatory (IL-4 and IL-10) cytokines (immune-inflammatory axes) and increased production of reactive oxygen species (oxidative stress) causing cell damage, alterations of gastric structure and functions (including changes in gastric acid and pepsin secretion, hormone production) as well as numerous effects on the gut (motility and microbiota) and extra-digestive organs; these may result in gastroduodenal erosion, peptic ulcer, carcinogenesis or lymphoma formation, as well as contribute to development and progression of numerous chronic diseases outside the stomach (CVDs, neurodegenerative, hematologic, metabolic, CKDs, CLDs, etc.); however, the role of HPI is not necessarily detrimental, it may even be “protective” (asthma in children; allergy; IBD, especially Crohn’s disease; and autoimmune disorders). Infection with virulent strains (in particular, cagA+ and vacA+) is associated with higher inflammatory response, oxidative injury and elevated risk of gastroduodenal and most extra-digestive diseases.