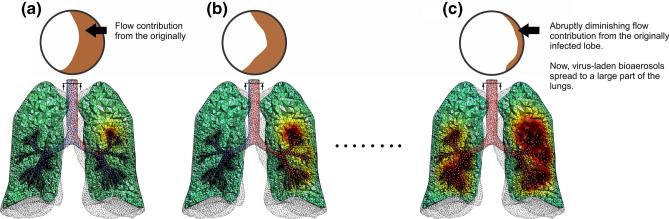
Figure 1.
SARS COV-2 virus spreading in the lungs (see also a video animation in supplementary material). Flow distribution in the lungs is mapped on the cross-section of the trachea shown at the top of each figure. (a) Suppose some part of the lung is initially infected by inhaled SARS COV-2 virus (in this example, we assume that the left upper lobe is initially infected). As a result, near the lesion, virus-laden meniscus may be formed and a rupture of those menisci may form a number of virus-laden small bioaerosols (shown as red dots). (b) Those bioaerosols move toward the airway opening with the expired air. While most of them exit from the body, some of them may remain suspended in the airways. Some of particles, which exit the body, may reenter the lungs in the next inhalation and move around the lungs, but deposition of those reentered particles may be minuscule due to their low diffusivity. Some of the particles, which remain suspended in the airways retrace back to their original position due to the negligible (but no zero) diffusivity. (c) However, as the disease progresses, the production of virus-laden bioaerosols increases, the tissues available for gas exchange become smaller and smaller as the infected lesion becomes larger and larger. This may dramatically alter the distribution of airflow in the lungs, resulting in a substantial spread the infection to other parts of the lungs. This may cause cytokine storm. A dramatic change of flow distribution in the lungs can be seen as a significant alteration cross sectional map pattern from Figs. 1a, to 1c.