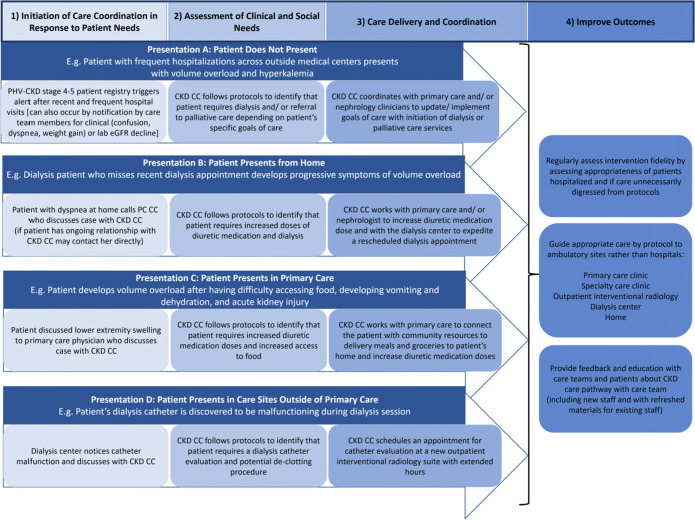
Figure 3.
Examples of the application of the PHV-CKD care coordination pathway to four prevalent scenarios (A–D) describing clinical decline or need for chronic kidney disease patients. Legend: Baseline structural problems prior to pathway implementation: Presentation A describes patients without a regular pattern of care monitoring or consistent care clinician, but with frequent episodes of clinical decline or need prompting recurrent ED and hospital stays across external care settings. The system lacked a patient registry for CKD patients to monitor patients outside of in-person clinic visits, data systems to integrate plans data useful in monitoring patients outside of the local hospital and ED, and staff to proactively monitor stage 4–5 CKD patients. Presentation B describes patients with a regular clinician but inconsistent follow-through with visits. From this group, analytics documented the frequent incidence of dialysis patients presenting with shortness of breath after missing a dialysis appointment. Primary care team including primary care coordinators were spread thin and did not have dedicated time to expeditiously care for these patients who require significant coordination outside of in-person visits. Presentation C focuses on patients with a recent primary care evaluation showing acute on chronic kidney injury. Primary care clinics were not linked to the operations of specialty services required to expeditiously care for patients. Presentation D describes patients who present with urgent or emergent needs from a variety of other care settings with malfunctioning dialysis catheters. The health system lacked staff to coordinate specialty care and care sites to evaluate and treat catheters in the ambulatory setting, and primary and multispecialty care team members would often send patients to the ED for evaluation. The system-wide CKD care team both includes primary care members consisting of primary care coordinators, primary care clinicians, social workers, and others and includes multispecialty care members consisting of specialists (e.g., nephrologists), emergency department, urgent care, dialysis centers, and others. CKD-CC, chronic kidney disease care coordinator; PC-CC, primary care coordinator.