Abstract
As a result of the coronavirus disease 2019 (COVID-19) global pandemic, medical trainees have faced unique challenges and uncertainties. To capture the experiences of allergy and immunology fellows throughout the United States and Canada during this time, a 17-item electronic questionnaire was distributed to 380 fellow-in-training (FIT) members of the American Academy of Allergy, Asthma, and Immunology enrolled in US and Canadian allergy/immunology fellowship programs. Voluntary and anonymous responses were collected from April 15 to May 15, 2020. In addition to summary statistics, categorical data were compared using χ2 tests (Fisher's exact). Responses were obtained from FITs across all years of training and primary specialties (Internal Medicine, Pediatrics, and Medicine-Pediatrics) with a response rate of 32.6% (124 of 380). Reassignment to COVID-19 clinical responsibilities was reported by 12% (15 of 124) of FITs, with the largest proportion in the US northeast region. A majority of FITs used telehealth (95%) and virtual learning (82%) during the pandemic. Overall, 21% (25 of 120) of FITs expressed concern about potentially lacking clinical experience for independently practicing allergy and immunology. However, FITs using telehealth reported lower concern compared with those who did not (18.4% [21 of 114] vs 66.7% [4 of 6]; P = .01). The survey shows that allergy and immunology trainee experiences have varied considerably since the COVID-19 outbreak. Notably, the adoption of telehealth and virtual learning was commonly reported, and optimization of these virtual experiences will be helpful. Even outside of pandemics, training on the use of telemedicine may be a sound strategy in preparation for future health care delivery and unexpected events.
Key words: COVID-19, Fellows-in-training, Trainee, Education, Survey, Telemedicine, Telehealth, Virtual learning, Allergy and immunology
Abbreviations used: AAAAI, American Academy of Allergy, Asthma, and Immunology; COVID-19, Coronavirus disease 2019; FIT, Fellow-in-training; PPE, Personal protective equipment
AAAAI Position Statements, Work Group Reports, and Systematic Reviews are not to be considered to reflect current AAAAI standards or policy after five years from the date of publication. The statement below is not to be construed as dictating an exclusive course of action nor is it intended to replace the medical judgment of healthcare professionals. The unique circumstances of individual patients and environments are to be taken into account in any diagnosis and treatment plan. The statement reflects clinical and scientific advances as of the date of publication and is subject to change.
For reference only.
The emergence and rapid global spread of the coronavirus disease 2019 (COVID-19) due to the novel severe acute respiratory syndrome coronavirus 2 has resulted in substantial mortality and morbidity, along with interruptions of normal health care delivery. COVID-19 disease was declared a global pandemic by the World Health Organization and deemed a national emergency by the United States in March 2020.1, 2, 3 In response to the widespread COVID-19 outbreak, the medical community quickly mobilized to protect patients, health care workers, and trainees. Changes that were implemented included converting outpatient clinic visits to telemedicine, halting elective procedures, redeploying health care professionals, and transitioning to virtual learning.4, 5, 6, 7, 8
Several studies have outlined how health care practices and various training programs adapted to the new realities.8, 9, 10, 11 Surveys regarding the impact of the pandemic on residency and fellowship training are available from only a select few procedural specialties and subspecialties. In a survey of urology program directors, 60% reported concern that their residents may not meet minimum training requirements.12 Similarly, 2 of 3 program directors in interventional cardiology reported in a recent survey that they are concerned that the pandemic may present a moderate-to-severe impediment to fellowship training.13 In another survey, more than 60% of plastic surgery residents stated that cutbacks to didactics and practical training would affect their training and professional experience significantly.14 Although some surveys demonstrate the resilience of program directors and trainees, others reflect the challenges perceived during this pandemic. For example, a survey of head and neck surgery program directors indicated that 86% felt that their fellows were ready to enter practice,15 whereas a survey of 81 head and neck surgery trainees reported that although most felt prepared to practice, only 57% had secured full-time positions and 10% had a pending position put on hold because of hiring freezes.15
Data regarding the impact of these disruptions on the trainee experience remain limited, and the final toll of these changes to clinical practice and education, as well as trainee well-being, remains unknown. Specifically, there are no surveys of fellows-in-training (FITs) in allergy and immunology that address the COVID-19 pandemic. Accordingly, we surveyed US and Canadian American Academy of Allergy, Asthma, and Immunology (AAAAI) FITs between April and May 2020 to assess their educational and clinical experiences.
Methods
Using a cross-sectional study design, voluntary and anonymous surveys were administered between April 15 and May 15, 2020, to study the impact of the COVID-19 pandemic on FITs. This survey and study met an institutional review board exception. A 17-item electronic questionnaire was distributed to 380 FIT members of the AAAAI enrolled in US and Canadian allergy and immunology fellowship training programs. The web-based survey was designed and implemented by the AAAAI FIT Committee, and responses were obtained from 124 FITs. Data were collected on demographics, reassignment to treat patients with COVID-19, transition to virtual training platforms, and the impact of the pandemic on fellowship training. General comments shared by FITs regarding the impact of COVID-19 are listed in Table E1 in this article's Online Repository at www.jaci-inpractice.org.
Geographic regions were categorized based on predefined AAAAI criteria for surveys: Northeast (includes states of CT, MA, ME, NH, NY, RI, and VT); Mid Atlantic (includes states of NJ, PA, DE, MD, VA, WV, OH, and Washington, DC); Southeast (includes states of AL, FL KY, GA, NC, TN, and SC); Midwest (includes states of IA, IN, IL, ND, NE, MI, MN, SD, and WI); Mid-South (includes states of AR, KS, LA, MO, MS, OK, and TX); Rocky Mountain (includes states of AK, AZ, CO, ID, MT, NM, NV, WY, and UT); Western (includes states of CA, OR, WA, and HI); and Canada. All 5-point Likert scale responses were dichotomized into agree (strongly agree/somewhat agree) and disagree (neutral/somewhat disagree/strongly disagree), determined a priori.
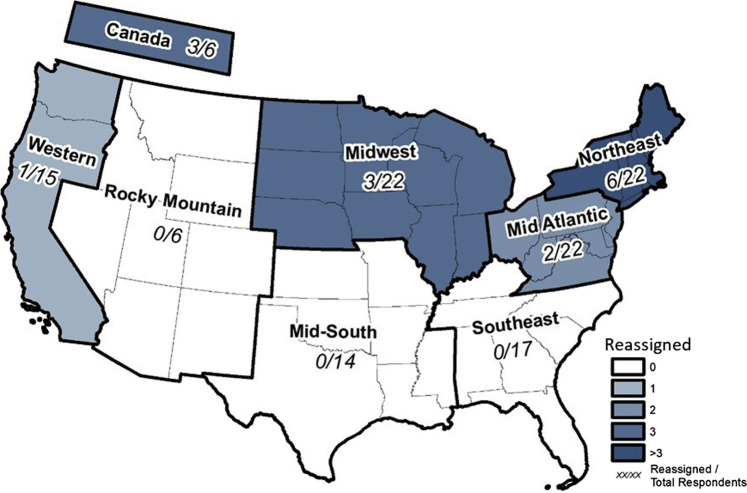
Summary statistics were reported including percentages for all categorical variables. Comparisons were done using χ2 tests with Fisher's exact for the categorical variables. Data were analyzed using STATA 16.1. Esri ArcGIS software (Redlands, NV) version 10.7 was used to generate the heat map (Figure 1 ).
Figure 1.
Regional distribution of fellows-in-training (FITs) reassigned to COVID-19 responsibilities. Responses are shown as the number of reassigned FITs and the number of respondents per region. Not depicted are the states of Alaska and Hawaii, which were included in the Rocky Mountain and Western regions, respectively. COVID-19, Coronavirus disease 2019.
Results
One hundred and twenty-four US and Canadian FITs responded to the survey between April and May 2020, for a response rate of 32% (124 of 380). Of those who responded, 49.2% expected to graduate in 2020; 42.7% in 2021; and 8.1% in 2022. FIT respondents were equally split between Internal Medicine and Pediatrics as their primary board certification. The majority (83.7%) held an unrestricted medical license to practice, and 31.7% had practiced at an attending level before their allergy and immunology fellowship (Table I ). The number of respondents from each geographic region is shown in Figure 1.
Table I.
Demographics of survey respondents
| Characteristic | All fellows-in-training (N = 124) |
|---|---|
| Anticipated year of graduation, n (%) | |
| 2020 | 61 (49.2) |
| 2021 | 53 (42.7) |
| 2022 | 10 (8.1) |
| Board certification, n (%) | |
| Internal Medicine | 55 (44.7) |
| Pediatrics | 56 (45.5) |
| Both Internal Medicine and Pediatrics | 6 (4.9) |
| Neither Internal Medicine nor Pediatrics | 6 (4.9) |
| Unrestricted full medical license, n (%) | 103 (83.7) |
| Prior attending level experience, n (%) | 39 (31.7) |
There were 12% (15 of 124) of FITs who reported being reassigned from their allergy and immunology fellowship duties to COVID-19-related clinical responsibilities that involved managing patients with COVID-19. Three of the 15 reassigned FITs volunteered for their new assignment. Reassignment response was missing in 1 individual and he or she was presumed to not have been reassigned. The Northeast region of the United States comprised the majority of reassigned FITs. Although FITs were reassigned from the Mid-Atlantic, Midwest, or Western regions as well as Canada, none were reassigned in the Mid-South or Rocky Mountain territories (Figure 1). The most common reassignment location was the adult inpatient floor (66.6% [10 of 15]), followed by the emergency department (20% [3 of 15]). All reassigned fellows managed patients with COVID-19 (93.3% [14 of 15]), except 1 FIT who was assigned to providing remote decision support for COVID-19 management.
Most (73.3% [11 of 15]) reassigned FITs were Internal Medicine trained, and 60% (9 of 15) responded that they had an unrestricted medical license to practice. Prior attending level experience was similar among those reassigned as compared with those not reassigned (33.3% [5 of 15] vs 31.5% [34 of 108]; P = 1.0) (Table II ). There were 23.3% (28 of 120) of FITs reporting an underlying condition that they felt may increase risk of severe COVID-19 illness. Fewer FITs with underlying medical conditions were reassigned relative to those with no underlying medical conditions (7.1% [2 of 28] vs 14.1% [13 of 92]; P = .5). Most (66.7% [10 of 15]) of those reassigned anticipated graduation in 2021 or later.
Table II.
Characterizing fellows in training who were reassigned to COVID-19 responsibilities and a comparison with those not reassigned
| Fellows-in-training reassigned (n = 15) | Fellows-in-training not reassigned (n = 109) | P value | |
|---|---|---|---|
| Reassignment setting∗, n (%) | |||
| Emergency medicine | 3 (20) | ||
| Adult inpatient medicine | 10 (66.7) | ||
| Other† | 3 (20) | ||
| Reassignment characteristics, n (%) | |||
| Voluntary reassignment | 3 (20.0) | ||
| Directly managed patients with COVID-19 during reassignment | 14 (93.3) | ||
| Board certification, n (%) | .09 | ||
| Internal Medicine | 11 (73.3) | 44 (40.7) | |
| Pediatrics | 3 (20.0) | 53 (49.1) | |
| Internal Medicine and Pediatrics | 0 | 6 (5.6) | |
| Neither Internal Medicine nor Pediatrics | 1 (6.7) | 5 (4.6) | |
| Anticipated graduation year, n (%) | |||
| Graduating in 2020 | 5 (33.3) | 56 (51.4) | |
| Graduating in 2021 or 2022 | 10 (66.7) | 53 (48.6) | |
| Unrestricted full medical license, n (%) | 9 (60.0) | 94 (87.0) | .01 |
| Prior attending level experience, n (%) | 5 (33.3) | 34 (31.5) | >.99 |
| Underlying medical conditions perceived as COVID-19 risk factors, n (%) | 2 (13.3) | 26 (24.8) | .51 |
| Concerned about lacking skills to practice Allergy Immunology independently after graduation, n (%) | 6 (40.0) | 19 (18.1) | .08 |
| Concerned about inability to complete research project before graduation, n (%) | 7 (46.7) | 39 (37.1) | .57 |
COVID-19, Coronavirus disease 2019; FIT, fellow-in-training.
One FIT was reassigned to more than 1 location.
Other locations included televisits, outpatient drive through testing, and a decision support unit for patients with COVID-19 illness.
Overall, 20.8% (25 of 120) expressed a concern over not having adequate clinical experience needed to practice independently, and 38% (46 of 120) of FITs expressed concern that they may not be able complete research projects before graduation. A trend was seen toward a higher portion of reassigned FITs expressing concern about graduating without the adequate clinical experience they needed to practice independently as compared with those who were not reassigned (40% [6 of 15] vs 18.1% [19 of 86]), although it was not statistically significant (P = .083). Trends remained similar when stratified by year of graduation (data not shown). Similarly, 46% (7 of 15) of reassigned FITs versus 37.1% (39 of 105) nonreassigned FITs expressed concern about not being able to complete research before graduation (P = .5).
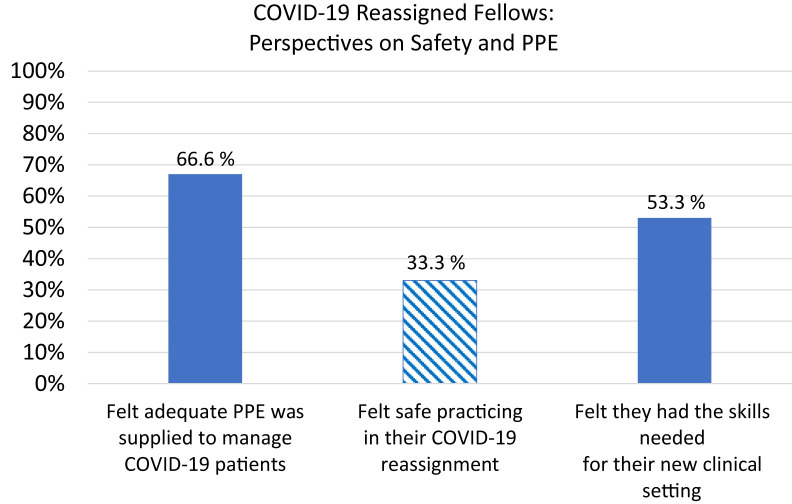
FITs reassigned to COVID-19 responsibilities were asked about their perceptions of safety, access to adequate personal protective equipment (PPE), and confidence managing patients with COVID-19. A majority (66.7% [10 of 15]) reported having adequate PPE; however, only 33.3% (5 of 15) FITs reported feeling safe practicing in their new setting (Figure 2). Although 3 FITs reported testing positive for COVID-19 or being presumed to have COVID-19 illness (an additional 4 individuals did not respond and they were presumed to have not developed COVID-19 illness), none of the reassigned FITs reported developing COVID-19 illness. Approximately half of the reassigned FITs (53.3% [8 of 15]) expressed confidence in possessing the needed skills to care for patients in the new COVID-19 setting, outside of their usual scope of allergy/immunology practice. No difference was noted by year of graduation or prior attending level experience (data not shown). Among the 8 FITs who felt confident managing patients with COVID-19, 62.5% (5 of 8) felt safe in their new practice setting. Conversely, none of the FITs who lacked confidence in their skills reported feeling safe (P = .02).
Figure 2.
Reported safety concerns among allergy and immunology fellows-in-training who were reassigned during the COVID-19 pandemic. COVID-19, Coronavirus disease 2019; PPE, personal protective equipment.
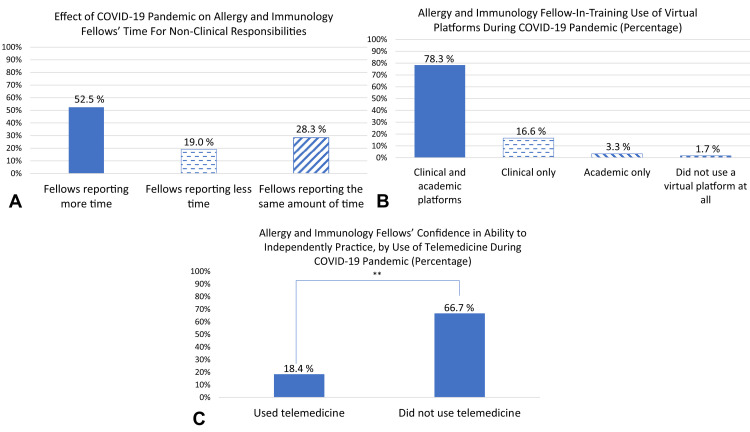
Most fellowship programs made a transition to telehealth and virtual learning during the COVID-19 pandemic; 78.3% (94 of 120) of FITs reported using both telehealth and virtual learning, whereas only 1.7% (2 of 120) reported using no virtual platforms (Figure 3 ). The changes in fellowship structure in response to COVID-19 allowed about half of the FITs more time (52.5% [63 of 120]) for nonclinical responsibilities, including research, whereas fewer FITs reported having less time (19% [23 of 120]) or no change in available time (28.3% [34 of 120]). Among those who expressed concerns about the lack of adequate clinical experience needed to practice independently, FITs using telehealth reported a lower concern about lack of adequate clinical experience as compared with those who did not transition to telehealth (18.4% [21 of 114] vs 66.7% [4 of 6]; P = .01).
Figure 3.
A, Most respondents noted an increase in time for nonclinical work during the COVID-19 pandemic. B, Percentages of US and Canadian allergy and immunology fellows using telemedicine and/or virtual learning during the COVID-19 pandemic. C, Fellows who did not use telemedicine during the COVID-19 pandemic were more than 3 times as likely to express concern about having insufficient clinical experience to practice independently (P = .017). COVID-19, Coronavirus disease 2019.
Discussion
The arrival and swift spread of COVID-19 in the United States and Canada has dramatically altered the medical landscape of these 2 countries and thereby given rise to unique challenges within our subspecialty. This Work Group Report summarizes and presents the data from the survey of FITs in allergy and immunology training programs in the United States and Canada to understand workflow and education changes, as well as concerns among fellows in response to change.
In our survey study, we found a wide range of experiences among allergy and immunology trainees during the COVID-19 pandemic. A small but significant number of fellows were reassigned to manage patients with COVID-19. Regional reassignment rates seemed to correlate with the geographic burden of COVID-19 on health care systems in Spring 2020, whereby the majority of reassigned FITs were in the Northeast region that contained the epicenter of the disease at that time.3 Most reassigned FITs were trained in Internal Medicine, likely a reflection of the burden of disease in the adult population, and all were reassigned to non–intensive care unit practice locations. A comparison of reassigned FITs versus those not reassigned showed similar characteristics, but there was a statistically nonsignificant trend toward more reassigned FITs feeling concerned about adequate clinical skills experience and inability to complete research on time.
Approximately 2 of 3 reassigned FITs reported having adequate PPE; however, only 1 in 3 reported feeling safe caring for patients with COVID-19. This is in concordance with a level of uncertainty and anxiety around the scarcity of PPE for health care workers with associated risks16 , 17 and changing recommendations for PPE use.18 A study of 91 residency Program Directors around New York City representing 24 specialties and more than 2300 residents showed that 43% of programs had at least 1 confirmed COVID-19-positive resident.17 They also showed that 11% (264 of 2306) of residents developed COVID-19, either confirmed or presumed illness. Although that study did not specifically address the proportions of hospital- versus community-acquired infections in these trainees, it brings up an important aspect of safety, specifically regarding the access and availability of adequate PPE. Similarly, we found that concerns about suboptimal PPE are common and pose an added level of anxiety. Importantly, in our study, none of the FITs who knowingly treated patients with COVID-19 had contracted the illness at the time of this survey. We do not have information on source of exposure for the 3 individuals in our survey who reported COVID-19 illness. The 23% overall rate of FITs who reported underlying medical conditions appears to be higher than would be expected in a trainee population; however, this survey reports individual perceptions early in the course of the US COVID-19 pandemic when knowledge about risk factors was still evolving. Although we may speculate whether more commonly encountered diagnoses, such as allergic rhinitis, asthma, and/or others, may have driven the higher than expected number, lack of knowledge about specific comorbidities in our survey remains a limitation.
An especially notable finding of our study was that confidence in the skills to manage patients with COVID-19 among reassigned FITs was associated with feeling safe in the new practice setting. This suggests that providing structured training and guidance in the care of patients with COVID-19 can be successful at alleviating stress and anxiety of preforming new unexpected tasks. It also adds to our understanding of the long-term dividends of strong specialty training, which may indicate an underappreciated way of enhancing provider confidence and well-being.
During the pandemic, FITs saw their daily routines dramatically altered, with the majority noting a shift to telehealth and/or virtual learning. In our study, when asked whether social distancing restrictions and virtual platforms implemented in response to the pandemic led to more or less time for nonclinical work, responses among fellows were mixed. The disagreement may be explained by differences in personal challenges outside fellowship (for instance, childcare issues for fellows with young children in the home may have seen their time diminished with increased parental commitments and stress). Reduced time for didactics and practical training is a concern as we move forward in the new phase after COVID-19. Importantly, in addressing this issue, our study found that the use of telehealth for clinical medicine was associated with lower anxiety about lacking adequate clinical skills to practice independently. It is important to optimize the telehealth and virtual learning experience while balancing the required in-person experience for FITs and maintaining open communication between FITs, program directors, and faculty. Facilitated communication is crucial to address any issues that may arise as new virtual curriculum strategies are explored. Looking ahead, telehealth visits and remote management will likely continue as we move into the next COVID phases. Our results reinforce that even as the pandemic resolves, training in virtual medicine should be used, not only to prepare for future large-scale events, but also to accommodate a probable transition of care toward a virtual format during “normal times.” It would be important to objectively evaluate the educational framework with various telemedicine practice models in conjunction with structured in-person care used by allergy and immunology trainees so as to optimize workflow and educational and patient care experiences.
The COVID-19 pandemic has required physicians to rapidly adapt to many changes within the traditional health care model. A survey of fellows in interventional cardiology expressed interest in potential fellowship extensions or a period of early career mentorship given the significant challenges.13 Creativity and resourcefulness are needed in fellowship programs along with buy-in from leadership to strengthen emphasis on career mentoring, networking, novel education formats, expectations, and research and safety projects. These may be aspects of training that will need to be addressed and adopted by the programs as we move forward with the next academic year, either during a COVID-safe recovery period or a continuing COVID pandemic. Such lessons may furthermore be applied to a future pandemic or other global challenge.
A voluntary response rate of 32.6% (124 of 380) from US/Canadian FIT members of the AAAAI provides a reasonably robust nationally representative sample of FITs in allergy and immunology. As with a voluntary survey, it is subject to selection bias and it is certainly possible that dissatisfied FITs or those with concerns may be more likely to complete surveys. In addition, the survey was completed in April/early May 2020 when the COVID-19 pandemic had not completely unfolded in several parts of the country and as such may be missing information on additional FIT experiences later in time. The inability to compare data from any of the FITs who did not respond to the survey remains a limitation in ascertaining the impact of survey sampling bias. Finally, although we believe that the allergy and immunology FIT community is diverse, it bears emphasis that the results of this survey pertain to a single subspecialty and may not be entirely generalizable to physician trainees in other fields of medicine.
In conclusion, we present here the results of the first nationally representative survey of allergy and immunology FITs regarding developments stemming from the COVID-19 pandemic. Allergy and immunology trainee experiences have varied widely, with several fellows reporting a pause in their training to allow reassignment to other services, a scenario that would have been almost unthinkable mere months ago. The vast majority of fellows described substantial changes in their day-to-day trainee lives. Although undoubtedly disruptive, the pandemic has generated opportunities to re-examine postgraduate medical education. For instance, the positive impact of telemedicine on trainee education and confidence in medical practice is a highlight of this study's results. This path would merit further development and continual assessment. As we pave the way forward with a phased reopening, we believe that these results may inform transformative innovation in the education of allergy and immunology FITs.
Acknowledgments
We would like to acknowledge Mariana Duran, Administrative Liaison to the FIT Committee, American Academy of Allergy, Asthma, and Immunology (AAAAI), for the effort to help with survey development, approvals, and implementation. We would also like to acknowledge Lauri Sweetman, Division of Practice and Policy, AAAAI; Renee Vandlik, Manager of Practice and Policy, AAAAI; and Sheila C. Heitzig, Director of Practice and Policy, AAAAI, for their effort in assistance with the AAAAI FIT survey approvals and implementation.
B. M. Kahwash contributed to study design and manuscript writing; and reviewed and approved the final manuscript. D. R. Deshpande contributed to study design, data analyses, and manuscript writing; and reviewed and approved the final manuscript. C. Guo contributed to manuscript writing and reviewed the manuscript. C. M. Panganiban contributed to manuscript writing, figures, and tables. H. Wangberg contributed to study design, figures, and abstract writing. T. J. Craig contributed to manuscript editing and review.
Footnotes
No funding was received for this work and authors were not compensated for their effort.
Conflicts of interest: D. R. Deshpande is the Chair of the American Academy of Allergy, Asthma, and Immunology (AAAAI) Fellows in Training Committee; and reports that she is employed by Regeneron Pharmaceuticals and her spouse is employed by Bristol Myers Squibb. C. Guo and C. M. Panganiban are the Past-Chair and Vice-Chair, respectively, of the AAAAI Fellows in Training Committee. T. J. Craig's only conflict in relation to these data and manuscript is being on the Board of the AAAAI. The rest of the authors declare that they have no relevant conflicts of interest.
Online Repository
Table E1.
Allergy and immunology FITs who responded to the survey were given an open text box to share their reactions to the changes brought by the COVID-19 pandemic
| Perceived concerns related to reassignment to COVID-19 duties | Reassignment of pediatrics trained FITs to adult COVID-19 units |
| Concerns that reassignments were perceived as nonvoluntary | |
| FITs being reassigned yet attendings not being reassigned | |
| Concern about being asked to practice as “attendings” in COVID-19 units | |
| Concern about compromised education in allergy and immunology due to reassignments | |
| Perceived clinical/research concerns | Requirement to be onsite despite virtual clinics |
| Concerns about perceived lack of support to find solutions to compensate for reduced clinical training and experience | |
| Concern about fewer patients and lack of physical examinations | |
| Concern about inability to complete research, especially bench research | |
| Lack of involvement of the Allergy Immunology service in COVID-19-related research | |
| Perceived educational/career concerns | Discontinued didactics and reliance solely on self-study |
| Cancelled electives resulting in compromised education | |
| Concerns related to missed networking and learning opportunities due to cancelled national conferences such as the AAAAI and CIS | |
| Concern related to uncertainty around the ABAI board examination and potential delays. Additional concerns regarding preparation for the ABAI board examination with a cancelled board review course | |
| Concerns about possible delays in graduation | |
| Job concerns including delays, hiring freezes, inability to find jobs, rescinded offers. Concern about viability of practices | |
| Perceived personal concerns | Added burden around family responsibilities. Concerns around childcare because schools and daycares are closed reducing time to study |
| Lack of personal time to study or get work done |
The table included responses summarized and grouped by areas of concerns.
AAAAI, American Academy of Allergy, Asthma, and Immunology; ABAI, American Board of Allergy and Immunology; CIS, Clinical Immunology Society; COVID-19, Coronavirus disease 2019; FIT, fellow-in-training.
References
- 1.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19): Cases, Data, and Surveillance. Center for Disease Control. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/index.html Available from:
- 4.Shaker M.S., Oppenheimer J., Grayson M., Stukus D., Hartog N., Hsieh E.W.Y. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract. 2020;8:1477–1488.e5. doi: 10.1016/j.jaip.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education . 2020. Three Stages of GME during the COVID-19 Pandemic.https://www.acgme.org/COVID-19/Three-Stages-of-GME-During-the-COVID-19-Pandemic/articleid/10127 Available from: [Google Scholar]
- 6.Chiel L., Winthrop Z., Winn A.S. The COVID-19 pandemic and pediatric graduate medical education. Pediatrics. 2020;146:e20201057. doi: 10.1542/peds.2020-1057. [DOI] [PubMed] [Google Scholar]
- 7.Keswani R.N., Sethi A., Repici A., Messman H., Chiu P. How to maximize trainee education during the COVID-19 pandemic: perspectives from around the world. Gastroenterology. 2020;159:26–29. doi: 10.1053/j.gastro.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall A.K., Nousiainen M.T., Campisi P., Dagnone J.D., Frank J.R., Kroeker K.I. Training disrupted: practical tips for supporting competency-based medical education during the COVID-19 pandemic. Med Teach. 2020;42:756–761. doi: 10.1080/0142159X.2020.1766669. [DOI] [PubMed] [Google Scholar]
- 9.Codispoti C.D., Bandi S., Moy J.N., Mahdavinia M. Running a virtual allergy division and training program in the time of COVID-19 pandemic. J Allergy Clin Immunol. 2020;145:1357–1359. doi: 10.1016/j.jaci.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agarwal S., Sabadia S., Abou-Fayssal N., Kurzweil A., Balcer L.J., Galetta S.L. Training in neurology: flexibility and adaptability of a neurology training program at the epicenter of COVID-19. Neurology. 2020;94:e2608–e2614. doi: 10.1212/WNL.0000000000009675. [DOI] [PubMed] [Google Scholar]
- 11.Eva K.W., Anderson M.B. Medical education adaptations: really good stuff for educational transition during a pandemic. Med Educ. 2020;54:494. doi: 10.1111/medu.14172. [DOI] [PubMed] [Google Scholar]
- 12.Rosen G.H., Murray K.S., Greene K.L., Pruthi R.S., Richstone L., Mirza M. Effect of COVID-19 on urology residency training: a nationwide survey of program directors by the Society of Academic Urologists. J Urol. 2020;204:1039–1045. doi: 10.1097/JU.0000000000001155. [DOI] [PubMed] [Google Scholar]
- 13.Gupta T, Nazif TM, Vahl TP, Ahmad H, Bortnick AE, Feit F, et al. Impact of the COVID-19 pandemic on interventional cardiology fellowship training in the New York metropolitan area: a perspective from the United States epicenter [published online ahead of print May 16, 2020]. Catheter Cardiovasc Interv. 10.1002/ccd.28977. [DOI] [PMC free article] [PubMed]
- 14.Zingaretti N., Contessi Negrini F., Tel A., Tresoldi M.M., Bresadola V., Parodi P.C. The impact of COVID-19 on plastic surgery residency training. Aesthetic Plast Surg. 2020;44:1381–1385. doi: 10.1007/s00266-020-01789-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Givi B., Moore M.G., Bewley A.F., Coffey C.S., Cohen M.A., Hessel A.C. Advanced head and neck surgery training during the COVID-19 pandemic. Head Neck. 2020;42:1411–1417. doi: 10.1002/hed.26252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ip V., Ozelsel T.J.P., Sondekoppam R.V., Tsui B.C.H. COVID-19 pandemic: the 3R's (reduce, refine, and replace) of personal protective equipment (PPE) sustainability. Can J Anaesth. 2020;67:1070–1071. doi: 10.1007/s12630-020-01653-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Breazzano M.P., Shen J., Abdelhakim A.H., Dagi Glass L., Horowitz J., Xie S.X. New York City COVID-19 resident physician exposure during exponential phase of pandemic. J Clin Invest. 2020;130:4726–4733. doi: 10.1172/JCI139587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention Information for Healthcare Professionals about Coronavirus (COVID-19) https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html Available from: