Figure 3 |.
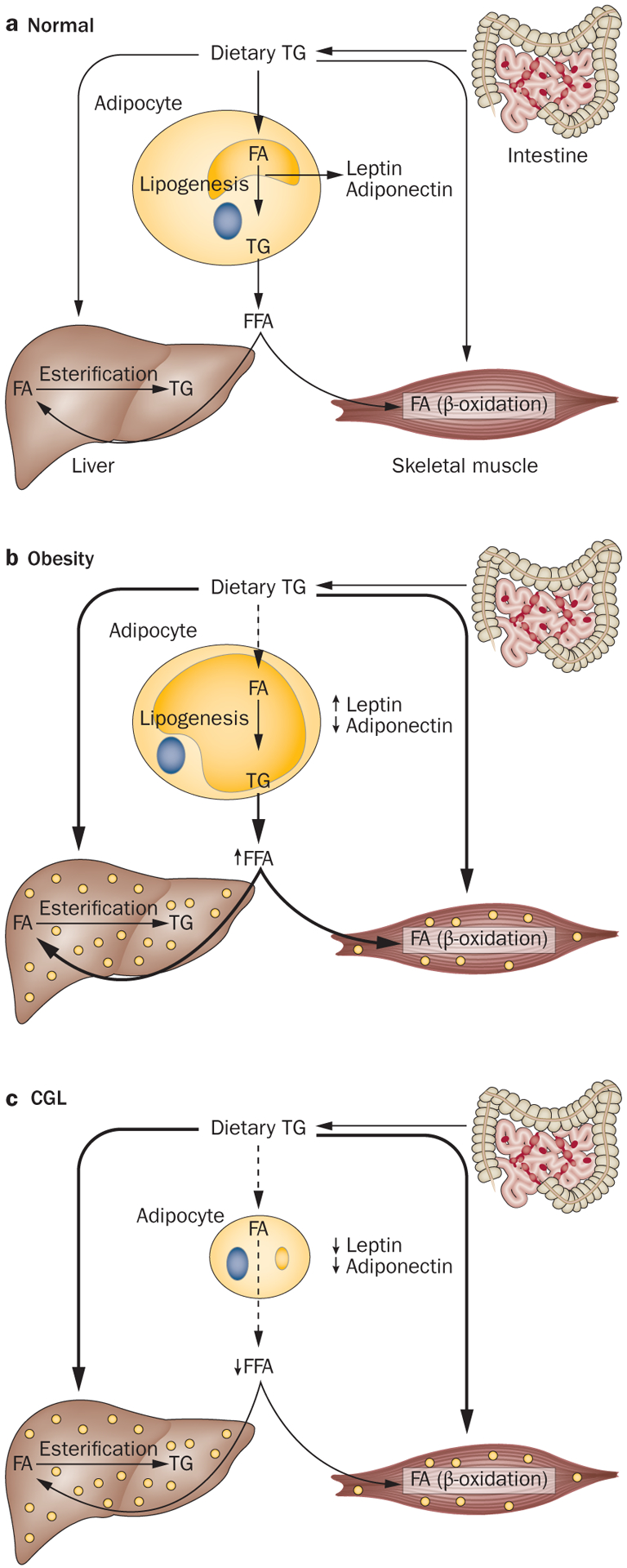
Mechanism of developing metabolic complications in obesity and CGL. a | Under normal conditions, dietary TGs are carried in chylomicrons and provide a source of FFA to the adipose tissue, liver and muscle for further storage and metabolism. Normally, adipocytes have plenty of capacity to store excess dietary TG and thus fewer TGs are directed to the liver and skeletal muscles. Skeletal muscles utilize FA for energy production (β-oxidation). During energy deprivation, the stored TGs are released from the adipocytes to deliver FA to the liver, skeletal muscle and other organs. b | In individuals with generalized or regional adiposity, adipocyte size enlarges and owing to the limited capacity to store more TG, dietary TG might be stored in sites such as the liver and skeletal muscles. Furthermore, lipolysis of excess TG stored in the adipocytes can also contribute to increased FA flux, which can contribute to TG storage in ectopic sites. Uptake of FFA and glucose depends on insulin action, thus in insulin resistance, uptake of FFA and glucose in these tissues is reduced, which might induce hypertriglyceridaemia, hyperglycaemia and hepatic steatosis. c | Patients with CGL lack adipocytes that can store TGs, which limits the disposal of excess dietary TG in the remaining adipocytes and consequently TGs are stored in ectopic sites such as the liver and skeletal muscles. This ectopic storage leads to severe insulin resistance and its complications. A lack of leptin induces hyperphagia, which further exacerbates ectopic storage of TG. Abbreviations: CGL, congenital generalized lipodystrophy; FA, fatty acid; FFA, free fatty acid; TG, triglyceride.
