Structured Abstract
Background:
The U.S. has seen an unprecedented rise in opioid-related morbidity and mortality, and states have passed numerous laws in response. Researchers have not comprehensively established the effectiveness of pain management clinic regulations to reduce opioid prescribing using national data.
Methods:
We combine a policy dataset from the Prescription Drug Abuse Policy System with the Centers for Disease Control and Prevention county-level opioid prescribing data, as well as with numerous government datasets for county- and state- level covariates. We predict retail opioid prescriptions dispensed per 100 people using county fixed-effects models with a state-level cluster correction. Our key predictors of interest are the presence of any state-level pain management clinic law and eight specific subcomponents of the law.
Results:
Pain management clinic laws demonstrate consistent, negative effects on prescribing rates. Controlling for county characteristics, state spending, and the broader policy context, states with pain management clinic laws had, on average, 5.78 fewer opioid prescriptions per 100 people than states without such laws (p<.05). Five specific subcomponents demonstrate efficacy in reducing prescribing rates: certification requirements (B = −6.02, p<.05), medical directors (B = −6.14, p<.05), dispenser and dispensing amount restrictions (B = −8.60, p<.01; B = −15.051, p<.001), and explicit penalties for noncompliance (B = −6.02, p<.05). Three subcomponents had no effect: prescription quantity restrictions and requirements to register with or review prescription drug monitoring programs.
Conclusions:
Implementation of pain management clinic laws reduced county-level opioid prescribing. States should review specific components to determine which forms of law are most efficacious.
Keywords: Opioids, Prescribing practices, Pain management clinics
1. Introduction
1.1. Background
Over the past several decades, the U.S. has seen a rapid rise in drug-related morbidity and mortality (Birnbaum et al., 2011; Dart et al., 2015), creating an unprecedented public health crisis. Opioids have played an enormous role in this crisis, beginning with the increase in prescriptions for opioids such as hydrocodone and oxycodone during the 1990s, and later continuing with increases in heroin and synthetic opioid overdoses. In 2018, approximately 46,802 people in the U.S. died of a drug overdose involving opioids, accounting for over two-thirds of all drug overdose deaths (N. Wilson et al., 2020). Even with conservative estimates, legally prescribed opioids – most of which are prescribed by physicians – account for a substantial number of these deaths (Seth et al., 2018). Estimates suggest that between 21 and 29 percent of patients with opioid prescriptions for chronic pain misuse their medication, and between 8 and 12 percent go on to develop a misuse disorder (Vowles et al., 2015).
Further, legally prescribed opioids can also be diverted to illicit markets, often via “doctor shopping” (McDonald and Carlson, 2013). Still, the majority of original sources of such drugs are legally written prescriptions for the users themselves or for a friend or family member (SAMHSA, 2019). In this manner, opioid medications circulating within networks of people who use drugs often begin from legitimate sources, and the percentage of people who misuse prescription opioids remains overwhelmingly higher than the number of people misusing illicit opioids, such as heroin and fentanyl (SAMHSA, 2019). Ultimately, beyond their own role in overdose deaths, legally prescribed opioids can also indirectly lead to non-prescription opioid-related deaths via transitions to heroin use, with about 80% of people who use heroin having first misused prescription opioids (Muhuri et al., 2013). The potential for transition to heroin, fentanyl, or other illicit opioids (Mars et al. 2014; Strickland and Victor, 2020) may be especially concerning when there are abrupt changes in access, and these illicit opioids account for an increasing number of opioid-related mortality (Scholl et al., 2019). Therefore, via both direct and indirect impacts, reducing unnecessary opioid prescriptions is a critical step in reducing the overall impact of the opioid crisis.
Several policies have been implemented in response to the opioid crisis. Some policies, such as pain management clinic (PMC) regulations or prescription drug monitoring programs, attempt to decrease the supply of opioid medications by reducing unnecessary prescriptions or practices such as doctor shopping. Other laws, such as expanded access to naloxone and Good Samaritan laws, attempt to reduce mortality on the back end by providing opportunities and reducing barriers to intervention following an overdose (Haegerich et al., 2014). These policies are also heterogeneous in nature with their implementation centered on differing mechanisms of action. In this paper, we focus specifically on the role of PMC regulations in addressing the opioid crisis while accounting for the broader policy context in which they have been passed. Policies restricting prescribing via PMCs have seen a range of forms, and these forms may have varied impacts on the opioid crisis. In this paper, we ask to what extent PMC laws reduce county-level opioid prescriptions. If shown to reduce opioid prescribing, such policies could have downstream effects that potentially reduce opioid-related morbidity and mortality.
1.2. Pain Management Clinic Laws
Although the exact form that PMCs take vary from state to state (see Andraka-Christou et al., 2019 for a detailed taxonomy of PMC functions), their primary purpose is to offer services to manage pain, with many directly offering the prescribing and dispensing of controlled substances, mainly opioids. PMC laws, sometimes known as “pill mill” laws, were first passed in the mid-2000s in response to concerns about prescribing practices at PMCs (Rutkow et al., 2017). These practices included on-site pharmacies where prescriptions could be paid for in cash on the spot, sometimes without a medical examination, and with some even allowing patients to choose their own medication (Rigg et al., 2010; Rutkow et al., 2017). Policies were thus implemented to regulate and provide state oversight for PMCs, helping to reduce erratic and inappropriate prescribing practices while preserving opportunities for pain management for those with medical needs. Although states have more often turned to prescription drug monitoring programs to manage inappropriate prescribing and doctor shopping, PMCs have the advantage of targeted oversight for high-risk prescribers while safeguarding access to medically necessary opioids for patients in need (Rutkow et al., 2017).
PMC laws vary from state to state but generally specify guidelines and requirements for the operation of a clinic. These laws can stipulate who can run such a clinic and the type of training they need – some states require that a physician serve as medical director for purposes of oversight and responsibility – as well as specific certification processes required to open a PMC. These laws also specify oversight processes for PMC inspections, including defining the agency responsible for oversight and the schedule of inspection. Some states include additional regulations such as limitations on who can prescribe and dispense opioids in these settings or specify limitations on the amounts prescribed, although differences in these statute stipulations are not well-studied (Rutkow et al., 2017). Given the diversity of PMC laws, further evidence is needed to determine the effects of heterogeneous state processes of oversight and penalties for noncompliant PMCs.
Evidence from studies with limited geographical scope suggests that PMC laws have been effective in reducing opioid prescribing. Many of these studies focus specifically on Florida, which has a notorious reputation regarding pill mills and prescribing practices. In 2011, Florida passed a PMC law at the same time that it passed a prescription drug monitoring program. Following this law, opioid prescriptions and deaths fell sharply in the state (Johnson et al., 2014), driven largely by changes in the prescribing practices of the highest volume prescribers (Chang et al., 2016; Rutkow et al., 2015) and due to successful enforcement activities (Kennedy-Hendricks et al., 2016). These successes are not limited to Florida. For instance, following the PMC law passed in Texas in 2010, the state saw significant declines in monthly opioid prescription volume, number of prescriptions, and average morphine equivalent dose per filled prescription, suggesting that PMC laws can reduce both number of prescriptions and amount of medication per prescription (Lyapustina et al., 2016).
While these studies suggest an important role for PMC laws in reducing prescribing and subsequent overdose deaths, they have typically been geographically limited to one state, which inhibits opportunities to identify specific policy effects. Studies that have expanded this line of inquiry to multiple states find more mixed results. For instance, Dowell and colleagues (2016) find that PMC laws are associated with reductions in state-level prescribing rates, although they find this effect only in combination with prescription drug monitoring programs and find no independent PMC effect. Meara and colleagues (2016) find no relationship at all between PMC laws and prescribing in the U.S., although they rely on individual-level Medicare data for fee-for-service disabled beneficiaries and terminate their analyses in 2012. Their study is therefore limited to a very specific population likely to have a particular relationship with opioids and a timeframe prior to the passage of many PMCs. The evidence is thus ultimately mixed on the efficacy of PMC laws, leaving the relationship between these regulations and opioid prescribing unclear (Mauri et al., 2020) and creating a need for a geographically and temporally expanded study of all prescribing activity.
The current study builds on this existing literature by examining the impact of PMC laws on prescribing practices, although it enhances prior analyses in several ways. First, we include all 50 states in our analysis, further expanding the geographic reach of the inquiry and allowing for the isolation of PMC effects independent of state context. Second, we measure prescribing rates at the county-level, which allows us to take into account important intrastate differences. Given the local nature of pain clinics, particularly within larger states with numerous PMCs, this is especially important for our research questions. Third, we include a robust battery of county- and state-level demographic covariates in a fixed-effects framework that also controls for measured and unmeasured county-level characteristics. Fourth, we include measures of other policies relevant to opioid-prescribing so that we can isolate the effect of PMC laws from other policies with similar aims. Fifth, we not only examine the effect of passing any PMC law, but we examine interstate differences in the specific elements of these laws, which has yet to be studied in detail (Rutkow et al., 2017). Sixth, we use a single, detailed policy database for all state laws rather than relying on multiple datasets and primary data collection efforts, which standardizes the exposure across different types of regulations. As a result, this manuscript provides the most robust estimates to date of the impact of PMC laws on prescribing practices, which relates to their potential efficacy to impact the broader opioid crisis.
2. Methods
2.1. Prescribing Data
We utilized county-level opioid prescribing rate data from the Centers for Disease Control and Prevention (CDC) from 2006 through 2016. Our outcome is retail opioid prescriptions dispensed for 100 people per county in county-year format. The CDC source these data from the IQVIA Xponent, which uses a sample of nearly 50,000 retail pharmacies. Collectively, these pharmacies dispense about 92% of all retail prescriptions in the U.S. The CDC uses Census population estimates for the denominator of the rate, and they identify an opioid prescription using National Drug Codes. Prescriptions for cough and cold medication containing opioids, as well as methadone and buprenorphine products prescribed for opioid addiction treatment, are not included in these estimates (CDC, 2020).
2.2. Policy Data
We utilized the Prescription Drug Abuse Policy System (PDAPS) for a comprehensive and detailed listing of policy passage in each state between 2000 and 2016 (PDAPS, n.d.). We begin the present analyses in 2006, as that year marks the beginning of the availability of the prescribing data. We then created a state-year dataset of the presence of policies across the observation period, with policies coded as 1 when they were active as of January 1st, and 0 otherwise. To account for other policies that may affect prescribing rates, we included controls for prescription drug monitoring programs, expanded naloxone access to the lay public, Good Samaritan laws absolving criminal or civil liability when reporting an overdose, and presence of medical marijuana laws, which were not necessarily passed in response to the overdose crisis but are nonetheless an important policy covariate given their applicability to pain management.
2.3. County- and State-level Covariates
From the U.S. Census Bureau’s American Community Survey (ACS) and Decennial Censuses, we draw county- and state-level covariates that account for key contextual socio-demographic and expenditure factors based on demonstrated importance in past literature (e.g. Guy et al., 2017; McDonald et al., 2012; F. A. Wilson et al., 2020). Specifically, we included the following county-level time-varying covariates: the unemployment rate, median household income, and percentages foreign-born, female-headed households, Black Non-Hispanic, Hispanic, and over 25 with a Bachelor’s. We include an interaction between percentage foreign-born and Hispanic given their high correlation. We used the 5-year ACS estimates because only larger counties are available with shorter estimates. As these begin in 2009, we linearly interpolated the years between the 2000 census and 2009, utilizing the interpolated values beginning in 2006. From the Annual Survey of State Government Finances, we included state-level per-capita spending on education, public welfare, hospitals, and health.
2.4. Analysis
We used fixed-effects ordinary least squares linear regression models to determine the effect of PMCs on the county-level opioid prescribing rate. Fixed effects models eliminate unobserved heterogeneity by differencing all predictors and the outcome from its county-specific average. Fixed-effects estimators are robust to any observed or unobserved time-invariant omitted variables, which removes any constant county-level effects and allows the variable of interest to operate as a “treatment” effect in a traditional experiment (Allison, 2009; Halaby, 2004; Winship and Morgan, 1999). We included a standard error cluster-correction using Huber/White Sandwich estimators (Huber, 1967; White, 1980) at the state level to account for dependencies between counties within states. We conducted all analyses using Stata.
We began by modeling the effect of any PMC law in three blocks. The first block includes a binary indicator for presence of a PMC law and fixed effects for years and county. The second block adds the county-level covariates with a one-year lag, while the third block adds indicators for additional relevant policies. We then modeled the effects of eight specific elements of PMC laws: certification requirements, restrictions on who can dispense, limitations on the amount of medication that can be dispensed, limitations on the amount of medication that can be prescribed, explicit penalties for noncompliance, a requirement for a medical director, a requirement that PMC doctors register with the PDMP, and a requirement that PMC doctors review the PDMP. Each of these elements was present in some, but not all, of the state PMC laws across years, and examining their effects helps to determine the most impactful elements of PMC laws to reduce prescribing rates. In determining these eight elements, we drew on literature highlighting the large diversity in PMC laws (Andraka-Christou et al., 2019; Rutkow et al., 2017) and included the core policy elements available for our time series and present in at least one state law prior to the final year in our analysis.
While there are a total of 3,149 unique U.S. counties as of 2016, the number of counties in our analysis range from 2,637 in 2012 to 2,851 in 2015, with the N in other years falling in-between, for a total of 30,798 county-year observations. Missing counties primarily result from incomplete CDC prescribing data, which contain rates for 87.6% to 94.0% of counties in a given year. Missing data can indicate that “the county had no retail pharmacies, the county had no retail pharmacies sampled, or the prescription volume was erroneously attributed to an adjacent, more populous county according to the sampling rules used” (CDC, 2020, note 5).
3. Results
3.1. Descriptive Statistics
As Figure 1 shows, average county-level opioid prescribing rates rose from 80.5 per 100 in 2006 to a high of 96.1 per 100 in 2012, at which point rates began to steadily decline. The pooled average across the analytic sample was 87.1. Figure 2 shows the main predictors of interest by plotting the percentage of states per year with an overall PMC law and each of the sub-components of the law. Table 1 shows the descriptive statistics. Across the pooled sample, 16.55% of county-year observations had a PMC law. As of 2006, Louisiana was the only state to have passed a legal regulation regarding PMCs. By 2016, nine other states had passed such laws. However, not all laws have included the same regulations. Certification and medical director requirements, along with explicit penalties for noncompliance, all rose steadily as components of PMC laws beginning around 2011. Restrictions on dispensers, restrictions on the amount prescribed or dispensed, and requirements to register or review the prescription drug monitoring program were less commonly included in laws. Limits on amount dispensed remained the least common regulation, consisting of only 0.71% of the county-year observations, as this law was passed in only one state during our time series.
Figure 1. County Average Prescribing Rate per 100.
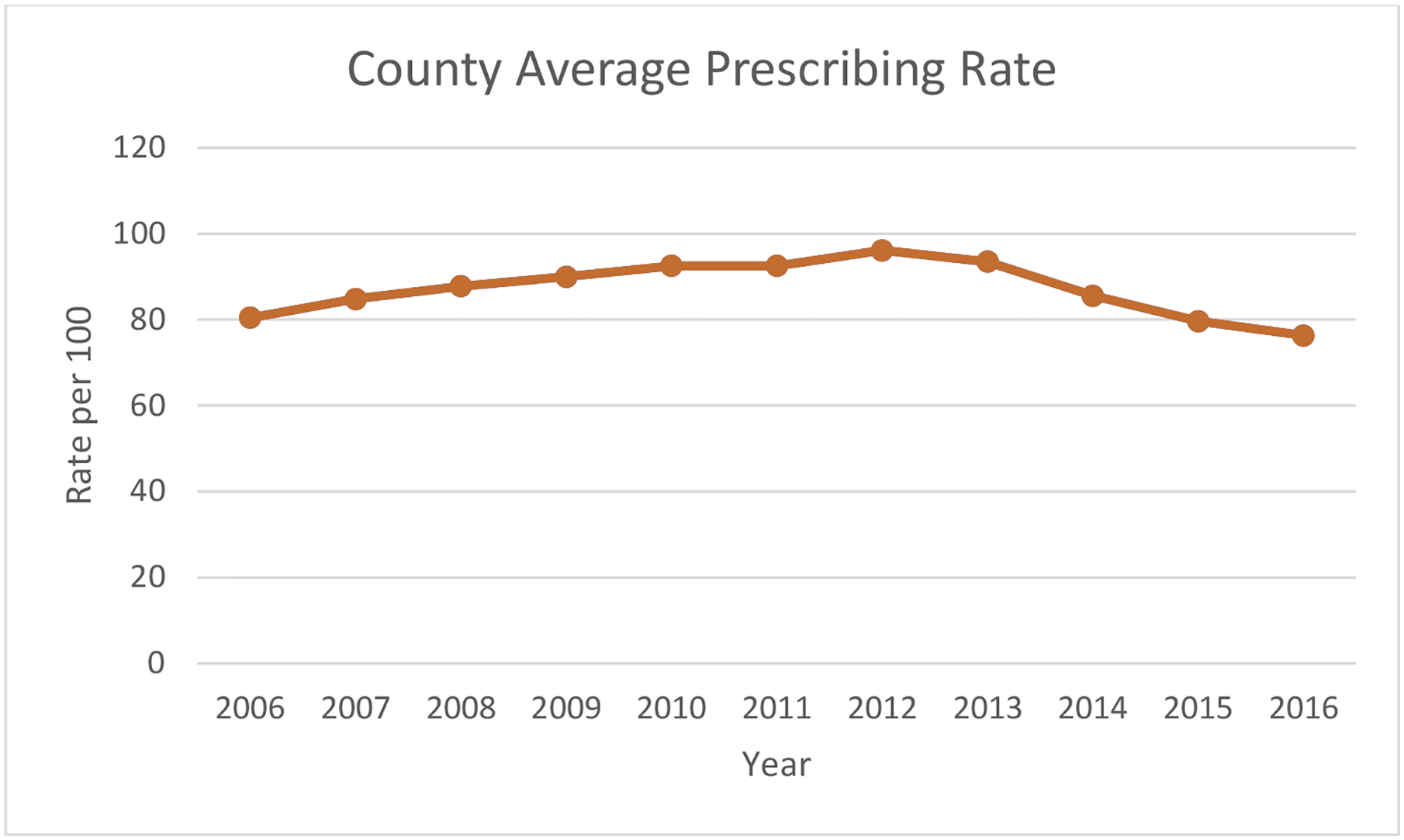
County Average Prescribing Rate per 100
Figure 2. Percentage of States with Pain Management Clinic Laws and Specific Regulations.
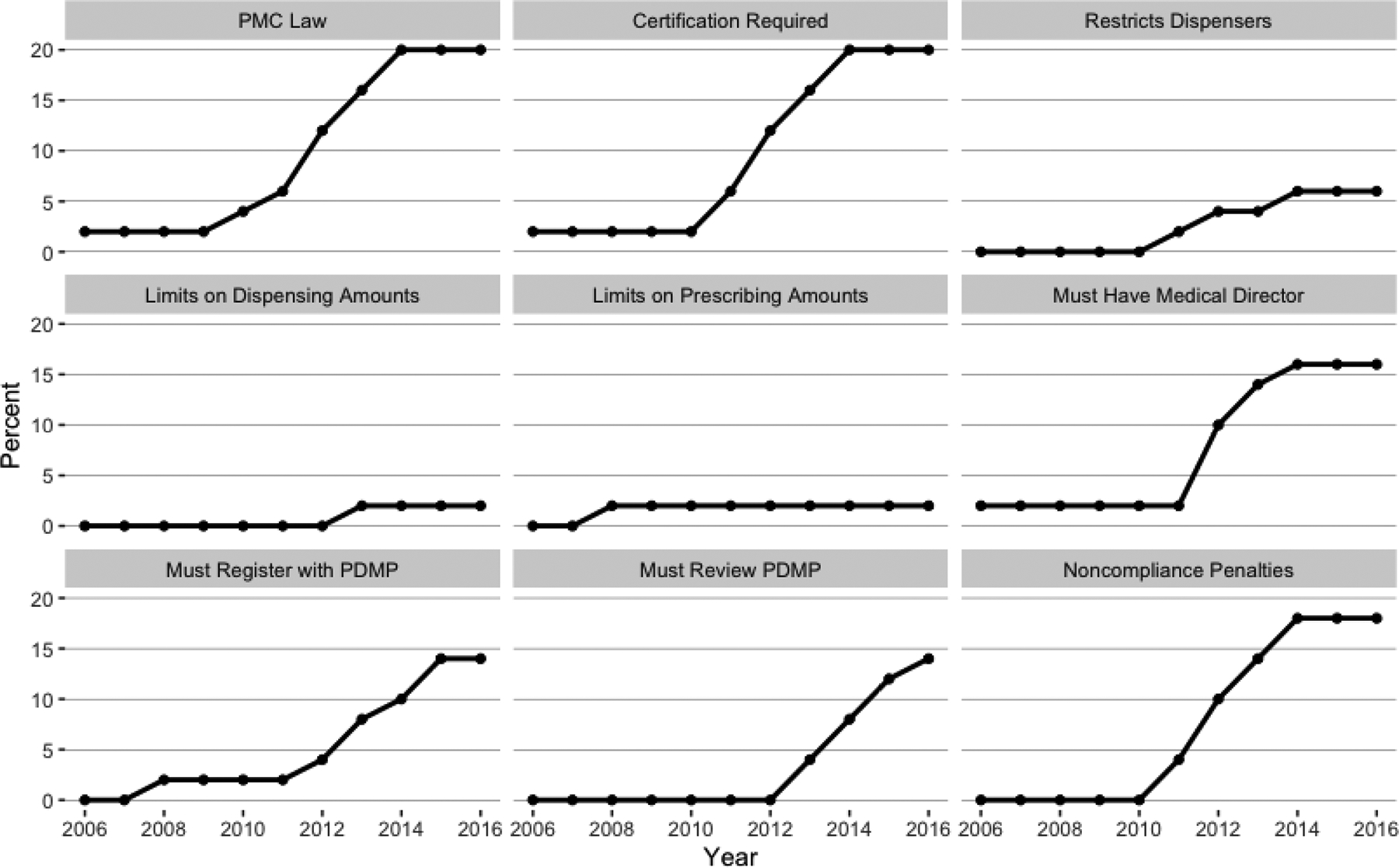
Percentage of States with Pain Management Clinic Laws and Specific Regulations
Table 1.
Descriptive statistics (pooled over counties and year 2000 to 2016, N = 30,798)
| Average/% (SD) | |
|---|---|
| County-level Average Prescribing Rate per 100 | 87.11 (47.63) |
| State Pain Management Clinic Policies | |
| Pain management clinic law | 16.55% |
| Certification required | 15.95% |
| Explicit penalties for noncompliance | 13.85% |
| Requires a medical director | 13.05% |
| Restricts who can dispense | 3.37% |
| Limits supply of medication doctors can dispense | 0.71% |
| Restricts amount that can be prescribed | 1.73% |
| Doctors must register with PDMP | 7.97% |
| Doctors must review PDMP | 5.64% |
| Additional State-level Policies | |
| PDMP system | 83.30% |
| Naloxone access law | 21.85% |
| Good Samaritan law for drug overdose | 14.54% |
| Medical marijuana | 18.33% |
| County-level Demographics | |
| Unemployment rate | 4.55 (1.68) |
| Median household income ($) | 44,918.67 (11,974.47) |
| Percent living in poverty | 11.68 (5.45) |
| Percent with bachelor’s degree | 14.59 (7.20) |
| Percent foreign-born | 4.42 (5.39) |
| Percent female-headed households | 6.57 (2.33) |
| Percent Black | 9.61 (14.26) |
| Percent Hispanic | 8.21 (12.62) |
| State-level Per Capita Expenditures ($) | |
| Education | 1.91 (.39) |
| Public Welfare | 1.47 (.42) |
| Hospitals | .21 (.15) |
| Health | .17 (.08) |
Regarding county-level demographics, the median household income was $44,918.67 with 9.61% Black and 8.21% Hispanic residents. Counties had an average unemployment rate of 4.55% with an average of 11.68% of people living in poverty and 14.59% with a Bachelor’s degree. Finally, counties had an average of 6.57% of female-headed households and 4.42% foreign-born residents. State expenditures per capita ranged from an average across county-years of $1.91 on education to $0.17 on health, with $1.47 spent on public welfare and $0.21 spent on hospitals. Finally, the majority of county-years had state-level Prescription Drug Monitoring Program laws (83.30%), with fewer having naloxone access laws (21.85%), medical marijuana laws (18.33%), or Good Samaritan laws (14.54%).
3.2. Models
As shown in Table 2, pain management clinic laws demonstrate consistent, negative effects on opioid prescribing rates. Controlling only for county and year fixed effects, counties in states with PMC laws had, on average, 5.58 fewer opioid prescriptions per 100 people (p<.05). The pattern of the magnitude of the year effects controlling for PMC laws is shown in Figure 3, with 2006 as the index baseline. The PMC effect remained when controlling for county-level factors (B = −6.06 in Block 2), of which only the unemployment rate, percent female-headed households, and the main effect for percent Hispanic were significant (B = .69, B = −.70 and B = −.74 respectively). When adding additional policies relevant to prescribing in Block 3, the effect of PMC laws remained robust; states with PMC laws had, on average, 5.78 fewer prescriptions per 100 people than states without such laws net of demographic factors and the broader policy context (p<.05).
Table 2.
Nested Fixed-effects Panel Models of County Prescribing Rates
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Pain Management Clinic | −5.68* | −6.06* | −5.78* |
| (2.63) | (2.50) | (2.40) | |
| Year | |||
| 2007 | 4.09*** | 4.64*** | 4.60*** |
| (.43) | (.66) | (.63) | |
| 2008 | 7.15*** | 8.39*** | 8.31*** |
| (.68) | (1.24) | (1.19) | |
| 2009 | 9.20*** | 11.33*** | 11.33*** |
| (.79) | (1.63) | (1.62) | |
| 2010 | 12.01*** | 14.90*** | 14.88*** |
| (.88) | (1.77) | (1.71) | |
| 2011 | 12.04*** | 15.92*** | 15.85*** |
| (.93) | (2.05) | (2.07) | |
| 2012 | 15.94*** | 19.85*** | 19.68*** |
| (.95) | (1.82) | (1.90) | |
| 2013 | 13.85*** | 18.06*** | 17.91*** |
| (.95) | (1.87) | (1.93) | |
| 2014 | 11.22*** | 15.19*** | 15.41*** |
| (1.21) | (2.44) | (2.44) | |
| 2015 | 5.32*** | 10.70** | 11.61*** |
| (1.22) | (2.94) | (2.98) | |
| 2016 | 1.93 | 8.17* | 9.87** |
| (1.22) | (3.12) | (3.09) | |
| Unemployment rate | .69* | .72* | |
| (.33) | (.33) | ||
| Median household income (Thousands) | −.21 | −.23 | |
| (.13) | (.13) | ||
| Percent living in Poverty | .21 | .21 | |
| (.15) | (.15) | ||
| Percent with Bachelor’s degree | −.11 | −.11 | |
| (.08) | (.08) | ||
| Percent foreign-born | .22 | .21 | |
| (.41) | (.42) | ||
| Percent female-headed households | −.70** | −.71** | |
| (.23) | (.23) | ||
| Percent Black | −.61 | −.64 | |
| (.43) | (.43) | ||
| Percent Hispanic | −.74* | −.73* | |
| (.34) | (.33) | ||
| Percent Hispanic*Percent Foreign Born | −.01 | −.01 | |
| (.01) | (.01) | ||
| State education expenditures | −1.43 | −1.75 | |
| (2.91) | (2.92) | ||
| State public welfare expenditures | −6.12 | −6.19 | |
| (3.71) | (3.65) | ||
| State hospital expenditures | 8.45 | 8.26 | |
| (8.20) | (8.10) | ||
| State health expenditures | 8.01 | 7.55 | |
| (6.59) | (6.52) | ||
| PDMP system | .82 | ||
| (1.55) | |||
| Naloxone access law | −1.92 | ||
| (1.28) | |||
| Good Samaritan law | −1.11 | ||
| (1.28) | |||
| Medical marijuana law | 1.86 | ||
| (1.33) | |||
| Constant | 79.67*** | 107.14*** | 108.08*** |
| (.68) | (10.19) | (10.09) | |
| Observations | 30,798 | 30,798 | 30,798 |
Note: Models include state-level cluster corrected standard errors.
Figure 3. Marginal Year Effects Controlling for PMC Law.
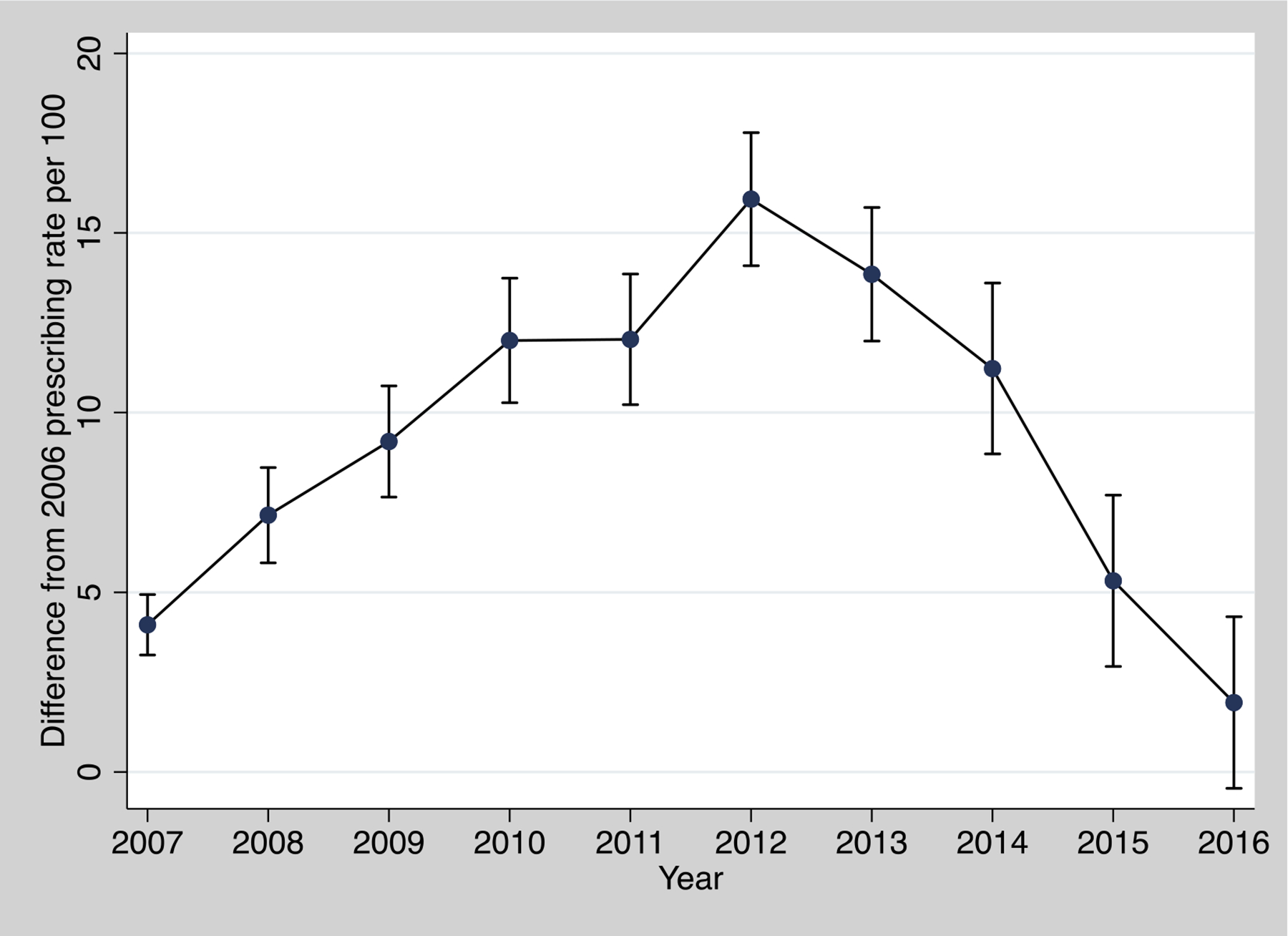
Marginal Year Effects Controlling for PMC Law
While this finding is substantial on its own, it does not take into account the differences in specific elements of these laws. We therefore model eight additional subcomponents that are present in some, but not all, PMC laws. Table 3 shows these results, which shows just the coefficients for the differing PMC policies since the covariate findings remain similar to that in Table 2 (full models are shown in Appendix A). Five components demonstrate efficacy in reducing prescribing rates, with certification requirements, requirement to have a medical director, and explicit penalties for noncompliance all reducing average prescriptions by approximately 6 per 100 people (p<.05), net of policy predictors and county-level demographics. Dispenser restrictions and limitations on the amount of medication that can be dispensed had even larger effects, reducing the average prescribing rate by 8.6 (p<.01) and 15.5 (p<.001) per 100 people respectively. In contrast, restrictions on prescribing amounts and requirements to review or register with the state’s prescription drug monitoring program had no significant effect on the average county prescribing rate.
Table 3.
Specific Pain Management Clinic Policy Effects from Fixed-effects Panel Models of County Prescribing Rates
| Coefficient (SE) | |
|---|---|
| PMC certification required | −6.02* (2.32) |
| PMC law restricts dispensers | −8.60** (2.50) |
| PMC must have a medical director | −6.14* (2.74) |
| Explicit penalties for noncompliance | −6.02* (2.32) |
| PMC law limits amount that can be dispensed | −15.51*** (2.15) |
| PMC law restricts amount that can be prescribed | 1.74 (1.16) |
| PMC doctors must register with PDMP | −3.84 (3.40) |
| PMC doctors must review PDMP | −6.65 (3.76) |
Note: Covariates are from separate models that include all covariates in Table 2. Full models areincluded in Appendix A.
4. Discussion
During the opioid crisis, states have passed numerous policies in attempts to reduce morbidity and mortality. Since adverse outcomes have been heavily driven by legal prescriptions (e.g. Seth et al., 2018), some policies, such as pain management clinic laws, attempted to intervene on unnecessary or inappropriate opioid prescriptions. Our study suggests that PMC laws were significantly and substantively effective. When considering the passage of any PMC regulation, county-level prescribing rates decreased by an average of 5.78 per 100 people following passage net of static county-level effects as well as time-varying county-level demographic factors, state-level expenditures, and the broader policy context. When considering specific elements of PMC policies, five that we tested were significant in reducing prescribing rates, with prescription limitations lowering the prescribing rate by an average of 15.4 per 100 people, the most of any subcomponent. Such drastic reductions in prescribing practices can have real and prolonged effects on morbidity and mortality due to the circulation of prescription opioids in communities. Given the potential for transition from prescription to illicit opioids (Mars et al., 2014; Scholl et al., 2019; Strickland and Victor, 2020), these results may also indirectly impact use of and dependence on illicit opioids by limiting prescription opioid misuse.
Despite these effects, only 20% of states had passed any form of PMC regulation as of 2016. Although not included in our dataset, only one additional state has since passed such a law (PDAPS, n.d.). Thus, there is an enormous opportunity for states that have not yet passed PMC laws to intervene on problematic prescribing practices that adversely impact population health. Further, our study suggests that PMC laws may be most effective when including a variety of specific measures, including requiring certification of all PMCs in the state, restricting which healthcare providers can dispense opioids in PMCs, requiring a medical director at each PMC, limiting the amount of opioids that can be dispensed, and laying out explicit penalties for noncompliance. In contrast, policies restricting prescription amounts or requiring PMCs to register with or review prescription drug monitoring programs thus far have had less impact in reducing overall prescribing rates, although we nonetheless do not discourage states from adopting such policies. Notably, no other policies displayed a direct effect on the county-level prescribing rate net of PMCs, further highlighting the direct importance of these policies for reducing opioid prescribing.
4.1. Limitations
While we take substantial steps to address potential issues with our study, it nonetheless has some limitations. First, counties are imperfect measures of geographic space, and measuring prescribing rates at this level can obfuscate important within-county level differentiation. The size and number of counties also vary considerably across states. However, they are a substantial improvement over measuring prescribing at the state level given the local nature of PMCs, and fixed-effects models allow us to net out any stable differences between counties, such as their size. Second, data limitations preclude us from using a more refined time measurement than county-year (such as county-month), which would allow for a more detailed and precise measurement of the timeliness of policy impact. Third, some of the specific elements of PMC laws that we measure are rare and have only been included in more recent laws. This is especially true for limitations on the supply of medication that doctors can dispense, which only exist in one state for 0.71% of our county-year observations. Fourth and relatedly, other specific elements exist in the majority of PMC laws, with requirements for certification differing from the main law in only one year. Nonetheless, the stronger coefficient for this sub-policy when compared to the overall law suggests that its inclusion in PMC laws is important to maximally reducing prescribing rates. Thus, while exactly which subcomponents might on their own affect prescribing is difficult to adjudicate, we believe the best approach is to consider them a package of approaches that can be passed for maximal benefit. As PMC laws expand and become more common, future research should continue to determine additional elements of such laws that are efficacious in tandem with those we have identified. Fifth and relatedly, we cannot take into account the degree of enforcement of laws, only their presence/absence, although prior studies have suggested that measuring enforcement is important to understanding PMC laws’ impacts (Kennedy-Hendricks et al., 2016). However, to the extent that this biases our results, it likely produces conservative estimates. Finally, we include a large number of county- and state- level covariates relevant to prescribing practices. While there is the possibility that other relevant variables are omitted, again the use of fixed-effects models means that only the omission of time-varying covariates could potentially bias the results.
5. Conclusions
The U.S. has experienced an unprecedented rise in opioid-related deaths, and regulating pain management clinics remains an underutilized tool to reduce opioid prescribing. Such a reduction could, in turn, reduce opioid morbidity and mortality by reducing the supply of legally prescribed drugs circulating within communities. States should consider passing PMC laws that have specific guidelines for dispensing, the presence of medical directors, the requirements for clinic certification, and clear penalties for noncompliance with these regulations. While there are not yet sufficient data to test the interactive effects of such policies, each has demonstrated independent efficacy to reduce county-level prescribing rates by between 6.0 and 15.4 prescriptions per 100 people, net of county-level, state-level, or policy covariates. Although recent years have seen a reduction in opioid prescriptions, further reductions via expansion of PMC laws could save countless lives while retaining access to care for patients with pain conditions.
Highlights.
Pain management clinic laws reduce county-level opioid prescribing
Specific aspects of pain management clinic laws impact opioid prescribing differently
Pain management clinic laws can help states fight the opioid crisis
Role of the funding source
This work was funded by the National Institute on Drug Abuse (grant # R21DA046447). The funding agency had no role in the research; the views expressed in this paper do not represent those of the funding agency.
Abbreviations:
- PMC
Pain Management Clinic
- CDC
Centers for Disease Control and Prevention
- ACS
American Community Survey
- PDMP
Prescription Drug Monitoring Program
Appendix A. Fixed-effects Panel Models of County Prescribing Rates with Specific Pain Management Clinic Policies
| PMC certification required | PMC law restricts dispensers | PMC must have a medical director | Explicit penalties for noncompliance | PMC law limits amount that can be dispensed | PMC law restricts amount that can be prescribed | PMC doctors must register with PDMP | PMC doctors must review PDMP | |
|---|---|---|---|---|---|---|---|---|
| Pain Management Clinic Law | −6.02* | −8.60** | −6.14* | −6.02* | −15.51*** | 1.74 | −3.84 | −6.65 |
| (2.32) | (2.50) | (2.74) | (2.32) | (2.15) | (1.16) | (3.40) | (3.76) | |
| Year | ||||||||
| 2007 | 4.65*** | 4.52*** | 4.58*** | 4.65*** | 4.38*** | 4.34*** | 4.50*** | 4.62*** |
| (.62) | (.63) | (.63) | (.62) | (.61) | (.63) | (.65) | (.65) | |
| 2008 | 8.41*** | 8.14*** | 8.21*** | 8.41*** | 7.84*** | 7.75*** | 8.20*** | 8.37*** |
| (1.15) | (1.13) | (1.19) | (1.15) | (1.12) | (1.14) | (1.21) | (1.23) | |
| 2009 | 11.46*** | 11.13*** | 11.16*** | 11.46*** | 10.67*** | 10.66*** | 11.17*** | 11.37*** |
| (1.57) | (1.55) | (1.59) | (1.57) | (1.54) | (1.56) | (1.62) | (1.64) | |
| 2010 | 14.64*** | 14.27*** | 14.28*** | 14.64*** | 13.71*** | 13.75*** | 14.29*** | 14.53*** |
| (1.77) | (1.75) | (1.77) | (1.77) | (1.76) | (1.77) | (1.85) | (1.88) | |
| 2011 | 16.06*** | 15.14*** | 15.69*** | 16.06*** | 14.34*** | 14.45*** | 15.06*** | 15.20*** |
| (2.06) | (2.10) | (2.13) | (2.06) | (2.12) | (2.12) | (2.21) | (2.19) | |
| 2012 | 19.92*** | 18.64*** | 19.40*** | 19.92*** | 17.59*** | 17.62*** | 18.38*** | 18.53*** |
| (1.88) | (2.07) | (2.08) | (1.88) | (2.04) | (2.05) | (2.09) | (2.07) | |
| 2013 | 18.19*** | 16.45*** | 17.66*** | 18.19*** | 15.64*** | 15.38*** | 16.49*** | 16.76*** |
| (1.86) | (2.19) | (2.10) | (1.86) | (2.11) | (2.14) | (2.11) | (2.11) | |
| 2014 | 15.70*** | 13.85*** | 14.82*** | 15.70*** | 12.73*** | 12.48*** | 13.61*** | 14.32*** |
| (2.35) | (2.26) | (2.41) | (2.35) | (2.26) | (2.26) | (2.44) | (2.51) | |
| 2015 | 11.94*** | 10.07*** | 10.97*** | 11.94*** | 8.78** | 8.68** | 10.02** | 10.79** |
| (2.87) | (2.69) | (2.85) | (2.87) | (2.75) | (2.72) | (3.05) | (3.14) | |
| 2016 | 10.25** | 8.40** | 9.25** | 10.25** | 6.93* | 6.78* | 8.07* | 9.07** |
| (2.99) | (2.82) | (3.03) | (2.99) | (2.94) | (2.94) | (3.24) | (3.30) | |
| Unemployment rate | .71* | .77* | .70* | .71* | .67 | .67 | .67 | .64 |
| (.33) | (.34) | (.33) | (.33) | (.35) | (.35) | (.35) | (.35) | |
| Median household income | −.22 | −.19 | −.19 | −.22 | −.16 | −.16 | −.19 | −.21 |
| (Thousands) | (.13) | (.13) | (.13) | (.13) | (.12) | (.13) | (.13) | (.13) |
| Percent living in Poverty | .20 | .22 | .16 | .20 | .19 | .25 | .24 | .23 |
| (.15) | (.14) | (.16) | (.15) | (.13) | (.15) | (.16) | (.15) | |
| Percent with Bachelor’s | −.11 | −.09 | −.12 | −.11 | −.10 | −.10 | −.10 | −.08 |
| degree | (.08) | (.07) | (.08) | (.08) | (.07) | (.07) | (.07) | (.07) |
| Percent foreign-born | .20 | .20 | .18 | .20 | .25 | .26 | .31 | .31 |
| (.42) | (.44) | (.43) | (.42) | (.44) | (.44) | (.44) | (.44) | |
| Percent female-headed | −.71** | −.69** | −.67** | −.71** | −.67** | −.69** | −.71** | −.70** |
| households | (.24) | (.24) | (.24) | (.24) | (.24) | (.24) | (.23) | (.24) |
| Percent Black | −.66 | −.61 | −.67 | −.66 | −.57 | −.58 | −.55 | −.55 |
| (.43) | (.44) | (.44) | (.43) | (.44) | (.43) | (.44) | (.45) | |
| Percent Hispanic | −.75* | −.72* | −.69* | −.75* | −.77* | −.70* | −.80* | −.86** |
| (.33) | (.32) | (.34) | (.33) | (.32) | (.33) | (.33) | (.32) | |
| Percent Hispanic*Percent | −.01 | −.01 | −.01 | −.01 | −.02 | −.02 | −.02 | −.02 |
| Foreign Born | (.01) | (.01) | (.01) | (.01) | (.01) | (.01) | (.01) | (.01) |
| State education expenditures | −2.10 | −.93 | −1.12 | −2.10 | −1.11 | −.93 | −1.71 | −2.04 |
| (2.80) | (2.93) | (3.10) | (2.80) | (3.09) | (3.09) | (2.84) | (2.83) | |
| State public welfare | −6.33 | −6.52 | −5.87 | −6.33 | −4.96 | −6.59 | −6.23 | −5.49 |
| expenditures | (3.64) | (3.87) | (3.45) | (3.64) | (4.15) | (4.23) | (4.01) | (3.60) |
| State hospital expenditures | 8.53 | 5.05 | 7.73 | 8.53 | 7.16 | 8.96 | 8.96 | 3.69 |
| (8.07) | (7.89) | (8.22) | (8.07) | (8.20) | (9.03) | (8.87) | (10.51) | |
| State health expenditures | 6.84 | 4.68 | 5.79 | 6.84 | 12.84 | 12.78 | 8.75 | 8.65 |
| (6.54) | (7.47) | (6.56) | (6.54) | (7.06) | (6.96) | (6.73) | (6.41) | |
| PDMP system | .78 | 1.27 | .44 | .78 | .88 | 1.11 | 1.06 | .99 |
| (1.55) | (1.59) | (1.50) | (1.55) | (1.64) | (1.69) | (1.65) | (1.62) | |
| Naloxone access law | −1.92 | −2.41 | −2.14 | −1.92 | −2.40 | −2.25 | −1.68 | −1.44 |
| (1.28) | (1.57) | (1.32) | (1.28) | (1.63) | (1.60) | (1.27) | (1.26) | |
| Good Samaritan law | −1.18 | −.58 | −1.18 | −1.18 | −.92 | −.82 | −.97 | −.87 |
| (1.29) | (1.35) | (1.33) | (1.29) | (1.49) | (1.45) | (1.37) | (1.45) | |
| Medical marijuana law | 1.81 | 2.35 | 1.86 | 1.81 | 2.54 | 3.03 | 2.61 | 2.16 |
| (1.33) | (1.47) | (1.28) | (1.33) | (1.51) | (1.57) | (1.39) | (1.16) | |
| Constant | 109.03*** | 105.30*** | 106.10*** | 108.90*** | 101.67*** | 101.76*** | 105.14*** | 107.13*** |
| (9.79) | (9.56) | (9.77) | (9.80) | (9.77) | (9.79) | (10.11) | (10.41) | |
| Observations | 30,798 | 30,798 | 30,798 | 30,798 | 30,798 | 30,798 | 30,798 | 30,798 |
Note: Models include state-level cluster corrected standard errors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
None declared.
Declaration of interests
All authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Allison P, 2009. Fixed Effects Regression Models. SAGE Publications, Thousand Oaks, CA. [Google Scholar]
- Andraka-Christou BT, Rager JB, Brown-Podgorski B, Silverman RD, Watson DP, 2019. An integrative systematic review of the medical literature on pain clinic definitions and comparison with existing state laws and regulations. Subst Abuse Treat Prev Policy 13, 17 10.1186/s13011-018-0163-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL, 2011. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med 12(4), 657–667. 10.1111/j.1526-4637.2011.01075.x [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC), 2020. U.S. Opioid Prescribing Rate Maps. https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html (accessed 5.17.20).
- Chang H-Y, Lyapustina T, Rutkow L, Daubresse M, Richey M, Faul M, Stuart EA, Alexander GC, 2016. Impact of prescription drug monitoring programs and pill mill laws on high-risk opioid prescribers: A comparative interrupted time series analysis. Drug Alcohol Depend 165(1), 1–8. 10.1016/j.drugalcdep.2016.04.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dart RC, Surratt HL, Cicero TJ, Parrino MW, Severtson SG, Bucher-Bartelson B, Green JL, 2015. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med 372, 241–248. 10.1056/NEJMsa1406143 [DOI] [PubMed] [Google Scholar]
- Dowell D, Zhang K, Noonan RK, Hockenberry JM, 2016. Mandatory provider review and pain clinic laws reduce the amounts of opioids prescribed and overdose death rates. Health Aff 35(10), 1876–1883. 10.1377/hlthaff.2016.0448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy GP Jr., Zhang K, Bohm MK, Losby J, Lewis B, Young R, Murphy LB, Dowell D, 2017. Vital signs: Changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep 66(26), 697–704. 10.15585/mmwr.mm6626a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haegerich TM, Paulozzi LJ, Manns BJ, Jones CM, 2014. What we know, and don’t know, about the impact of state policy and systems-level interventions on prescription drug overdose. Drug Alcohol Depend 145(1), 34–47. 10.1016/j.drugalcdep.2014.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halaby CN, 2004. Panel models in sociological research: Theory into practice. Annu Rev Sociol 30, 507–544. 10.1146/annurev.soc.30.012703.110629 [DOI] [Google Scholar]
- Huber PJ, 1967. The behavior of maximum likelihood estimates under nonstandard conditions, in: Kojima K (Ed.), Proceedings of the fifth Berkeley symposium on mathematical statistics and probability. University of California Press, Berkeley, pp. 221–233. [Google Scholar]
- Johnson H, Paulozzi L, Porucznik C, Mack K, Herter B, 2014. Decline in drug overdose deaths after state policy changes — Florida, 2010–2012. MMWR Morb Mortal Wkly Rep 63, 569–574. [PMC free article] [PubMed] [Google Scholar]
- Kennedy-Hendricks A, Richey M, McGinty EE, Stuart EA, Barry CL, Webster DW, 2016. Opioid overdose deaths and Florida’s crackdown on pill mills. Am J Public Health 106(2), 291–297. 10.2105/AJPH.2015.302953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyapustina T, Rutkow L, Chang H-Y, Daubresse M, Ramji AF, Faul M, Stuart EA, Alexander GC, 2016. Effect of a “pill mill” law on opioid prescribing and utilization: The case of Texas. Drug Alcohol Depend 159(1), 190–197. 10.1016/j.drugalcdep.2015.12.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Bourgois P, Karandinos G, Montero F, Ciccarone D, 2014. “Every ‘never’ I ever said came true”: Transitions from opioid pills to heroin injecting. Int J Drug Policy 25(2), 257–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauri AI, Townsend TN, Haffajee RL, 2020. The association of state opioid misuse prevention policies with patient- and provider-related outcomes: A scoping review. Milbank Q 98, 57–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald DC, Carlson K, Izrael D, 2012. Geographic variation in opioid prescribing in the U.S. J Pain 13(10), 988–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald DC, Carlson KE, 2013. Estimating the prevalence of opioid diversion by “doctor shoppers” in the United States. PLOS ONE 8, e69241 10.1371/journal.pone.0069241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meara E, Horwitz JR, Powell W, McClelland L, Zhou W, O’Malley AJ, Morden NE, 2016. State legal restrictions and prescription-opioid use among disabled adults. N Engl J Med 375, 44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhuri PK, Gfroerer JC, Davies MC, 2013. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States. SAMHSA, Rockville, MD. [Google Scholar]
- Prescription Drug Abuse Policy System (PDAPS), n.d. http://pdaps.org/ (accessed 5.17.20).
- Rigg KK, March SJ, Inciardi JA, 2010. Prescription drug abuse & diversion: Role of the pain clinic. J Drug Issues 40(3), 681–701. 10.1177/002204261004000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutkow L, Chang H-Y, Daubresse M, Webster DW, Stuart EA, Alexander GC, 2015. Effect of Florida’s prescription drug monitoring program and pill mill laws on opioid prescribing and use. JAMA Intern Med 175(10), 1642–1649. 10.1001/jamainternmed.2015.3931 [DOI] [PubMed] [Google Scholar]
- Rutkow L, Vernick JS, Alexander GC, 2017. More states should regulate pain management clinics to promote public health. Am J Public Health 107(2), 240–243. 10.2105/AJPH.2016.303568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G, 2019. Drug and opioid-involved overdose deaths – United States, 2013–2017. MMWR Morb Mortal Wkly Rep 67(51–52), 1419–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seth P, Rudd RA, Noonan RK, Haegerich TM, 2018. Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health 108(4), 500–502. 10.2105/AJPH.2017.304265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickland JC, Victor GA, 2020. Leveraging crowdsourcing methods to collect qualitative data in addiction science: Narratives of non-medical prescription opioid, heroin, and fentanyl use. Int J Drug Policy 75, 102587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Administration (SAMHSA), 2019. Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. SAMHSA, Rockville, MD. [Google Scholar]
- Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, van der Goes DN, 2015. Rates of opioid misuse, abuse, and addiction in chronic pain: A systematic review and data synthesis. Pain 156(4), 569–576. 10.1097/01.j.pain.0000460357.01998.f1 [DOI] [PubMed] [Google Scholar]
- White H, 1980. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica 48, 817–830. http://www.jstor.com/stable/1912934 [Google Scholar]
- Wilson FA, Mosalpuria K, Stimpson JP, 2020. Association between opioid prescriptions and non-US-born status in the US. JAMA Netw Open 3(6), e206745. doi: 10.1001/jamanetworkopen.2020.6745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson N, Kariisa M, Seth P, Smith IV H, Davis NL, 2020. Drug and opioid-involved overdose deaths — United States, 2017–2018. MMWR Morb Mortal Wkly Rep 69(11), 290–297. 10.15585/mmwr.mm6911a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winship C, Morgan SL, 1999. The estimation of causal effects from observational data. Annu Rev Sociol 25, 659–706. 10.1146/annurev.soc.25.1.659 [DOI] [Google Scholar]


