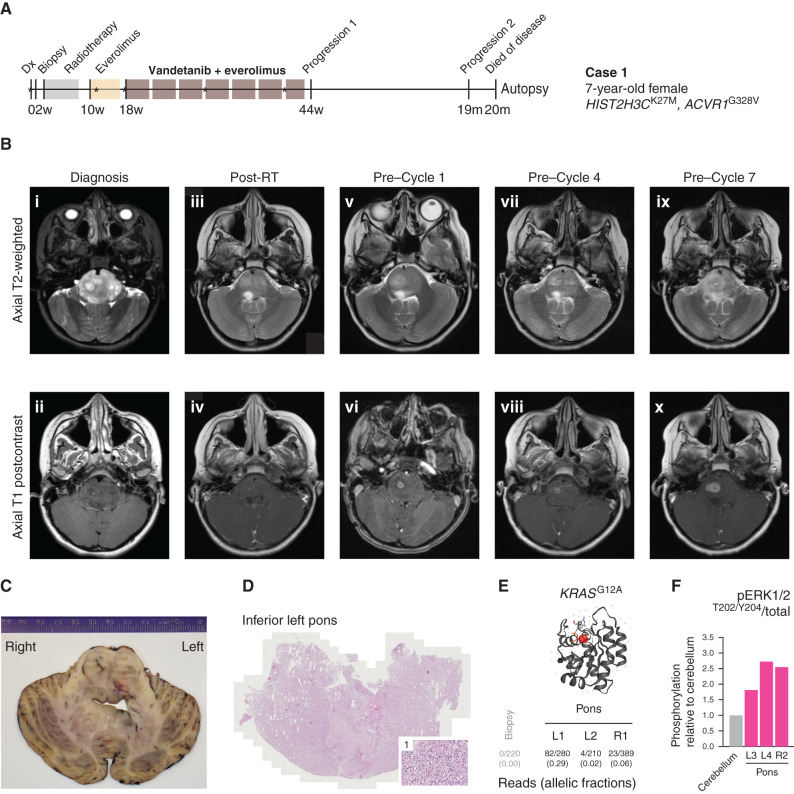
Figure 5.
Clinical experience of combined vandetanib and everolimus in a 7-year-old girl with ACVR1-mutant DIPG (case 1). A, Timeline summarizing the clinical history of case 1, treated at the Royal Marsden Hospital, London, United Kingdom. *Imaging scans presented in B. Dx, diagnosis. B, Sequential head MRI scans: diagnostic MRI showing diffuse heterogenous tumor infiltration and anatomic distortion of the pons, including partial invagination of the basilar artery (i) with a single focus of intratumoral enhancement in the right central pons (ii); MRI scan 6 weeks after radiotherapy (RT) showed considerable reduction in tumor infiltrative bulk (iii) with the small focus of enhancement persisting in the right pons (iv); the MRI scan after three cycles of everolimus single agent constituted also the baseline scan prior to starting vandetanib/everolimus, and it showed increased T2 signal abnormality in the right pons (v) associated with mildly increased focal enhancement (vi); the MRI scans after three cycles (vii, viii) and six cycles (ix, x) of vandetanib/everolimus showed modest enlargement and progressive infiltration of the right pons (vii, ix) with concomitant increase of the associated focal enhancement (viii, x) but nevertheless with relatively stable appearances/lack of progression elsewhere. The child started cycle 7 of vandetanib/everolimus but then developed worsening symptoms (slurred speech, ataxia), and treatment was permanently discontinued 11 months after initial diagnosis. No further systemic treatment or reirradiation was administered. The child could be weaned off steroids completely, and her balance and activity levels improved significantly. Eight months after discontinuation of vandetanib/everolimus, she developed further clinical and radiologic progression (local and metastatic) and died a month later (OS, 20 months). C, Macroscopic transverse cross section of pons and cerebellum from the brain autopsy specimen from case 1. D, Hematoxylin and eosin–stained image from the inferior left pons (×40), with a higher magnification inset (×200) of region 1, showing diffuse infiltration of tumor cells. E, Protein structure representation of KRAS showing mutant G12A residue (shaded red), generated in COSMIC-3D (https://cancer.sanger.ac.uk/cosmic3d/). Allelic fractions are provided for mutant reads identified in distinct areas of the pons taken at autopsy. F, MAPK pathway activation in distinct autopsy regions measured by quantitative capillary electrophoresis for phospho-ERK1/2T202/Y204, plotted as a ratio of respective phosphorylated/total protein compared with normal cerebellum.