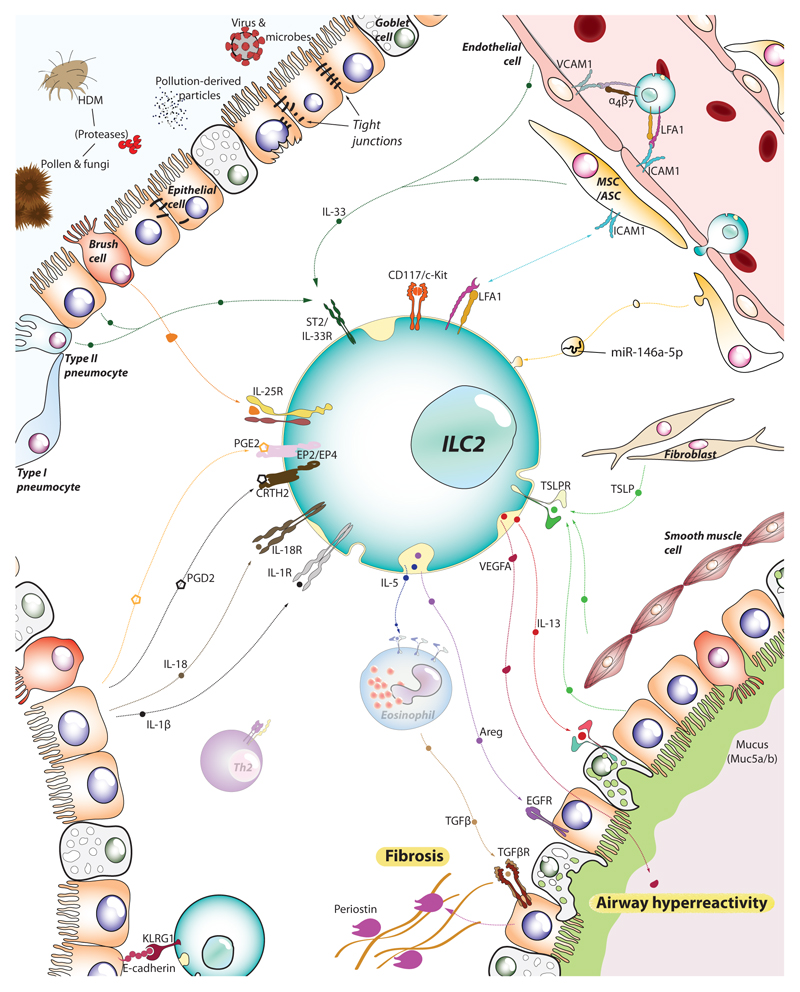
Figure 2.
ILC2s sense the tissue microenvironment and kick-off the type-2 immune response. As tissue resident lymphocytes, ILC2s are strategically positioned in the mucosal barrier sites, poised to monitor the release of alarmins by epithelial, endothelial and stromal cells. Epithelial cells, brush cells, multipotent and adventitial stromal cells (MSC/ASC) and pneumocytes (together with immune cells such as alveolar macrophages and dendritic cells) can detect allergens and irritants and, in turn, release IL-33, IL-25 and TSLP. Together with IL-1β and IL-18 liberated by dying cells, these alarmins stimulate ILC2s to secrete IL-5, IL-13, amphiregulin (Areg), and vascular endothelial factor A (VEGFA), that engage their respective receptors in epithelial cells, goblet cells and smooth muscle cells amongst others. The activation of these cells leads to airway hyperresponsiveness, mucus production and fibrosis, cardinal pathophysiological features of asthma and allergy. Endothelial cells also respond to the local inflammation and support further recruitment of ILC2s and other immune effector cells from the blood and distal tissues (e.g. intestine), boosting the inflammatory process.