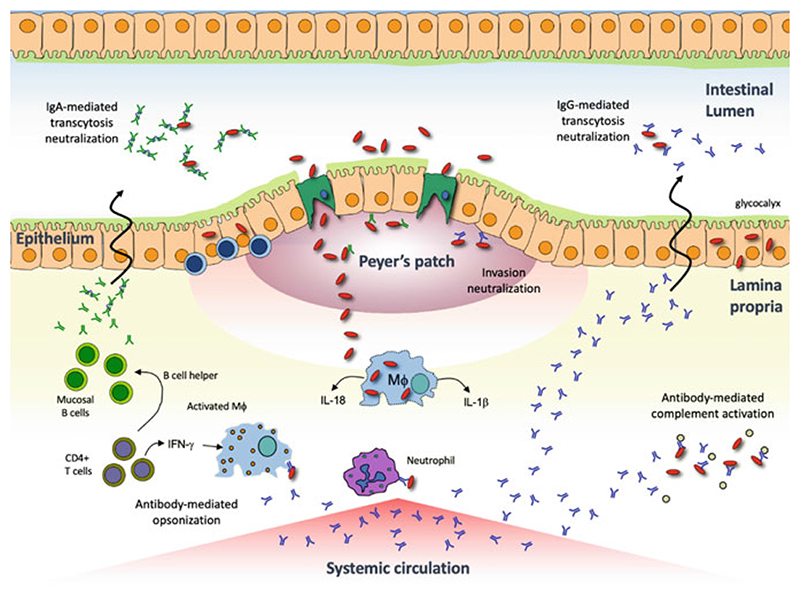
Fig. 2. Shigella pathogenesis and potential protective immune mechanisms.
Shigella is transmitted via the fecal-oral route and transits from the lumen into the lamina propria via M cells. Once in the basolateral space, Shigellae can induce pyroptosis in macrophages (MΦ) and utilize a type-III secretion system to translocate effector proteins (i.e., Ipa proteins) resulting in phagocytosis of the bacterium. Once intracellular, Shigellae multiply and spread to adjacent cells by reorganizing host cell actin polymerization. The intercellular bacterial spread and subsequent recruitment of neutrophils to the site of infection results in tissue destruction and the characteristic pathology of shigellosis. Although well-defined correlates of immunity have not been fully elucidated, protective immune responses may include neutralization of the bacteria in the gut lumen (prevention of M cell transit) or in the lamina propria (interference with host cell invasion), antibody-mediated complement activation (bacterial killing) and opsonization (marking bacteria for phagocytosis)